Abstract
Purpose
To determine the efficacy of mitomycin C in reducing the recurrence of anterior urethral stricture after internal optical urethrotomy (IOU).
Materials and Methods
This was a randomized controlled trial conducted in the Department of Urology at the Institute of Kidney Diseases Peshawar from March 2011 to December 2013. A total of 151 patients who completed the study were divided into two groups by the lottery method. Group A (cases) comprised 78 patients in whom mitomycin C 0.1% was injected submucosally in the stricture after conventional IOU. Group B (controls) comprised 73 patients in whom IOU only was performed. Self-clean intermittent catheterization was not offered in either group. All patients were regularly followed up for 18 months. Recurrence was diagnosed by use of retrograde urethrogram in all patients and flexible urethroscopy in selected cases. Data were collected on a structured pro forma sheet and were analyzed by SPSS.
Results
The mean age of the patients in group A was 37.31±10.1 years and that in group B was 40.1±11.4 years. Recurrence of urethral stricture was recorded in 11 patients (14.1%) in group A and in 27 patients (36.9%) in group B (p=0.002). The mitomycin group also showed a delay in recurrence compared with the control group (p=0.002).
Urethral stricture is a disease of antiquity. The earliest reference to urethral stricture can be traced to ancient Greek writings [1]. Hamilton Russell described the first surgical procedure of urethroplasty in 1914 (quoted from [2]). Sachse performed his first internal optical urethrotomy (IOU) in 1974 [3]. The exact incidence of stricture is unknown but it can be as high as 0.6% in some susceptible populations [45]. In Pakistan, the incidence of urethral stricture is around 3% to 4% [4].
There are several procedures for the management of urethral stricture, ranging from minimally invasive IOU to invasive modalities such as buccal mucosal graft urethroplasty and even tissue engineering in the 21st century. However, the greatest concern in urethral strictures is the high recurrence rate, which has culminated in the evolution of the common dictum that "once a stricture, always a stricture" [6].
IOU is the mainstay treatment modality in the management of urethral stricture. Being a minimally invasive procedure with less morbidity, it is commonly performed and is the procedure most favored by urologists around the globe [7]. Although the short-term success rate of optical urethrotomy is promised to be from 80% to 100% [89], the long-term efficacy of IOU is questionable, with a high recurrence rate in different studies ranging from 20% to 60% [1011].
Numerous techniques have been adopted to reduce the recurrence of stricture after IOU, such as prolonged catheterization and self-clean intermittent catheterization (SCIC) with varying success. Mitomycin C has antifibroblast and anticollagen properties and has been used in trabeculectomy, in myringotomy, and after keloid scar excision in contemporary surgical practice [121314].
In the present study, we explored the antifibroblast activity of mitomycin in preventing the recurrence of stricture after IOU with the aim of preventing this minimally invasive procedure from becoming obsolete. To the best of our knowledge, the present study is the first pilot study in Pakistan on this very important topic with the aim of determining the efficacy of mitomycin C in preventing recurrence of urethral stricture after IOU.
This was a randomized controlled trial conducted in the Department of Urology at the Institute of Kidney Diseases Hayatabad Medical Complex Peshawar, Pakistan, from March 2011 until December 2013. A total of 180 newly diagnosed cases of urethral stricture were included in the study. The study sample size was determined by use of software from the World Health Organization with the formula n=z2p(1-p)/d2. The sample was equally divided into two groups by the lottery method. Group A (cases) comprised 90 patients who were subjected to intralesional mitomycin C after IOU. Group B (controls) comprised 90 patients who underwent IOU only.
We included all patients with newly diagnosed anterior urethral stricture who completed the duration of the study and had urethral strictures of a maximum length of 2 cm, irrespective of etiology, according to the findings of a retrograde urethrogram supplemented by uroflowmetry. Patients with an maximal flow rate (MFR) of less than 12 mL/s and who underwent flexible urethroscopy were included in the study. We excluded patients with blind urethral strictures, multiple urethral strictures, urethrocutaneous fistula, recurrent stricture after failed IOU, and history of urethroplasty.
Permission was sought from the institutional research and ethics board, and a complete history, examination, and relevant investigations were completed in all patients. In group A, 0.1% mitomycin C was injected after IOU at the site in the 1, 11, and 12 o'clock positions with a TLA needle using a straight working channel pediatric cystoscope. In group B, IOU only was performed. SCIC was not offered in either group. Patients in both groups were regularly followed up for 18 months at 3 months, 6 months, 9 months, 12 months, and 18 months. The follow-up consisted of history, examination, and uroflowmetry every 3 months and retrograde urethrogram at 6, 12, and 18 months.
