Abstract
Purpose
Urinary calculi is a familiar disease. A well-known complication of endourological treatment for impacted ureteral stones is the formation of ureteral strictures, which has been reported to occur in 14.2% to 24% of cases.
Materials and Methods
This was a prospective study. Ureterotripsy treatment was used on patients with impacted ureteral stones. Then, after 3 months and 6 months, the condition of these patients was assessed by means of a kidney-ureter-bladder (KUB) ultrasound. If the KUB ultrasound indicated moderate to serious hydronephrosis, the patient was further assessed by means of a computed tomography intravenous urogram or retrograde pyelogram to confirm the occurrence of ureteral strictures.
Results
Of the 77 patients who participated in the study, 5 developed ureteral strictures. Thus, the stricture rate was 7.8%. An analysis of the intraoperative risk factors including perforation of the ureter, damage to the mucous membrane, and residual stone impacted within the ureter mucosa revealed that none of these factors contributed significantly to the formation of the ureteric strictures. The stone-related risk factors that were taken into consideration were stone size, stone impaction site, and duration of impaction. These stone factors also did not contribute significantly to the formation of the ureteral strictures.
Go to : 
Urinary calculi is a globally prevalent disease. The introduction of improved endourological methods ensures that practically all such patients can be treated and their stones removed.
Ureteral calculi is an especially distressing condition, particularly in Malaysia, because patients often present with a large burden of calculi that are impacted into the ureteral mucosa. The formation of ureteral strictures is a potential complication of the treatment of such patients [1,2,3]. The persistent irritation caused by impaction can result in epithelial hypertrophy and edema, thus rendering the patient vulnerable to fibrosis and stricture formation [4]. The removal of stones by means of endourological methods may lead to mechanical insult and increased risk. This happens even with recent innovations, such as the latest ureteroscopes, which come with smaller diameters, and the latest techniques for shattering stones by use of a Holmium laser [4,5].
Shock wave lithotripsy (SWL) is one method of treatment. However, impacted upper ureteral stones are more resistant to shock wave disintegration, owing to the lack of space to expand when the stones are battered by the shock waves [6]. Pre-SWL stenting provides no additional benefit over in situ SWL [6]. One study showed that ureterolithotripsy achieved better outcomes than did SWL for proximal ureteral stones bigger than 1 cm [7].
Not many studies have been carried out to ascertain the occurrence and the factors that cause stricture f ormation in patients who undergo endourologic treatment for impacted ureteral calculi. Retrospective studies have revealed that ureteric perforation is related to a high rate of stricture formation (90%-95%) [1,2,3]. The edematous ureter is likely to perforate even when a gentle procedure is performed [4]. Damage to the ureteric mucosa can also trigger stricture formation. Fibrinous exudates produced by the mucosa precipitate onto the injured area, stimulating adherence and, finally, stricture formation [1]. The limited working space as a consequence of ureteral edema increases the chances of damage to the mucous membrane while the stones are being fragmented. Furthermore, Dretler and Young [8] discovered a massive cell reaction to a foreign body around the calcium oxalate crystals at the location of strictures in patients who went through stone fragmentation prior to extraction. Fragments of calculi embedded in the ureteral mucosa can trigger inflammation that can lead to stricture formation [9]. In a few studies, strictures eventually developed at the site where leftover stone fragments were found [8,10]. Prolonged irritation due to ureteral calculi is an important factor in the formation of ureteral lesions [11]. Ischemia, resulting from persistent pressure or from an immunological reaction to the stone materials, may give rise to ureteral edema and fibrosis [9]. Yamaguchi et al. [11] noticed two types of microscopic features in ureteral lesions linked to impacted stones. They deduced that the length of time that the stones are present is a probable factor contributing to the development of ureteral lesions.
In a retrospective study, Roberts et al. [1] reported an incidence rate of 24% for ureteral strictures after an average follow-up of 7 months following removal of stones by endoscopy. Brito et al. [3] also obtained a stricture incidence rate of 14.2% among 42 patients who underwent treatment f or impacted ureteric stones. A larger multicenter study conducted in 1999 reported an incidence rate of 19% for stricture formation, with the risk factors being ureteral perforation and the lodging of leftover fragments in the mucous membrane [2]. So far, there has been no publication of any potential randomized study.
