Abstract
Since its initial introduction in 1976, percutaneous nephrolithotomy (PCNL) has been widely performed for the management of large renal stones and currently is recommended for staghorn calculi, kidney stones larger than 2 cm, and shock wave lithotripsy-resistant lower pole stones greater than 1 cm. However, except for open and laparoscopic surgery, PCNL is the most invasive of the minimally invasive stone surgery techniques. Over the years, technical and instrumental advances have been made in PCNL to reduce morbidity and improve effectiveness. A thorough review of the recent literature identified five major areas of progress for the advancement of PCNL: patient positioning, method of percutaneous access, development of lithotriptors, miniaturized access tracts, and postoperative nephrostomy tube management. This review provides an overview of recent advancements in PCNL and the outcomes of each area of progress and notes how much we achieve with less invasive PCNL. This information may allow us to consider the future role and future developments of PCNL.
The incidence of kidney stones has been increasing in Korea with the rise in dietary and lifestyle changes influenced by Western countries. Nephrolithiasis is one of the common causes of morbidity and deterioration of quality of life in the United States, with a lifetime prevalence of 5% to 10% [1]. In addition, urolithiasis is a recurrent disease, with lifetime recurrence risks reported to be as high as 50% [2]. Given this high incidence and recurrence, technological advances have been made to dramatically improve minimally invasive techniques for the management of kidney stones, such as percutaneous nephrolithotomy (PCNL), extracorporeal shock wave lithotripsy (ESWL), and retrograde intrarenal surgery (RIRS). Although ESWL and RIRS are currently widely used as less-invasive treatment modalities for renal stones, PCNL still has a role depending on the size, position, shape, and composition of the stones [3]. PCNL is recommended as the treatment of choice for large renal stones (>20 mm) and for lower calyceal stones sized 10 to 20 mm with unfavorable factors for ESWL according to updated European Association of Urology guidelines [4]. Since its initial introduction in 1976 by Fernstrom and Johansson, PCNL has been widely performed for the management of large and complex renal stones and it remains the gold standard approach for difficult-to-treat renal stones (staghorn calculi, hard stones, stones associated with abnormal renal anatomy, and stones that have failed treatment with other less-invasive methods) [56789]. However, although PCNL is considered as a minimally invasive procedure for stone removal, it is still a challenging surgical technique and can be associated with critical complications such as bleeding and septicemia. In addition, as the indications for RIRS have expanded, it has supplanted ESWL and PCNL for the treatment of some renal stones. Nevertheless, many efforts have been made to reduce morbidity and increase the efficiency and effectiveness of PCNL (Table 1), because PCNL remains indicated as a first-line treatment for many cases. Herein, recent advancements in PCNL in surgical technique, instrumentation, and perioperative care are reviewed from the current literature.
Traditionally, PCNL has been performed with the patient in a prone position, and retrograde ureteral catheter placement is usually performed in the dorsal lithotomy position before the main lithotripsy procedure. The prone position provides a larger surface area for the choice of puncture site, including upper pole puncture, a wider space for manipulating the nephroscope and lithotriptors, and a lower risk of other perirenal visceral injury [10]. However, there are also disadvantages to performing PCNL in a traditional prone position, such as patient discomfort, a relatively longer overall operation time owing to repositioning, and anesthesiological risks including circulatory problems, ventilatory difficulties, suboptimal airway control, increased sympathetic activity, ocular and pharmacokinetic effects, and possible lesions of the cervical spine or peripheral nerves. Moreover, repositioning of the anesthetized patient is inevitable for retrograde access if it is needed, and this can lead to wasted time and increased risk of iatrogenic articular and peripheral nerve inadvertent pressure injury[11121314]. To overcome these limitations, various modifications of patient positioning have been proposed over the years.
The prone split-leg position was introduced as a modification of standard prone PCNL to increase efficiency and reduce the operation time [15]. This position obviously decreases the operation time and the need for operative staff for multiple patient transfers, but it still has disadvantages related to anesthesiological risks. Another modification of the prone position is the prone-flexed position [16]. This position provides a larger surface area and wider working space. The distance from the posterior iliac crest to the 12th rib is reported to be increased by 2.9 cm with the prone-flexed position compared with the standard prone position [16]. This means that this position has an advantage for easier access to upper pole puncture. Although standard and modified prone positions have been successfully performed, they still have drawbacks related to increased cardiopulmonary risks. In particular, obese patients and those with cardiopulmonary comorbidities may have increased risks of cardiopulmonary-related complications for long operations in the prone position. To overcome these drawbacks, supine PCNL was introduced.
Since Valdivia et al. [14] first performed supine PCNL in 1987, several studies have reported favorable outcomes and the technical benefits of this technique [171819202122232425]. A recent systemic review and meta-analysis comparing supine and prone PCNL reported a shorter operation time in supine PCNL and similar complication and transfusion rates between supine and prone PCNL [2325]. Theoretically and practically, the advantages of supine PCNL compared with standard prone PCNL are as follows: (1) optimal cardiovascular and airway control, (2) better in high-risk patients with heart failure or in obese patients, (3) shorter operation time due to no need for repositioning, (4) opportunity for a combined retrograde approach, (5) better stone fragment washout due to horizontal dorsal sheath angle, and (6) less radiation exposure to the surgeons' hands. However, supine PCNL also has several limitations, as follows: (1) limited space for renal puncture and nephroscope mobility (Fig. 1); (2) upper pole calyx puncture is more challenging; (3) more complex tract dilation due to high kidney mobility; (4) increased risk of spleen and liver injury during upper pole puncture; (5) decreased filling of the collecting system, which is constantly collapsed; and (6) spinal interposition in the fluoroscopic field during anteroposterior projections [1113262728].