Values p<0.05 were considered significant in the analysis. The data were collected on a structured pro forma sheet and were analyzed by use of SPSS ver. 17 (SPSS Inc., Chicago, IL, USA).
Of the total 180 patients, 12 patients in group A and 17 patients in group B were lost to follow-up in the first 6 months and hence were dropped from the study. The sample was thus reduced to 151 patients who were divided into two groups. Group A (cases) comprised 78 patients who were subjected to intralesional mitomycin C after IOU. Group B (controls) comprised 73 patients who underwent IOU only.
The mean age of the patients in group A was 37.31±10.1 years and that in group B was 40.1±11.4 years (p=0.007). Regarding the etiology of urethral stricture, road traffic injury and iatrogenic urethral injury were the most common causes in both groups. Details on the different causes of stricture are shown in Fig. 1. The mean preoperative MFR in patients with symptoms of bladder outflow obstruction in 13 patients in group A was 11.5±5.1 mL/s, whereas it was 12.2±4.7 mL/s in 23 patients in group B. The mean stricture length in group A was 1.86±1.2 cm, whereas it was 1.67±1.4 cm in group B. No significant differences were observed in maximum flow or mean stricture length.
Urethral stricture can present in diverse clinical scenarios ranging from symptoms of bladder outflow obstruction like poor stream, straining, and intermittency to potentially fatal urosepsis and obstructive uropathy. The details of the clinical presentation in both groups are shown in Table 1. We included patients with strictures of only the anterior urethra; the split statistics for site of urethral involvement are shown in Fig. 2. Patients in both groups were regularly followed up for 18 months for evaluation of any recurrence, and the overall outcome in both groups is shown in Table 2. Regarding the association of recurrence with site, 8 patients in group A and 22 patients in group B had recurrence in the bulbar urethra, whereas 3 patients in group A and 5 patients in group B had recurrence in the penile urethra.
The timing of recurrence was also observed in our study in 38 patients, the details of which are shown in Table 3. As evident in the table, of the total 27 patients with recurrence in group B, 25 patients (92%) experienced recurrence within 6 months. In contrast, in group A, no recurrence was observed at 3 months, and 5 (45.5%), 4 (36.4%), 1 (9.1%), and 1 patient (9.1%) experienced recurrence at 6, 9, 12, and 18 months, respectively. The mean change in MFR in 102 men without recurrence in both groups was 18.9±11.7 mL/s versus 10.4±6.4 mL/s in 38 patients (p<0.001) who experienced recurrence.
No significant complications, such as necrosis of the urothelium, extravasation, or systemic absorption, were recorded in the mitomycin group.
Urethral stricture is a common ailment presenting to urologists around the globe. IOU is a minimally invasive, cost-effective procedure that is favored by the majority of urologists. A recent survey suggested that 86% of American urologists prefer IOU in the management of anterior urethral stricture [15]. The problem with the long-term success of IOU is recurrence of urethral stricture. Although several refinements have been introduced to minimize recurrence, such as repeated SCIC [16], recurrence has been labeled as a failure of the procedure itself by numerous authors [17]. Thus, we did not offer SCIC in either group to alleviate this bias. Study of the antifibroblast properties of initially steroids and later mitomycin C has opened new windows of research in different surgical disciplines. Intralesional mitomycin C has been proven to be effective in preventing fibrosis in myringotomy [1213], after excision of keloid scars in vivo, and in preventing urethral stricture in rats [14]. We have also found some encouraging results with intralesional mitomycin C in reducing the recurrence of urethral stricture.
A strength of our study was that it was a pioneer randomized controlled trial in Pakistan on the use of intralesional mitomycin. Moreover, our sample size and follow-up of 18 months makes this study comparable to international standards.
A weakness of the study was the unavailability of modern diagnostic tools in Pakistan, such as endoluminal magnetic resonance imaging or even high-frequency ultrasound for proper evaluation of thickness and hence grading of urethral stricture. Thus, we included all patients with urethral stricture of less than 2 cm on retrograde urethrogram.