Go to : 
This was a prospective study. This study was approved by University Kebangsaan Malaysia (project code: FF-297-2010). A sample population was selected from among patients who were examined at the Urology Clinic of the University Kebangsaan Malaysia Medical Centre from May 2010 to November 2012. All patients in the sample population had undergone ureterolithotripsy treatment for ureteral calculi.
Computed tomography urogram was performed for all patients for diagnosis and assessment of the stone. To fit the definition of impacted calculi, at least one of the following criteria had to be met: (1) difficulty encountered in passing a standard guidewire or ureteral catheter past the level of the calculi at the first attempt [5]; (2) moderate to severe hydronephrosis experienced beyond the level of the calculi owing to its presence [6,9]; (3) calculi immobile at the same location for a minimum of 2 months [1].
In this study, retrograde rigid ureteroscopy was used to remove the impacted stones and a Holmium laser was used to assist in the fragmentation of the stones. The operations were performed by three certified urologists in our center. A 365-µ laser fiber was used with frequency set at 8 Hz and energy set at 800 mJ for all cases.
The stones were removed by means of a ureteroscope according to the method recommended by Gerber and Lyon [12]. A guidewire was inserted into the vesicoureteric orifice and was pushed up the ureter. A 6.5-Fr rigid ureteroscope was inserted until it reached the level of the calculi. A Holmium laser was used to facilitate fragmentation. A 2.2-Fr grasper or nitinol basket was used to remove the fragments. As usual, a 6-Fr ureteral stent was fixed at the site for 3 to 4 weeks after the operation. In cases in which difficulty was experienced at the first attempt, a ureteral stent was left in position for 2 to 4 weeks, after which a second attempt was made to remove the stone. After the operation, the surgeon analyzed and recorded signs of any intraoperative risk factors including perforation of the ureter, damage to the mucous membrane, and leftover stones lodged within the ureter mucosa. The patients were also monitored for risk factors with regard to stone size, location of stone impaction, and period of impaction.
A kidney-ureter-bladder (KUB) ultrasound was used to assess the patients at 3 months and 6 months. When the KUB ultrasound showed moderate to severe hydronephrosis, a computed tomography intravenous urogram (CT-IVU) was used for further assessment of the patients to confirm the formation of ureteric strictures. A ureteral stricture was described as a principal narrowing of the ureter at the place where stone impaction occurred earlier, with a CT-IVU indicating moderate to gross hydroureteronephrosis. Retrograde pyelography (RPG) was performed on those patients who were contraindicated for CT-IVU and whose blockage in the ureter could not be clearly detected by a CT-IVU.
Those patients who were unfit for general anaesthesia, who declined to undergo endoscopic treatment for their ureteral calculi, who had undergone endoscopic treatment for ureteral calculi earlier at the same site in the ureter as the current stone, or who had previously undergone radiotherapy to the pelvic or abdominal area were excluded from this study.
Data analysis was performed by using SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA). Risk factors for ureteral perforation were analyzed with multiple logistic regression.
Go to : 
Results were obtained from 77 patients during the course of the 2-year study. All patients were treated for impacted ureteral stones by means of retrograde ureterolithotripsy. Thirteen patients were excluded from the study, nine for noncompliance with follow-up procedures and four who required secondary intervention for ureteral obstruction owing to incomplete stone removal.
Five of the 64 patients remaining in the analysis developed ureteral strictures with a stricture formation rate of 7.8%. Strictures were detected in four of these patients 3 months after the CT-IVU and in one patient 6 months after surgery.