In addition to supine PCNL, various modified positions have recently been proposed, such as supine oblique [29], semisupine [30], lateral decubitus [31], split-leg modified lateral [32], flank [33], and flank prone position [34]. The advantage of these positions is the possibility for simultaneous antegrade and retrograde access to the kidney without repositioning. However, there are still limited studies available to validate the efficacy and safety of PCNL in these various positions, including supine PCNL. Therefore, a large, prospective, multicenter, randomized controlled trial is necessary to verify the feasibility and safety of PCNL in modified positions.
One of the most important steps for successful PCNL is well-placed access into the kidney. Traditionally, intraoperative percutaneous access was most commonly performed by use of fluoroscopic guidance. However, this approach has some drawbacks, including increased radiation exposure for the surgeon, operating room staff, and patient, and possible iatrogenic visceral injury such as to the colon, liver, spleen, and pleura. Moreover, it is hard to perform fluoroscopic-guided access in patients in whom retrograde ureteral catheter placement is difficult or impossible, such as in patients with urinary diversions or renal transplants.
To overcome these limitations of fluoroscopy, an alternative is ultrasound-guided percutaneous access. The advantages of this approach are less radiation exposure and the ability to identify nearby organs. Several studies have reported satisfactory outcomes and fewer complications with ultrasound-guided access compared with fluoroscopic-guided access [35363738]. According to these studies, the success rate in the targeted calyces of ultrasound- and fluoroscopic-guided access ranges from 90% to 100% and from 96% to 100%, respectively. Visceral injury was not reported in these studies. Basiri et al. [35] reported intraoperative bleeding rates of 10% (5 of 50) in an ultrasound-guided access group and 6% (3 of 50) in a fluoroscopic-guided access group (p=0.5). However, ultrasound-guided access is surgeon-dependent and has some limitations for delineating fine details of the renal anatomy, especially in patients with nondilated collecting systems or in obese patients [39]. In this condition, my preference for percutaneous access is a combined approach using ultrasound and fluoroscopic guidance simultaneously. With fluoroscopic guidance, I can easily focus on the targeted calyx, and then percutaneous access can be performed by using ultrasound guidance, resulting in less radiation exposure and reducing the risk of nearby organ injury. Moreover, large branches of the renal artery can be identified by using the Doppler ultrasound setting, which may reduce the risk of bleeding by avoiding punctures to that area.
If the patients have a collecting system that is difficult to access or a spinal deformity such as spina bifida or scoliosis, fluoroscopic-guided access can cause adjacent organ injury and may not guarantee successful PCNL. In these situations, computed tomography (CT)-guided percutaneous access can be a good alternative [27]. Matlaga et al. [40] reported six cases of CT-guided access due to spinal deformity, retrorenal colon, or transplanted kidney and showed favorable outcomes. They reported that percutaneous access was achieved successfully without complications in all cases and the stone-free rate was 83% (5 of 6).
Because fluoroscopic-guided or CT-guided access can have concerns related to ionizing radiation exposure, and ultrasound-guided access may obscure fine details of the renal anatomy, magnetic resonance imaging (MRI)-guided access has been introduced as an alternative means of nonionizing radiation [41]. Kariniemi et al. [42] performed percutaneous access using open-configuration, C-arm shaped MRI and reported success in seven of eight patients. They demonstrated that a drawback of this approach is difficulty visualizing the guidewire with MRI. Besides, the need for specially designed equipment to perform this technique can also be an obstacle to widespread use of MRI-guided access.
In addition to these various imaging-guided access methods, the development of endoscopy such as flexible ureteroscopy and optical puncture systems has introduced modified techniques for safe and desirable access. Lawson et al. [43] and Hunter et al. [44] used a retrograde approach that can be applied by directing a steerable catheter in a retrograde fashion into the desired calyx and then advancing a puncture wire out through the catheter to the skin. Grasso et al. [45] and Kidd and Conlin [46] reported simultaneous retrograde ureteroscopic and fluoroscopic-guided percutaneous access. Bader et al. [47] reported successful use of an optical puncture needle named an "allseeing needle" to confirm the optimal percutaneous access.
After successful percutaneous access and tract dilatation, efficient stone fragmentation and evacuation depend on the effectiveness of the lithotriptors. Traditionally, ultrasonic and pneumatic lithotriptors have been most commonly used for PCNL. Ultrasonic lithotriptors can effectively fragment most stones except very hard stones, such as cystine or calcium oxalate monohydrate stones, and can simultaneously aspirate stone fragments [48]. Pneumatic lithotriptors can fragment hard stones more efficiently than ultrasonic lithotriptors but have no or limited suctioning function [49].
To combine the characteristics of both ultrasonic and pneumatic lithotriptors, dual-modality devices, such as the Swiss LithoClast Ultra (Boston Scientific Corp., Natick, MA, USA) and the CyberWand dual ultrasonic lithotriptor (Gyrus ACMI, Southborough, MA, USA) have been developed that provide efficient stone fragmentation with concomitant aspiration [5051]. Pietrow et al. [52] performed a randomized controlled study comparing the Swiss LithoClast Ultra with a standard ultrasonic lithotriptor and demonstrated a better stone clearance rate (40 mm2/min vs. 17 mm2/min, p=0.028) and shorter mean time to stone clearance (21 minutes vs. 44 minutes, p=0.036) with the Swiss LithoClast Ultra. However, another multicenter randomized clinical trial showed no advantage of the CyberWand dual ultrasonic lithotriptor compared with a single-probe ultrasonic lithotriptor with regard to time to stone clearance, stone-free rate, and complication rate [53]. Another new device is the holmium: yttrium aluminium garnet (YAG) laser. This device can be used alone or in combination with an ultrasound lithotriptor. The vaporizing and bursting effect of the holmium:YAG laser can fragment the stone quickly regardless of stone composition; therefore, it may reduce the lithotripsy and operation time [5455]. Recently, a cordless lithotripsy device, the LMA stone Breaker Pneumatic Lithotripter (Cook Medical, Bloomington, IN, USA), was developed. The advantage of this device is that it is portable and can generate high velocity at the probe tip, but no clinical trials have compared the efficiency and safety of this device with those of other lithotriptors [56].