Urethral stricture usually presents at an early age. The mean age of the patients in our study was almost 40 years, which agrees with the findings of Islam et al. [8] and Khan et al. [16], both of whom noted that urethral stricture usually occurs in patients older than 40 years. Historically, gonococcal urethritis was the most common etiology of urethral stricture, but currently trauma, both external and iatrogenic urethral trauma, is the most common cause [1618]. Our study also showed that road traffic accidents and iatrogenic injury were the most frequent causes of urethral stricture. One patient in our study had a stricture with an infective etiology; Stein et al. [19] also reported an infective etiology in 1% of cases in their study in 2013.
Regarding the location of urethral stricture, we found that 123 patients had bulbar urethral stricture followed by penile urethral stricture in 28 patients. This is because of the anatomical curve, which predisposes to bulbar urethral injury in iatrogenic and straddle urethral injury. Our observation agrees with the literature [8915].
Mitomycin C is an antitumor antibiotic isolated from Streptomyces caespitosus. It has been found to inhibit fibroblast proliferation and prevent scar formation [121314].
Mazdak et al. [20] introduced intralesional mitomycin C in 2007. He documented a 10% decreased rate of recurrence in the mitomycin group compared with a 50% rate of recurrence of stricture in the control group.
The observation of Mazdak was challenged by Mundy [21], who questioned his small sample size of 40 patients and shorter follow-up of 6 months. Both of these issues were properly addressed in our study, which had a sample size of 70 in each group and a follow-up period of 18 months. Our study showed a significant reduction in recurrence of stricture to 14.1% in the group with intralesional mitomycin versus 36.9% in the control group (p=0.001). In his review article, Vanni [22] also reported a significant reduction in recurrence of urethral stricture with intralesional mitomycin. Currently, a combination of antifibroblast agents containing mitomycin is being used with successful outcomes. Kumar et al. [23] recorded the recurrence of urethral stricture in only 20% of cases after intralesional injections. Another study by Chung [24] also showed positive results of recurrence in only 10% with intralesional injections.
Recently, intralesional triamcinolone after holmium laser optical urethrotomy has also shown promising results by reducing recurrence by 24% [25], which supplements our use of intralesional antifibroblast agents for successful reduction of recurrence of stricture after IOU. We have also documented that intralesional mitomycin C can prolong the timing of recurrence compared with a control group. Almost 92% of patients in the control group experienced recurrence of urethral stricture by 6 months, whereas a delay in recurrence was observed in 54% of patients in the mitomycin C group. Our observation agrees with the literature [20222325]. Significant improvement in uroflowmetry was observed in patients without recurrence in both groups. Erickson et al. [26] also mentioned significant improvement in the MFR after successful treatment of urethral stricture. We found no association of etiology, site, or size with recurrence in either group. This also agrees with the literature [826].
Our study has implications for all urologists who are involved in the management of urethral stricture. This novel technique of using intralesional mitomycin C has opened new windows of research for fellow urologists in urethral stricture disease. Further research is needed on the efficacy and safety of this novel technique.
Figures and Tables
Fig. 1
Bar graph showing different etiological factors in urethral stricture. Pearson chi-square=0.164.
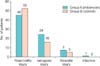
Table 1
Various clinical presentation in urethral stricture

Table 2
Main outcome in terms of rate of recurrence in both groups

| Group A (n=78) | Group B (n=73) | Total (n=151) | p-valuea) | |
|---|---|---|---|---|
| Recurrence | 11 (14.1) | 27 (36.9) | 38 (25.1) | 0.002 |
| No recurrence | 67 (85.8) | 46 (63.0) | 113 (74.8) |
Table 3
Timing of recurrence of urethral stricture (n=38)

References
1. Santucci RA, Joyce GF, Wise M. Male urethral stricture disease. J Urol. 2007; 177:1667–1674.
2. Mundy AR. Management of urethral strictures. Postgrad Med J. 2006; 82:489–493.
3. Sachse H. Treatment of urethral stricture: transurethral slit in view using sharp section. Fortschr Med. 1974; 92:12–15.
4. Zehri AA, Ather MH, Afshan Q. Predictors of recurrence of urethral stricture disease following optical urethrotomy. Int J Surg. 2009; 7:361–364.
5. Sangkum P, Levy J, Yafi FA, Hellstrom WJ. Erectile dysfunction in urethral stricture and pelvic fracture urethral injury patients: diagnosis, treatment, and outcomes. Andrology. 2015; 3:443–449.
6. Bazo A, Rao K. Urethral strictures: 'once a stricture, always a stricture'. Trop Doct. 2003; 33:69–71.
7. Heyns CF, van der Merwe J, Basson J, van der Merwe A. Treatment of male urethral strictures - possible reasons for the use of repeated dilatation or internal urethrotomy rather than urethroplasty. S Afr J Surg. 2012; 50:82–87.