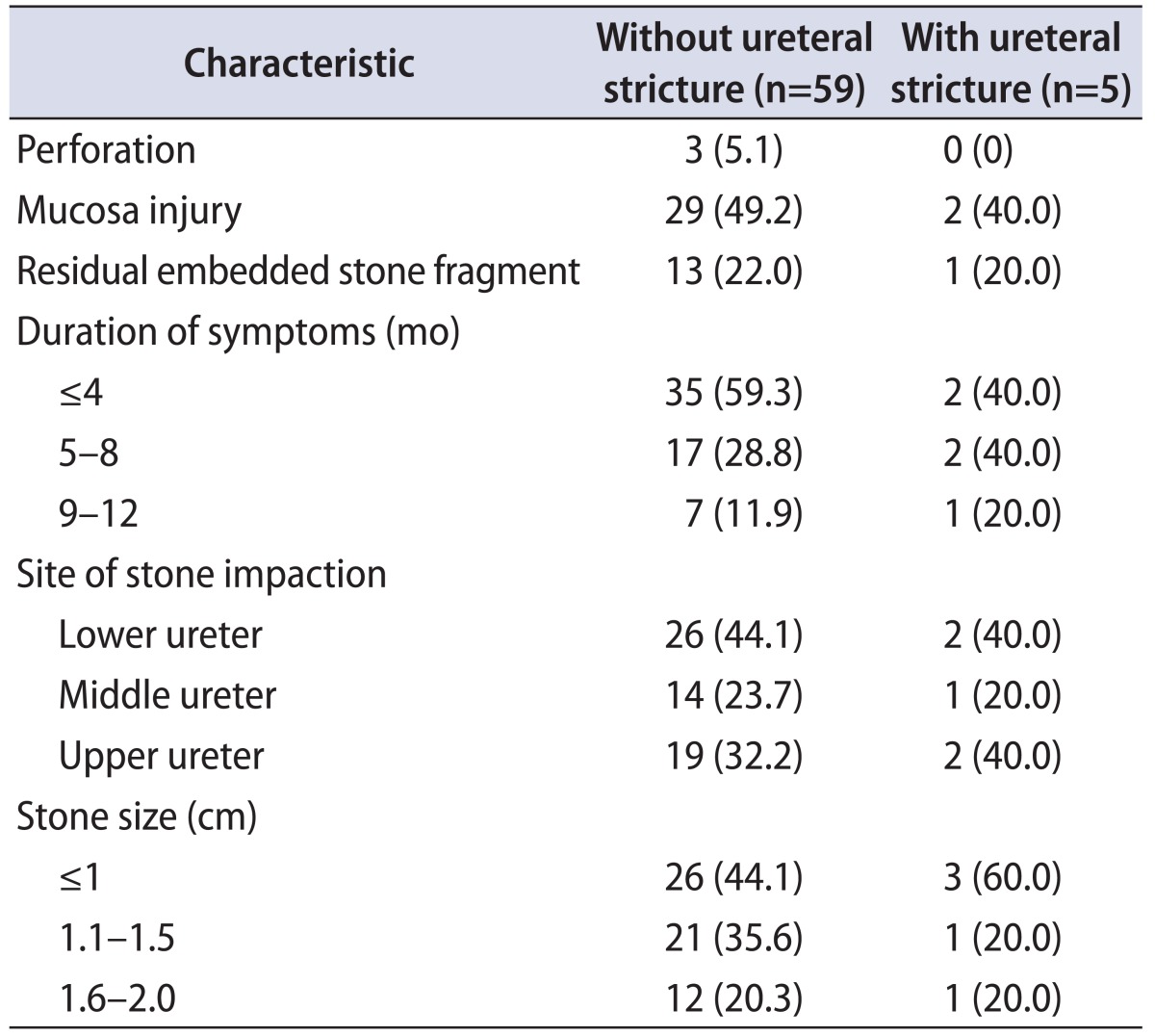
As mentioned above, three criteria were used to define the impacted ureteral stones. Fourteen patients were diagnosed with impacted ureteral stones on the basis of criterion 1, a total of 50 patients were diagnosed on the basis of criterion 2, and 36 patients were diagnosed on the basis of criterion 3. Thirty-one patients were diagnosed with impacted ureteral stones on the basis of two criteria, whereas only three patients were diagnosed on the basis of all three criteria. Table 1 lists the characteristics of the patients and the risk factors. Of the patients who ended up with ureteral strictures, two patients had been diagnosed with impacted ureteral stones on the basis of criteria 2 and 3, two patients had been diagnosed on the basis of criterion 3, and one patient had been diagnosed on the basis of criterion 2.