Standard PCNL is usually performed through 24- to 30-Fr percutaneous tracts. Recently, several reports have suggested that the risk of bleeding is associated with sheath size [5758]. Thus, to decrease morbidity related to larger tracts, such as bleeding, postoperative pain, and potential renal damage, modifications to technique and the size of the instruments have been made. This technique of using a small caliber working sheath, known as mini-PCNL or miniperc, was originally developed for the management of large renal stones in pediatric patients. Helal et al. [59] first reported miniaturized PCNL for 2-year-old pediatric patients with renal stones with the use of a 15-Fr peel-away vascular sheath. Then, Jackman et al. [60] accomplished mini-PCNL using an 11-Fr access sheath. In their series, the mean decreases in operation time, estimated blood loss, and hematocrit were 176 minutes, 83 mL, and 6.6%, respectively. The stone-free rate was 89% (8 of 9) without any procedure-related complications. However, there is still no exact definition as to what should be called mini-PCNL or mini-perc. Since the first trial of miniaturized PCNL, several authors have utilized various sizes of working sheaths ranging from 11 to 20 Fr [60616263]. Thus, the term mini-PCNL is used for any PCNL that utilizes access tracts of 20 Fr or smaller [2]. In addition, Desai et al. [64] recently introduced the smallest sized access tract (4.8 Fr), which was named "microperc."
Definite indications for mini-PCNL have not been clearly defined. However, mini-PCNL can be the first-line treatment for renal stones with a diameter larger than 2 cm in children [2], and general indications for mini-PCNL in adults may include renal stones less than 2 or 2.5 cm in size with previous failure of ESWL or RIRS, cystine stones, and anatomical abnormalities inhibiting retrograde access or distal passage of stones [61]. Mini-PCNL can also be used in patients with a narrow or long infundibulum or as a secondary access for inaccessible or residual stones after standard PCNL [261]. Nevertheless, mini-PCNL has not only been used for the management of smaller renal stones or pediatric renal stones but for large impacted upper ureteral stones and staghorn calculi as well [65666768].
The advantages of mini-PCNL, based on several prospective trials, are less bleeding, increased maneuverability, lower postoperative pain, and reduced hospital stay. However, the longer operation time due to the need to disintegrate stones into small fragments to evacuate through a small-sized sheath is a limitation of mini-PCNL [697071]. Most studies reported similar stone-free rates and comparable overall complication rates between mini-PCNL and standard PCNL for the management of renal stones less than 2.5 cm in size [269]. Compared with ESWL, mini-PCNL has been reported to have significantly higher stone-free rates, especially for renal stones greater than 1 cm, although it is more invasive [7273]. Compared to RIRS, mini-PCNL has shown better stone-free rates for the management of larger renal stones (2-3 cm) [74] and large impacted upper ureteral stones [75], but similar effectiveness was reported when treating smaller renal stones between both procedures [7677]. In these studies, mini-PCNL was superior in terms of operation time for the management of comparably sized stones, but was inferior with respect to invasiveness. However, the combination of RIRS and mini-PCNL showed better outcomes than did mini-PCNL alone for large renal stones (>3 cm) with shorter operation times [78].
Microperc, which uses the smallest sized access tract, can be applicable for small or intermediate-sized lower calyceal stones, especially stones that are ESWL-resistant or retrograde inaccessible. Specifically, microperc can also be used for the management of renal stones in calyceal diverticula and in horseshoe and ectopic kidneys [64]. However, further prospective randomized controlled trials will be needed to validate the safety, efficacy, and applicability of this technique.
After completing the lithotripsy, the final step in PCNL is sealing the nephrostomy tract. Traditionally, a large-caliber nephrostomy tube, such as a 24-Fr Council catheter, a reentry Malecot catheter, or a nephroureteral stent, was placed to provide hemostasis of the tract and maintain adequate urine drainage. The nephrostomy tube was historically left indwelling for several days, which required a prolonged hospital stay, increased analgesic use owing to patient discomfort, and resulted in urinary extravasation around the tube. Many trials have been conducted to overcome these drawbacks.
The first such trial involved the placement of a smaller sized nephrostomy tube instead of a large-bore one. Several studies have compared the outcomes of PCNL using different sized nephrostomy tubes. Maheshwari et al compared a patient group who underwent PCNL and had either a 28-Fr nephrostomy tube or a 9-Fr pigtail catheter postoperatively [79]. In that study, the incidence of hematuria was comparable between the two groups, but the 9-Fr pigtail catheter group showed a lower analgesic requirement, less urine leakage, and a shorter hospital stay. Pietrow et al. [80] also reported similar results from their randomized prospective trial comparing a 22-Fr Council catheter with a 10-Fr pigtail catheter.
