Abstract
Purpose
The objective was to determine whether stone density on plain radiography (kidney-ureter-bladder, KUB) could predict the outcome of extracorporeal shockwave lithotripsy (ESWL) for ureteral stones.
Materials and Methods
A total of 223 patients treated by ESWL for radio-opaque ureteral stones of 5 to 20 mm were included in this retrospective study. All patients underwent routine blood and urine analyses, plain radiography (KUB), and noncontrast computed tomography (NCCT) before ESWL. Demographic, stone, and radiological characteristics on KUB and NCCT were analyzed. The patients were categorized into two groups: lower-density (LD) group (radiodensity less than or equal to that of the 12th rib, n=163) and higher-density (HD) group (radiodensity greater than that of the 12th rib, n=60). Stone-free status was assessed by KUB every week after ESWL. A successful outcome was defined as stone free within 1 month after ESWL.
Results
Mean stone size in the LD group was significantly smaller than that in the HD group (7.5±1.4 mm compared with 9.9±2.9 mm, p=0.002). The overall success rates in the LD and HD groups were 82.1% and 60.0%, respectively (p=0.007). The mean duration of stone-free status and average number of SWL sessions required for success in the two groups were 21.7 compared with 39.2 days and 1.8 compared with 2.3, respectively (p<0.05). On multivariate logistic analysis, stone size and time to ESWL since colic and radiodensity of the stone on KUB were independent predictors of successful ESWL.
Urinary tract stones affect 10% of individuals in industrialized countries, and 50% of first-time stone formers who do not receive treatment have another stone within 5 years [1]. Various treatment options are available, such as extracorporeal shockwave lithotripsy (ESWL), ureteroscopic stone removal, and percutaneous nephrolithotomy. Of these, ESWL has become the most popular noninvasive intervention for stone disease. However, all urinary stones are not easily fragmented by ESWL, and the success rate of ESWL depends on multiple factors, such as stone size, location, and composition [2]. Auxiliary procedures, which are used in cases of ESWL failure to clear stones, are costly and time consuming. Therefore, it would be useful to be able to predict which stones will be successfully fragmented by ESWL.
Several studies have investigated how to predict the success of ESWL treatment with radiological tools, such as noncontrast computed tomography (NCCT) and plain x-ray (kidney-ureter-bladder, KUB). Recently, many studies have attempted to correlate the radiographic findings on NCCT with ESWL treatment success. Most studies have shown that the consistency, size, shape, location, and attenuation value of urinary calculi measured in Hounsfield unit (HU) density on NCCT and body mass index may be predictors of ESWL success, as determined by the stone-free (SF) rate [3,4]. However, NCCT has some disadvantages. Diagnosis with NCCT is costly, and this procedure exposes patients to more radiation than does plain x-ray. To avoid these disadvantages, intravenous pyelogram or KUB x-ray has been used as an alternative; however, the accuracy of these methods is not as good as that of NCCT [5]. However, if we were able to predict the success rate of ESWL based on stone characteristics determined by KUB, it would help eliminate the need for NCCT.
However, the data regarding prediction of ESWL outcomes by KUB are limited to two studies. Dretler [6] suggested that smooth-edged calculi with a homogeneous structure in on KUB required more shockwaves to be completely fragmented than did calculi with round, radially reticulated, and speculated edges and irregular margins. Bon et al. [7] found that smooth, uniform, bulging calculi that appeared denser than bone (12th rib or transverse process) responded poorly to ESWL.
Domestically, no study has been conducted to predict ESWL outcomes based on KUB findings. Furthermore, few studies have analyzed KUB and NCCT findings together for predicting ESWL outcomes. The aim of this study was to determine whether radiological findings on NCCT and KUB can predict the outcome of ESWL for ureteral stones.
Between July 2005 and July 2013, a total of 223 patients who underwent ESWL for radio-opaque, single ureteral stones of 5 to 20 mm were included in this retrospective study. The exclusion criteria were as follows: simultaneous treatment of renal stone or bilateral ureteral stones, placement of percutaneous nephrostomy tube or ureteral stent before ESWL, or structural urinary tract abnormality. All patients underwent a baseline evaluation, including a medical history, a physical examination, a complete blood count, a serum creatinine measurement, determination of the glomerular f iltration rate, a urinalysis, a urine culture, a KUB, and an NCCT. The radiological parameters on KUB included stone location, stone width, stone length, surface outline, and stone density relative to that of the 12th rib. The surface outline of the stone was classified as smooth or irregular. Stone density relative to that of the 12th rib was assigned a value of less than, equal to, or more than the radiodensity of the 12th rib on KUB (Fig. 1). In terms of stone density relative to that of the 12th rib on KUB and surface outline, two radiologists who were blind to each other's interpretations evaluated all KUB results. In case of a lack of consensus between the two radiologists, a third radiologist was involved in the final KUB interpretation. To investigate the effect of stone density on ESWL, patients were divided into two subgroups. The lower-density (LD) group was assigned a density less than or equal to that of the 12th rib, and the higher-density (HD) group was assigned a density greater than that of the 12th rib [7].