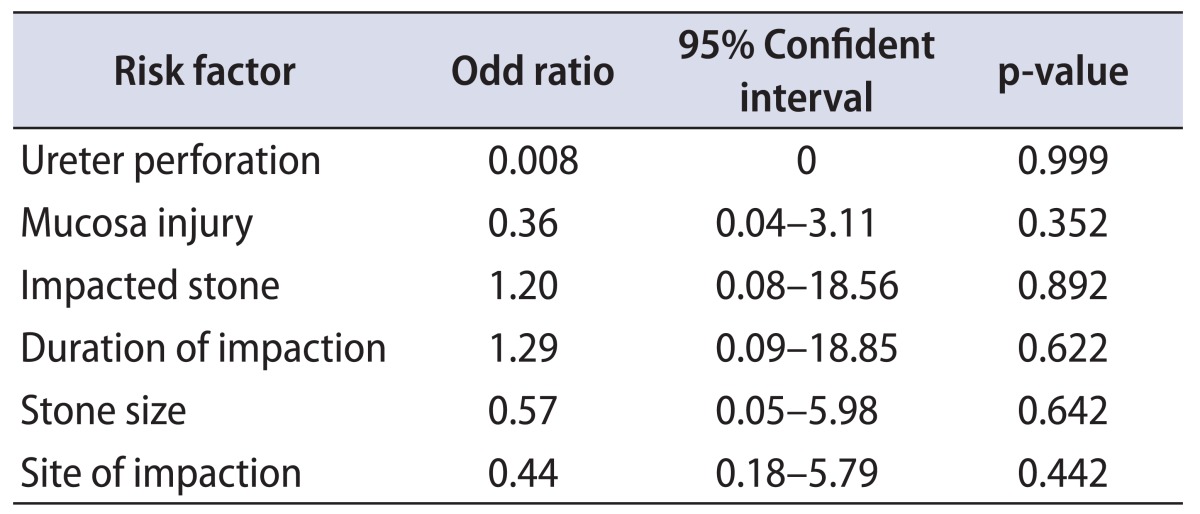
A separate analysis was carried out on the intraoperative risk factors for the formation of strictures, namely, for perforation of the ureter, damage to the membrane, and leftover stones lodged within the ureter mucosa. The analysis indicated that none of these factors contributed significantly to the formation of ureteric strictures. In addition, the formation of ureteric strictures was not caused significantly by the presence of more than one intraoperative risk factor (Table 2).
The stone-related risk factors that were taken into consideration were stone size, site of stone impaction, and period of impaction. The largest stone burden in this study had a diameter of 3 cm, and the longest period of impaction was 12 months. Out of 13 patients who had stone sizes larger than 1.5 cm, only 1 patient developed ureteral strictures after surgery. Out of eight patients with ureteral stone impaction for a period of more than 9 months, only one patient developed ureteral strictures after surgery. It was shown by statistical analysis that none of these three stone factors contributed significantly to the formation of ureteral strictures (Table 2).
Of the five patients with ureteral strictures after ureterotripsy treatment, one was diagnosed by means of an RPG 6 months after surgery. Although a KUB ultrasound done on this patient at 3 months and 6 months following the ureterotripsy indicated moderate hydronephrosis of the ipsilateral kidney, a CT-IVU failed to detect the presence of ureteral strictures. Following that, an RPG showed the presence of a stricture in the middle left side of the ureter.
Go to : 
Previous research into the rate of stricture formation following endoscopic treatment for impacted stones reported stricture rates of between 14.2% and 24% [1,3]. Retrospective methods were used in all these studies and fewer patients were involved than in the present study (n=24 and n=42). In this prospective study, the rate of formation of ureteral strictures following ureterotripsy for impacted stones was 7.8%, which was lower than the rates in earlier studies.