Although Wickham et al. [81] f irst described no placement of a nephrostomy tube after PCNL in 1984, tubeless PCNL was not actively attempted for over 10 years because postoperative hemorrhage was reported [82]. The first series of tubeless PCNL was reported in 1997 by Bellman et al. [83]. In that study, the tubeless PCNL group showed comparable stone-free and complication rates, a lower analgesic requirement (11.58 mg vs. 36.06 mg of morphine sulfate, p=0.0001), a reduced hospital stay (0.6 days vs. 4.6 days, p=0.0001), and an earlier return to normal activity (17.85 days vs. 26.6 days, p=0.0004) compared with the standard PCNL group with a 22-Fr nephrostomy tube. Since then, many studies have evaluated the safety and applicability of tubeless PCNL. Desai et al. [84] compared three different randomly divided groups (22-Fr nephrostomy tube, 9-Fr pigtail catheter, and 6-Fr double-J stent without nephrostomy tube) and reported no significant differences in blood loss among the three groups. They also found that analgesics were most frequently required in the 22-Fr nephrostomy tube group, and the duration of urine leakage and hospital stay was the shortest in the tubeless group. Marcovich et al. [85] also reported no significant difference in blood loss or the transfusion rate when comparing three different groups according to the size of the nephrostomy tube (24-Fr reentry catheter, 8-Fr pigtail catheter, and tubeless). However, analgesic use and hospital stay were also not significantly different in their series. Meta-analysis also showed that tubeless PCNL was associated with lower analgesic requirements, shorter hospital stay, and comparable blood loss compared with standard PCNL [8687].
Although the indications for tubeless PCNL have not been clearly defined, initially, tubeless PCNL was performed only in highly selected cases such as uncomplicated stones, smaller stones (less than 3 cm), normal renal function, single-tract procedure, short operation time, complete stone removal, no collecting system perforation, and no active bleeding from the tract at completion [10]. Since then, there have been several efforts to apply tubeless PCNL in more complicated cases, including multiple, complex, and bilateral stones; patients with elevated serum creatinine; children; obese patients; and elderly patients [888990]. On the basis of these current experiences and analyses, many investigators have concluded that tubeless PCNL should be avoided in case of multiple access, serious intraoperative bleeding, collecting system perforation, and need for early second-look surgery [1056].
Although many studies have reported that tubeless PCNL can be safely performed in well-selected cases, there are still concerns associated with tract bleeding. Limb and Bellman [91] reported a postoperative transfusion rate of 5.4% (6 of 112) and 2 cases (1.8%) of renal pseudoaneurysm, which were managed by selective angioembolization, in their first 112 tubeless renal surgery cases. To overcome these concerns, several techniques for tract sealing, such as electrocauterization of bleeding points, applying fibrin glue, and placement of hemostatic matrix into the tract, have been tried [92939495]. Most of these studies reported favorable outcomes in terms of safety and efficacy for the tract control, but routine use of these tract-sealing techniques in tubeless PCNL to prevent tract bleeding or urine leakage is still controversial. Moreover, the possibility of stone formation in the collecting system due to misplacement of these biological sealants or worsening of bleeding with further renal parenchymal injury due to inappropriate electrocauterization are possible side effects of these techniques. Thus, meticulous care must be taken when the tract-sealing technique is considered for tubeless PCNL.
Initially, tubeless PCNL was performed with placement of an internal double-J stent for the purpose of preventing urinary extravasation. The internal stent can also cause patient discomfort owing to bladder irritation symptoms and urine reflux. In addition, the most bothersome fact is the need for postoperative stent removal by use of cystoscopy. To avoid this procedure, several attempts such as leaving the string attached to the stent and using externalized ureteral stents have been tried, but there is the risk that patients may pull out their stents prematurely by accident, and the risk of urinary tract infection may be increased. To overcome these drawbacks, "totally tubeless" PCNL, which is tubeless and stentless, has been introduced [9697]. Many investigators have suggested that the best available urinary drainage method from the kidney is the normal peristaltic ureter and the only indication for ureteral stent placement is ureteral obstruction due to edema, inflammation, presence of residual stones, or stricture [1088]. Several studies have demonstrated that totally tubeless PCNL is safe, effective, and well tolerated in selected patients and is associated with a shorter hospital stay, less postoperative pain, and decreased analgesic requirements compared with standard PCNL [9899]. There are limited prospective randomized study data comparing totally tubeless and tubeless PCNL, but Istanbulluoglu et al. [99] found that totally tubeless PCNL had comparable blood loss, success rates, operation time, hospital stay, analgesic requirements, and complication rates with the advantage of no need for stent removal even compared with tubeless PCNL in their retrospective study. To validate these data, further prospective randomized trials will be needed to compare safety and efficacy between totally tubeless and tubeless PCNL.
PCNL was developed to reduce the morbidity and mortality associated with open renal surgery, and it currently remains the first-line treatment for large renal stones. However, it represents the most morbid of the minimally invasive endoscopic surgeries for renal stones. Over the years, with the development of endoscopic instruments and techniques, the role of ESWL and RIRS has increased. Nevertheless, PCNL still has many advantages over ESWL and RIRS in some cases. Currently, many efforts and trials to reduce morbidity and increase the efficiency and effectiveness of PCNL have furthered this procedure technically and have broadened its indications. Recent advancements that make PCNL a less-invasive technique promise higher success rates and less perioperative complications. Further efforts will be needed to validate the many promising retrospective data by use of large-scale prospective studies and to develop this procedure more safely and effectively.