8. Islam M, Anwar F, Ahmed S, Ali A. Optical urethrotomy in strictures following fracture pelvis. J Ayub Med Coll Abbottabad. 2010; 22:106–108.
9. Ali MN. Experience with cold knife optical internal urethrotomy. J Coll Physicians Surg Pak. 2001; 11:693.
10. Dubey D. The current role of direct vision internal urethrotomy and self-catheterization for anterior urethral strictures. Indian J Urol. 2011; 27:392–396.
11. Santucci R, Eisenberg L. Urethrotomy has a much lower success rate than previously reported. J Urol. 2010; 183:1859–1862.
12. Jampel HD. Effect of brief exposure to mitomycin C on viability and proliferation of cultured human Tenon's capsule fibroblasts. Ophthalmology. 1992; 99:1471–1476.
13. Yamamoto T, Varani J, Soong HK, Lichter PR. Effects of 5-fluorouracil and mitomycin C on cultured rabbit subconjunctival fibroblasts. Ophthalmology. 1990; 97:1204–1210.
14. Ayyildiz A, Nuhoglu B, Gulerkaya B, Caydere M, Ustun H, Germiyanoglu C, et al. Effect of intraurethral Mitomycin-C on healing and fibrosis in rats with experimentally induced urethral stricture. Int J Urol. 2004; 11:1122–1126.
15. Ferguson GG, Bullock TL, Anderson RE, Blalock RE, Brandes SB. Minimally invasive methods for bulbar urethral strictures: a survey of members of the American Urological Association. Urology. 2011; 78:701–706.
16. Khan S, Khan RA, Ullah A, ul Haq F, ur Rahman A, Durrani SN, et al. Role of clean intermittent self catheterisation (CISC) in the prevention of recurrent urethral strictures after internal optical urethrotomy. J Ayub Med Coll Abbottabad. 2011; 23:22–25.
17. Jackson MJ, Veeratterapillay R, Harding CK, Dorkin TJ. Intermittent self-dilatation for urethral stricture disease in males. Cochrane Database Syst Rev. 2014; 12:CD010258.
18. Xu YM, Song LJ, Wang KJ, Lin J, Sun G, Yue ZJ, et al. Changing trends in the causes and management of male urethral stricture disease in China: an observational descriptive study from 13 centres. BJU Int. 2014; 10. 07. [Epub]. DOI: 10.1111/bju.12945.
19. Stein DM, Thum DJ, Barbagli G, Kulkarni S, Sansalone S, Pardeshi A, et al. A geographic analysis of male urethral stricture aetiology and location. BJU Int. 2013; 112:830–834.
20. Mazdak H, Meshki I, Ghassami F. Effect of mitomycin C on anterior urethral stricture recurrence after internal urethrotomy. Eur Urol. 2007; 51:1089–1092.
21. Mundy AR. Adjuncts to visual internal urethrotomy to reduce the recurrence rate of anterior urethral strictures. Eur Urol. 2007; 51:1467–1468.
22. Vanni AJ. New frontiers in urethral reconstruction: injectables and alternative grafts. Transl Androl Urol. 2015; 4:84–91.
23. Kumar S, Garg N, Singh SK, Mandal AK. Efficacy of optical internal urethrotomy and intralesional injection of Vatsala-Santosh PGI tri-inject (triamcinolone, mitomycin c, and hyaluronidase) in the treatment of anterior urethral stricture. Adv Urol. 2014; 2014:192710.
24. Chung JH, Kang DH, Choi HY, Jeong TY, Ha US, Han JH, et al. The effects of hyaluronic acid and carboxymethylcellulose in preventing recurrence of urethral stricture after endoscopic internal urethrotomy: a multicenter, randomized controlled, single-blinded study. J Endourol. 2013; 27:756–762.
25. Kumar S, Kapoor A, Ganesamoni R, Nanjappa B, Sharma V, Mete UK. Efficacy of holmium laser urethrotomy in combination with intralesional triamcinolone in the treatment of anterior urethral stricture. Korean J Urol. 2012; 53:614–618.
26. Erickson BA, Breyer BN, McAninch JW. Changes in uroflowmetry maximum flow rates after urethral reconstructive surgery as a means to predict for stricture recurrence. J Urol. 2011; 186:1934–1937.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download