In the above studies with higher stricture rates [1,2], ureteroscopes with larger diameters ranging from 8.5 Fr to 10 Fr were used, and these may have been partly responsible for the damage to the ureter during treatment. By contrast, a 6.5-Fr ureteroscope was used in our study. Furthermore, the majority of ureteral stricture formation in the previous studies was associated with ureteral perforation. The study by Brito et al. [3] indicated that 75% of patients with ureteral perforation subsequently developed ureteral strictures, whereas Roberts et al. [1] revealed that 4 of 5 patients (80%) with ureteral perforation developed strictures [3]. In this study, three patients suffered iatrogenic perforation by the hydrophilic guidewire during a procedure for the insertion of a stent. However, follow-up examination revealed that none of these patients developed ureteral strictures, thus contradicting the results from the earlier above-mentioned studies. It is believed that guidewires only cause tiny perforations that mainly heal without forming any strictures. Ureteral perforation was not a risk for ureteral formation in this study, and it was also one of the reasons the stricture rate was lower in this study.
Dretler and Young [8] pointed to lef tover stone fragments lodged in the ureter mucosa as the cause of stricture formation. According to them, these stone fragments induce an inflammatory reaction that leads to stricture formation. Robert et al. [2] agreed that this was a risk factor for ureteral stricture formation. In the current study, out of 14 patients identified with residual embedded stone fragments following ureteroscopy, only 1 patient developed stricture formation as a result of embedded stones. Hence, a statistical analysis showed there was no significant relationship between the formation of ureteral strictures and lodged stone fragments.
Ureteral stones cause persistent irritation that leads to edema and fibrosis in the ureter mucosa. Microscopic studies have shown the occurrence of chronic interstitial fibrosis and urothelial hypertrophy at the stone impaction area. Decreased blood flow due to prolonged physical pressure or an immunological response toward stone material causes severe and chronic inflammation at the ureter mucosa [4,5,8]. Greater pressure is exerted at the impact site by larger stones and a longer period of impaction, thus increasing the risk of stricture formation. However, in the case of this study, the patients with ureteral stricture were not necessarily storing bigger stones or had not necessarily undergone a longer period of stone impaction. It was shown through analysis that neither the period of impaction nor the stone size was a risk factor for ureteral stricture formation. It is believed that besides a large-sized stone, the position of the stone in the ureter is important for stricture formation. The greatest pressure to the ureter mucosa is exerted by stones with larger transverse diameters (as measured by axial CT scans), which extend across the lumen of the ureter, thus resulting in ischemia and eventually stricture formation. A large stone size recorded in terms of its vertical length or its total volume may not have a significant effect on ureteral stricture formation.
During ureteroscope, it was noted that the endoscopic images of eight patients showed lesions resembling strictures next to the area of impaction. The lesions were edematous hemispheres without villi, thus resulting in a considerable reduction in the intraluminal diameter. The same type of lesions was detected in 28 patients in a study by Mugiya et al. [10]. Because of these lesions it was difficult to get a good view of the stone and its ensuing fragmentation. These lesions were thought to be indications of permanent ureteral strictures. However, KUB ultrasounds done on these patients did not show any signs of hydronephrosis. From these findings, it can be gathered that the stricture-like lesions that were discovered endoscopically were mainly due to excessive fluid in the mucous membrane. There is no possibility of permanent damage because these lesions have no fibrotic component. Hence, the ureteral lumen will return to normal once the edema has been treated.
According to this study, it is hypothesized that ureteral strictures will be formed within 3 months after patients have undergone ureterolithotripsy treatment. Four of five patients were diagnosed with ureteral strictures at 3 months according to a CT-IVU. The last patient was diagnosed at 6 months according to RPG after CT-IVU failed to demonstrate ureteral stricture. KUB ultrasound performed on this patient showed moderate hydronephrosis 3 months after ureterolithotripsy. Thus, it was assumed that the ureteral stricture had formed then.