Figures and Tables
 | Fig. 1Schematic images of percutaneous access for percutaneous nephrolithotomy (PCNL) in the supine position. The position is usually modified by using a saline bag or a specially made cushion below the ipsilateral upper flank, except in the complete supine position PCNL. (A) Transverse view, (B) lateral view. Arrow indicates direction of percutaneous access. |
Table 1
History of the first advancement of percutaneous nephrolithotomy
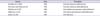
| Source | Year | Procedure |
|---|---|---|
| Goodwin et al. [100] | 1955 | First percutaneous nephrostomy |
| Fernstrom and Johansson [5] | 1976 | First percutaneous nephrolithotomy |
| Wickham et al. [81] | 1984 | First tubeless percutaneous nephrolithotomy |
| Valdivia et al. [14] | 1987 | First supine percutaneous nephrolithotomy |
| Helal et al. [59] | 1997 | First mini-perc |
References
1. Stamatelou KK, Francis ME, Jones CA, Nyberg LM, Curhan GC. Time trends in reported prevalence of kidney stones in the United States: 1976-1994. Kidney Int. 2003; 63:1817–1823.
2. Ferakis N, Stavropoulos M. Mini percutaneous nephrolithotomy in the treatment of renal and upper ureteral stones: Lessons learned from a review of the literature. Urol Ann. 2015; 7:141–148.
3. Lee JK, Kim BS, Park YK. Predictive factors for bleeding during percutaneous nephrolithotomy. Korean J Urol. 2013; 54:448–453.
4. Turk C, Knoll T, Petrik A, Sarica K, Skolarikos A, Straub M, et al. Guidelines on urolithiasis. Arnheim (NL): European Association of Urology;2015.
5. Fernström I, Johansson B. Percutaneous pyelolithotomy. a new extraction technique. Scand J Urol Nephrol. 1976; 10:257–259.
6. Gupta NP, Mishra S, Seth A, Anand A. Percutaneous nephrolithotomy in abnormal kidneys: single-center experience. Urology. 2009; 73:710–714.
7. Liatsikos EN, Kallidonis P, Stolzenburg JU, Ost M, Keeley F, Traxer O, et al. Percutaneous management of staghorn calculi in horseshoe kidneys: a multi-institutional experience. J Endourol. 2010; 24:531–536.
8. Umbreit EC, Childs MA, Patterson DE, Torres VE, LeRoy AJ, Gettman MT. Percutaneous nephrolithotomy for large or multiple upper tract calculi and autosomal dominant polycystic kidney disease. J Urol. 2010; 183:183–187.
9. Yuruk E, Binbay M, Sari E, Akman T, Altinyay E, Baykal M, et al. A prospective, randomized trial of management for asymptomatic lower pole calculi. J Urol. 2010; 183:1424–1428.
10. Cracco CM, Scoffone CM, Scarpa RM. New developments in percutaneous techniques for simple and complex branched renal stones. Curr Opin Urol. 2011; 21:154–160.
11. de la Rosette JJ, Tsakiris P, Ferrandino MN, Elsakka AM, Rioja J, Preminger GM. Beyond prone position in percutaneous nephrolithotomy: a comprehensive review. Eur Urol. 2008; 54:1262–1269.
12. Ibarluzea G, Scoffone CM, Cracco CM, Poggio M, Porpiglia F, Terrone C, et al. Supine Valdivia and modified lithotomy position for simultaneous anterograde and retrograde endourological access. BJU Int. 2007; 100:233–236.
13. Miano R, Scoffone C, De Nunzio C, Germani S, Cracco C, Usai P, et al. Position: prone or supine is the issue of percutaneous nephrolithotomy. J Endourol. 2010; 24:931–938.
14. Valdivia Uria JG, Lachares Santamaria E, Villarroya Rodriguez S, Taberner Llop J, Abril Baquero G, Aranda Lassa JM. Percutaneous nephrolithotomy: simplified technique (preliminary report). Arch Esp Urol. 1987; 40:177–180.
15. Grasso M, Nord R, Bagley DH. Prone split leg and flank roll positioning: simultaneous antegrade and retrograde access to the upper urinary tract. J Endourol. 1993; 7:307–310.
16. Ray AA, Chung DG, Honey RJ. Percutaneous nephrolithotomy in the prone and prone-flexed positions: anatomic considerations. J Endourol. 2009; 23:1607–1614.
17. Valdivia Uria JG, Valle Gerhold J, Lopez Lopez JA, Villarroya Rodriguez S, Ambroj Navarro C, Ramirez Fabian M, et al. Technique and complications of percutaneous nephroscopy: experience with 557 patients in the supine position. J Urol. 1998; 160(6 Pt 1):1975–1978.
18. Steele D, Marshall V. Percutaneous nephrolithotomy in the supine position: a neglected approach? J Endourol. 2007; 21:1433–1437.
19. Rana AM, Bhojwani JP, Junejo NN, Das Bhagia S. Tubeless PCNL with patient in supine position: procedure for all seasons?--with comprehensive technique. Urology. 2008; 71:581–585.
20. Ng MT, Sun WH, Cheng CW, Chan ES. Supine position is safe and effective for percutaneous nephrolithotomy. J Endourol. 2004; 18:469–474.
21. Neto EA, Mitre AI, Gomes CM, Arap MA, Srougi M. Percutaneous nephrolithotripsy with the patient in a modified supine position. J Urol. 2007; 178:165–168.
22. Manohar T, Jain P, Desai M. Supine percutaneous nephrolithotomy: Effective approach to high-risk and morbidly obese patients. J Endourol. 2007; 21:44–49.
23. Liu L, Zheng S, Xu Y, Wei Q. Systematic review and meta-analysis of percutaneous nephrolithotomy for patients in the supine versus prone position. J Endourol. 2010; 24:1941–1946.
24. Basiri A, Mohammadi Sichani M. Supine percutaneous nephrolithotomy, is it really effective? A systematic review of literature. Urol J. 2009; 6:73–77.
25. Wu P, Wang L, Wang K. Supine versus prone position in percutaneous nephrolithotomy for kidney calculi: a meta-analysis. Int Urol Nephrol. 2011; 43:67–77.
26. Falahatkar S, Enshaei A, Afsharimoghaddam A, Emadi SA, Allahkhah AA. Complete supine percutaneous nephrolithotomy with lung inflation avoids the need for a supracostal puncture. J Endourol. 2010; 24:213–218.
27. Ghani KR, Patel U, Anson K. Computed tomography for percutaneous renal access. J Endourol. 2009; 23:1633–1639.
28. Patel U, Walkden RM, Ghani KR, Anson K. Three-dimensional CT pyelography for planning of percutaneous nephrostolithotomy: accuracy of stone measurement, stone depiction and pelvicalyceal reconstruction. Eur Radiol. 2009; 19:1280–1288.
29. Arrabal-Polo MA, Arrabal-Martin M, Saz T, Paiz P. Emergency percutaneous nephrostomy in supine-oblique position without cushion. Urol Res. 2011; 39:521–522.
30. Xu KW, Huang J, Guo ZH, Lin TX, Zhang CX, Liu H, et al. Percutaneous nephrolithotomy in semisupine position: a modified approach for renal calculus. Urol Res. 2011; 39:467–475.
31. El-Husseiny T, Moraitis K, Maan Z, Papatsoris A, Saunders P, Golden B, et al. Percutaneous endourologic procedures in high-risk patients in the lateral decubitus position under regional anesthesia. J Endourol. 2009; 23:1603–1606.
32. Lezrek M, Ammani A, Bazine K, Assebane M, Kasmaoui el H, Qarro A, et al. The split-leg modified lateral position for percutaneous renal surgery and optimal retrograde access to the upper urinary tract. Urology. 2011; 78:217–220.
33. Jang WS, Choi KH, Yang SC, Han WK. The learning curve for flank percutaneous nephrolithotomy for kidney calculi: a single surgeon's experience. Korean J Urol. 2011; 52:284–288.
34. Karami H, Rezaei A, Mohammadhosseini M, Javanmard B, Mazloomfard M, Lotfi B. Ultrasonography-guided percutaneous nephrolithotomy in the flank position versus fluoroscopy-guided percutaneous nephrolithotomy in the prone position: a comparative study. J Endourol. 2010; 24:1357–1361.
35. Basiri A, Ziaee AM, Kianian HR, Mehrabi S, Karami H, Moghaddam SM. Ultrasonographic versus fluoroscopic access for percutaneous nephrolithotomy: a randomized clinical trial. J Endourol. 2008; 22:281–284.
36. Basiri A, Ziaee SA, Nasseh H, Kamranmanesh M, Masoudy P, Heidary F, et al. Totally ultrasonography-guided percutaneous nephrolithotomy in the flank position. J Endourol. 2008; 22:1453–1457.
37. Hosseini MM, Hassanpour A, Farzan R, Yousefi A, Afrasiabi MA. Ultrasonography-guided percutaneous nephrolithotomy. J Endourol. 2009; 23:603–607.
38. Karami H, Arbab AH, Rezaei A, Mohammadhoseini M, Rezaei I. Percutaneous nephrolithotomy with ultrasonography-guided renal access in the lateral decubitus flank position. J Endourol. 2009; 23:33–35.
39. Park S, Pearle MS. Imaging for percutaneous renal access and management of renal calculi. Urol Clin North Am. 2006; 33:353–364.
40. Matlaga BR, Shah OD, Zagoria RJ, Dyer RB, Streem SB, Assimos DG. Computerized tomography guided access for percutaneous nephrostolithotomy. J Urol. 2003; 170:45–47.
41. Hagspiel KD, Kandarpa K, Silverman SG. Interactive MRguided percutaneous nephrostomy. J Magn Reson Imaging. 1998; 8:1319–1322.
42. Kariniemi J, Sequeiros RB, Ojala R, Tervonen O. MRI-guided percutaneous nephrostomy: a feasibility study. Eur Radiol. 2009; 19:1296–1301.
43. Lawson RK, Murphy JB, Taylor AJ, Jacobs SC. Retrograde method for percutaneous access to kidney. Urology. 1983; 22:580–582.
44. Hunter PT, Hawkins IF, Finlayson B, Nanni G, Senior D. Hawkins-Hunter retrograde transcutaneous nephrostomy: a new technique. Urology. 1983; 22:583–587.
45. Grasso M, Lang G, Taylor FC. Flexible ureteroscopically assisted percutaneous renal access. Tech Urol. 1995; 1:39–43.
46. Kidd CF, Conlin MJ. Ureteroscopically assisted percutaneous renal access. Urology. 2003; 61:1244–1245.
47. Bader MJ, Gratzke C, Seitz M, Sharma R, Stief CG, Desai M. The "all-seeing needle": initial results of an optical puncture system confirming access in percutaneous nephrolithotomy. Eur Urol. 2011; 59:1054–1059.
48. Marberger M. Disintegration of renal and ureteral calculi with ultrasound. Urol Clin North Am. 1983; 10:729–742.
49. Teh CL, Zhong P, Preminger GM. Laboratory and clinical assessment of pneumatically driven intracorporeal lithotripsy. J Endourol. 1998; 12:163–169.
50. Kuo RL, Paterson RF, Siqueira TM Jr, Evan AP, McAteer JA, Williams JC Jr, et al. In vitro assessment of lithoclast ultra intracorporeal lithotripter. J Endourol. 2004; 18:153–156.
51. Kim SC, Matlaga BR, Tinmouth WW, Kuo RL, Evan AP, McAteer JA, et al. In vitro assessment of a novel dual probe ultrasonic intracorporeal lithotriptor. J Urol. 2007; 177:1363–1365.
52. Pietrow PK, Auge BK, Zhong P, Preminger GM. Clinical efficacy of a combination pneumatic and ultrasonic lithotrite. J Urol. 2003; 169:1247–1249.