None of the patients with ureteral strictures displayed symptoms during the follow-up. Their renal profiles showed no abnormality. This is a silent disease which cannot be easily detected clinically or biochemically. When moderate hydronephrosis is detected in an ultrasound, it is a good indicator that there is some abnormality in the ureter. According to the results of the present study, 75% of the patients with moderate hydronephrosis had a blockage in the ureter due to either a stricture or a residual stone.
According to the formula by Kish [13] for sample size calculation , we needed 100 patients to achieve test power of 80%. We only collected 64 samples in a duration of 2 years, which is a limitation of this study. We acknowledge that despite the insignificance of all the risk factors, a large sample size might change the results. A larger multiinstitutional collaboration study should be carried out to achieve a good sample size.
Go to : 
The rate of formation of ureteral stricture following endoscopic treatment for impacted ureteral stones is 7.8%, which is much lower than reported earlier. However, this is still a warning sign to urologists. This prospective study failed to identify any factors for predicting the formation of ureteral strictures. Because this is a silent disease that can result in unilateral damage to the kidneys, it is recommended that a simple KUB ultrasound examination be conducted on patients 3 months after they have undergone endoscopic treatment for impacted ureteral stones.
Go to : 
References
1. Roberts WW, Cadeddu JA, Micali S, Kavoussi LR, Moore RG. Ureteral stricture formation after removal of impacted calculi. J Urol. 1998; 159:723–726. PMID: 9474134.

2. Robert WW, Caddedu JA, Fabrizio MD, Jarrett TW, Kavoussi LR, Moran ME, et al. Ureteral stricture formation following removal of impacted calculi. J Urol. 1999; 161(Suppl):376.
3. Brito AH, Mitre AI, Srougi M. Ureteroscopic pneumatic lithotripsy of impacted ureteral calculi. Int Braz J Urol. 2006; 32:295–299. PMID: 16813672.

4. Morgentaler A, Bridge SS, Dretler SP. Management of the impacted ureteral calculus. J Urol. 1990; 143:263–266. PMID: 1967657.

5. el-Sherif AE. Endoscopic management of impacted stones in the intramural or meatal part of the ureter without performing meatotomy. Br J Urol. 1995; 76:394–396. PMID: 7551856.

6. Ghoneim IA, El-Ghoneimy MN, El-Naggar AE, Hammoud KM, El-Gammal MY, Morsi AA. Extracorporeal shock wave lithotripsy in impacted upper ureteral stones: a prospective randomized comparison between stented and non-stented techniques. Urology. 2010; 75:45–50. PMID: 19811806.

7. Wu CF, Shee JJ, Lin WY, Lin CL, Chen CS. Comparison between extracorporeal shock wave lithotripsy and semirigid ureterorenoscope with holmium:YAG laser lithotripsy for treating large proximal ureteral stones. J Urol. 2004; 172(5 Pt 1):1899–1902. PMID: 15540749.
8. Dretler SP, Young RH. Stone granuloma: a cause of ureteral stricture. J Urol. 1993; 150:1800–1802. PMID: 8230508.

9. Devarajan R, Ashraf M, Beck RO, Lemberger RJ, Taylor MC. Holmium: YAG lasertripsy for ureteric calculi: an experience of 300 procedures. Br J Urol. 1998; 82:342–347. PMID: 9772868.
10. Mugiya S, Ito T, Maruyama S, Hadano S, Nagae H. Endoscopic features of impacted ureteral stones. J Urol. 2004; 171:89–91. PMID: 14665851.

11. Yamaguchi K, Minei S, Yamazaki T, Kaya H, Okada K. Characterization of ureteral lesions associated with impacted stones. Int J Urol. 1999; 6:281–285. PMID: 10404303.

12. Gerber GS, Lyon ES. Treatment of ureteral stones. In : Smith AD, editor. Smith's textbook of endourology. St. Louis: Quality Medical Publishing Inc.;1996. p. 455–462.
13. Kish L. Survey sampling. New York: John Wiley & Sons Inc.;1965.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download