53. Krambeck AE, Miller NL, Humphreys MR, Nakada SY, Denstedt JD, Razvi H, et al. Randomized controlled, multicentre clinical trial comparing a dual-probe ultrasonic lithotrite with a single-probe lithotrite for percutaneous nephrolithotomy. BJU Int. 2011; 107:824–828.
54. Sun Y, Gao X, Zhou T, Chen S, Wang L, Xu C, et al. 70 W holmium: yttrium-aluminum-garnet laser in percutaneous nephrolithotomy for staghorn calculi. J Endourol. 2009; 23:1687–1691.
55. Gu Z, Qi J, Shen H, Liu J, Chen J. Percutaneous nephroscopic with holmium laser and ultrasound lithotripsy for complicated renal calculi. Lasers Med Sci. 2010; 25:577–580.
56. Antonelli JA, Pearle MS. Advances in percutaneous nephrolithotomy. Urol Clin North Am. 2013; 40:99–113.
57. Kukreja R, Desai M, Patel S, Bapat S, Desai M. Factors affecting blood loss during percutaneous nephrolithotomy: prospective study. J Endourol. 2004; 18:715–722.
58. Yamaguchi A, Skolarikos A, Buchholz NP, Chomon GB, Grasso M, Saba P, et al. Operating times and bleeding complications in percutaneous nephrolithotomy: a comparison of tract dilation methods in 5,537 patients in the Clinical Research Office of the Endourological Society Percutaneous Nephrolithotomy Global Study. J Endourol. 2011; 25:933–939.
59. Helal M, Black T, Lockhart J, Figueroa TE. The Hickman peel-away sheath: alternative for pediatric percutaneous nephrolithotomy. J Endourol. 1997; 11:171–172.
60. Jackman SV, Docimo SG, Cadeddu JA, Bishoff JT, Kavoussi LR, Jarrett TW. The "mini-perc" technique: a less invasive alternative to percutaneous nephrolithotomy. World J Urol. 1998; 16:371–374.
61. Chan DY, Jarrett TW. Mini-percutaneous nephrolithotomy. J Endourol. 2000; 14:269–272.
62. Lahme S, Bichler KH, Strohmaier WL, Gotz T. Minimally invasive PCNL in patients with renal pelvic and calyceal stones. Eur Urol. 2001; 40:619–624.
63. Nagele U, Schilling D, Sievert KD, Stenzl A, Kuczyk M. Management of lower-pole stones of 0.8 to 1.5 cm maximal diameter by the minimally invasive percutaneous approach. J Endourol. 2008; 22:1851–1853.
64. Desai MR, Sharma R, Mishra S, Sabnis RB, Stief C, Bader M. Single-step percutaneous nephrolithotomy (microperc): the initial clinical report. J Urol. 2011; 186:140–145.
65. Yang Z, Song L, Xie D, Hu M, Peng Z, Liu T, et al. Comparative study of outcome in treating upper ureteral impacted stones using minimally invasive percutaneous nephrolithotomy with aid of patented system or transurethral ureteroscopy. Urology. 2012; 80:1192–1197.
66. Zeng G, Mai Z, Zhao Z, Li X, Zhong W, Yuan J, et al. Treatment of upper urinary calculi with Chinese minimally invasive percutaneous nephrolithotomy: a single-center experience with 12,482 consecutive patients over 20 years. Urolithiasis. 2013; 41:225–229.
67. Zeng G, Zhao Z, Wan S, Mai Z, Wu W, Zhong W, et al. Minimally invasive percutaneous nephrolithotomy for simple and complex renal caliceal stones: a comparative analysis of more than 10,000 cases. J Endourol. 2013; 27:1203–1208.
68. Zhong W, Zeng G, Wu W, Chen W, Wu K. Minimally invasive percutaneous nephrolithotomy with multiple mini tracts in a single session in treating staghorn calculi. Urol Res. 2011; 39:117–122.
69. Knoll T, Wezel F, Michel MS, Honeck P, Wendt-Nordahl G. Do patients benefit from miniaturized tubeless percutaneous nephrolithotomy? A comparative prospective study. J Endourol. 2010; 24:1075–1079.
70. Mishra S, Sharma R, Garg C, Kurien A, Sabnis R, Desai M. Prospective comparative study of miniperc and standard PNL for treatment of 1 to 2 cm size renal stone. BJU Int. 2011; 108:896–899.
71. Cheng F, Yu W, Zhang X, Yang S, Xia Y, Ruan Y. Minimally invasive tract in percutaneous nephrolithotomy for renal stones. J Endourol. 2010; 24:1579–1582.
72. Kruck S, Anastasiadis AG, Herrmann TR, Walcher U, Abdelhafez MF, Nicklas AP, et al. Minimally invasive percutaneous nephrolithotomy: an alternative to retrograde intrarenal surgery and shockwave lithotripsy. World J Urol. 2013; 31:1555–1561.
73. Zeng G, Jia J, Zhao Z, Wu W, Zhao Z, Zhong W. Treatment of renal stones in infants: comparing extracorporeal shock wave lithotripsy and mini-percutaneous nephrolithotomy. Urol Res. 2012; 40:599–603.
74. Pan J, Chen Q, Xue W, Chen Y, Xia L, Chen H, et al. RIRS versus mPCNL for single renal stone of 2-3 cm: clinical outcome and cost-effective analysis in Chinese medical setting. Urolithiasis. 2013; 41:73–78.
75. Gu XJ, Lu JL, Xu Y. Treatment of large impacted proximal ureteral stones: randomized comparison of minimally invasive percutaneous antegrade ureterolithotripsy versus retrograde ureterolithotripsy. World J Urol. 2013; 31:1605–1610.
76. Kirac M, Bozkurt OF, Tunc L, Guneri C, Unsal A, Biri H. Comparison of retrograde intrarenal surgery and mini-percutaneous nephrolithotomy in management of lower-pole renal stones with a diameter of smaller than 15 mm. Urolithiasis. 2013; 41:241–246.
77. Knoll T, Jessen JP, Honeck P, Wendt-Nordahl G. Flexible ureterorenoscopy versus miniaturized PNL for solitary renal calculi of 10-30 mm size. World J Urol. 2011; 29:755–759.
78. Hamamoto S, Yasui T, Okada A, Taguchi K, Kawai N, Ando R, et al. Endoscopic combined intrarenal surgery for large calculi: simultaneous use of flexible ureteroscopy and mini-percutaneous nephrolithotomy overcomes the disadvantageous of percutaneous nephrolithotomy monotherapy. J Endourol. 2014; 28:28–33.
79. Maheshwari PN, Andankar MG, Bansal M. Nephrostomy tube after percutaneous nephrolithotomy: large-bore or pigtail catheter? J Endourol. 2000; 14:735–737.
80. Pietrow PK, Auge BK, Lallas CD, Santa-Cruz RW, Newman GE, Albala DM, et al. Pain after percutaneous nephrolithotomy: impact of nephrostomy tube size. J Endourol. 2003; 17:411–414.
81. Wickham JE, Miller RA, Kellett MJ, Payne SR. Percutaneous nephrolithotomy: one stage or two? Br J Urol. 1984; 56:582–585.
82. Winfield HN, Weyman P, Clayman RV. Percutaneous nephrostolithotomy: complications of premature nephrostomy tube removal. J Urol. 1986; 136:77–79.
83. Bellman GC, Davidoff R, Candela J, Gerspach J, Kurtz S, Stout L. Tubeless percutaneous renal surgery. J Urol. 1997; 157:1578–1582.
84. Desai MR, Kukreja RA, Desai MM, Mhaskar SS, Wani KA, Patel SH, et al. A prospective randomized comparison of type of nephrostomy drainage following percutaneous nephrostolithotomy: large bore versus small bore versus tubeless. J Urol. 2004; 172:565–567.
85. Marcovich R, Jacobson AI, Singh J, Shah D, El-Hakim A, Lee BR, et al. No panacea for drainage after percutaneous nephrolithotomy. J Endourol. 2004; 18:743–747.
86. Wang J, Zhao C, Zhang C, Fan X, Lin Y, Jiang Q. Tubeless vs standard percutaneous nephrolithotomy: a meta-analysis. BJU Int. 2012; 109:918–924.
87. Yuan H, Zheng S, Liu L, Han P, Wang J, Wei Q. The efficacy and safety of tubeless percutaneous nephrolithotomy: a systematic review and meta-analysis. Urol Res. 2011; 39:401–410.
88. Agrawal MS, Agrawal M. Tubeless percutaneous nephrolithotomy. Indian J Urol. 2010; 26:16–24.
89. Kara C, Resorlu B, Bayindir M, Unsal A. A randomized comparison of totally tubeless and standard percutaneous nephrolithotomy in elderly patients. Urology. 2010; 76:289–293.
90. Zilberman DE, Lipkin ME, de la Rosette JJ, Ferrandino MN, Mamoulakis C, Laguna MP, et al. Tubeless percutaneous nephrolithotomy: the new standard of care? J Urol. 2010; 184:1261–1266.
91. Limb J, Bellman GC. Tubeless percutaneous renal surgery: review of first 112 patients. Urology. 2002; 59:527–531.
92. Jou YC, Cheng MC, Sheen JH, Lin CT, Chen PC. Electrocauterization of bleeding points for percutaneous nephrolithotomy. Urology. 2004; 64:443–446.
93. Nagele U, Schilling D, Anastasiadis AG, Corvin S, Seibold J, Kuczyk M, et al. Closing the tract of mini-percutaneous nephrolithotomy with gelatine matrix hemostatic sealant can replace nephrostomy tube placement. Urology. 2006; 68:489–493.
94. Shah HN, Hegde S, Shah JN, Mohile PD, Yuvaraja TB, Bansal MB. A prospective, randomized trial evaluating the safety and efficacy of fibrin sealant in tubeless percutaneous nephrolithotomy. J Urol. 2006; 176(6 Pt 1):2488–2492.
95. Cormio L. TachoSil sealed tubeless percutaneous nephrolithotomy to reduce urine leakage and bleeding: outcome of a randomized controlled Study. J Urol. 2012; 09. 14. [Epub]. DOI: 10.1016/j.juro.2012.08.207.
96. Aghamir SM, Hosseini SR, Gooran S. Totally tubeless percutaneous nephrolithotomy. J Endourol. 2004; 18:647–648.
97. Gupta V, Sadasukhi TC, Sharma KK, Yadav RG, Mathur R. Tubeless and stentless percutaneous nephrolithotomy. BJU Int. 2005; 95:905–906.
98. Chang CH, Wang CJ, Huang SW. Totally tubeless percutaneous nephrolithotomy: a prospective randomized controlled study. Urol Res. 2011; 39:459–465.
99. Istanbulluoglu MO, Cicek T, Ozturk B, Gonen M, Ozkardes H. Percutaneous nephrolithotomy: nephrostomy or tubeless or totally tubeless? Urology. 2010; 75:1043–1046.
100. Goodwin WE, Casey WC, Woolf W. Percutaneouis trocar (needle) nephrostomy in hydronephrosis. J Am Med Assoc. 1955; 157:891–894.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download