For NCCT, the maximum diameter of stone, stone cross-sectional area, presence or absence of hydronephrosis, tissue rim sign, skin-to-stone distance (SSD), and average and maximum Hounsf ield density were evaluated, respectively. The tissue rim sign is recognized as an area of soft tissue attenuation surrounding a suspended ureteral calculus that appears calcified [5]. The SSD was calculated on NCCT by three measured distances from the center of the stone to the skin (0°, 45°, and 90°) using radiographic calipers at an NCCT workstation [3]. The measurements were designed to capture the distance required to pass from the skin to the stone. The average SSD was calculated from these values and recorded as the representative SSD for each stone [4]. Follow-up SF status was assessed by KUB every week after ESWL. Successful outcome was defined as no radio-opaque stones on KUB within 4 weeks after ESWL. In patients in whom SF status on KUB was indeterminate, NCCT was performed after discussion with the patients. All other outcomes were regarded as failures. This study was approved by the Institutional Review Board at our hospital.
All patients were managed with intramuscular administration of ketolorac (30 mg) or intravenous administration of pethidine (50 mg). All procedures were performed with the same electromagnetic Dornier Compact Delta lithotriptor (Dornier Medtech, Kennesaw, GA, USA) under fluoroscopy, as described previously [8]. Briefly, a maximum of 3,000 shocks per session were delivered to the stone at a frequency of 100 shocks per minute, and the power was set at 15 to 20 kV.
The statistical analysis was performed by using a Fisher exact test or chi-square test for categorical variables. For continuous variables, the independent t-test was used to compare the results between the two groups for normally distributed data, and the Mann-Whitney U test was used for skewed data. To minimize confounding effects by discrepancy of baseline parameters between the groups, we performed a propensity-score matching analysis after determining propensity scores with a multivariate logistic regression analysis including patient age, sex, stone size, and stone location. To identify the predictive factors for ESWL success, we used logistic regression analysis. Variables with a p-value <0.05 on univariate analysis were included in the multivariate logistic model. A 5% level of significance was used for all statistical testing, and all statistical tests were two-sided. The IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA) was used for the data analysis.
The LD group consisted of 163 patients (73.1%), and the HD group consisted of 60 patients (26.9%). Mean stone size in the LD group was significantly smaller than that in the HD group (7.5±1.4 mm compared with 9.9±2.9 mm, p=0.002). Also, the average HU density in the two groups was 789.8±348.1 and 1030.7±338.5, respectively, which was significantly different between the two groups (p<0.001). No significant differences in other baseline characteristics, such as age, body mass index, and glomerular filtration rate, were found between the two groups. Other radiological parameters such as stone location, surface outline, hydronephrosis, tissue rim sign, and SSD were not significantly different (Table 1).
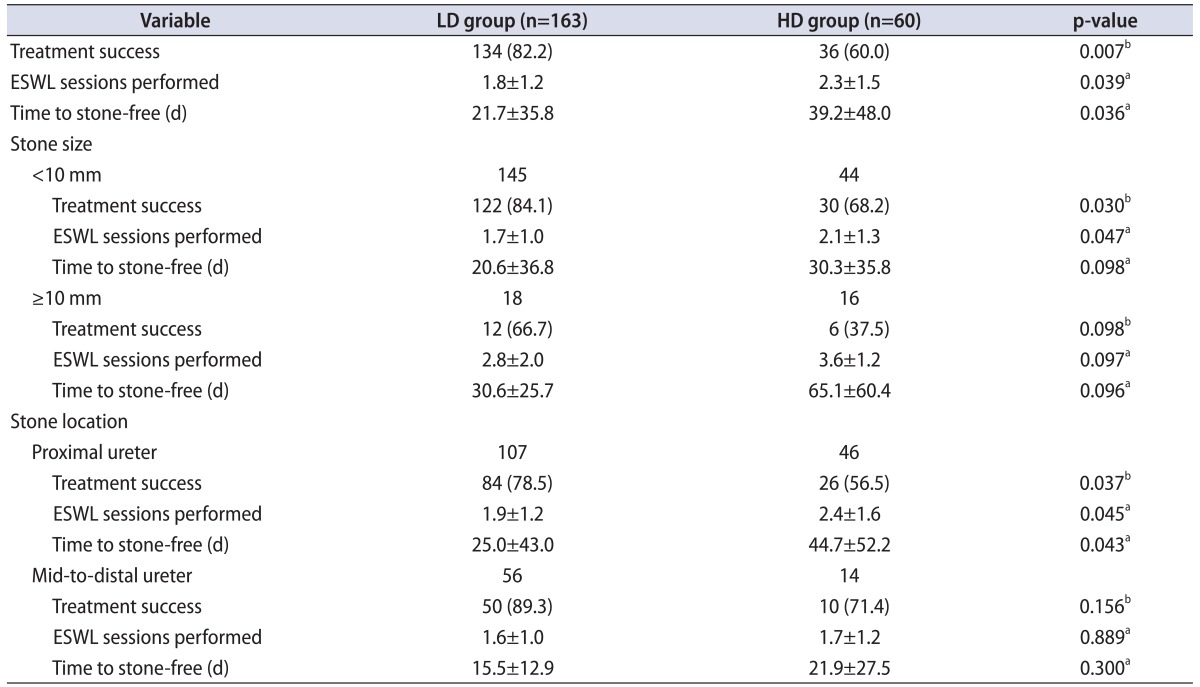
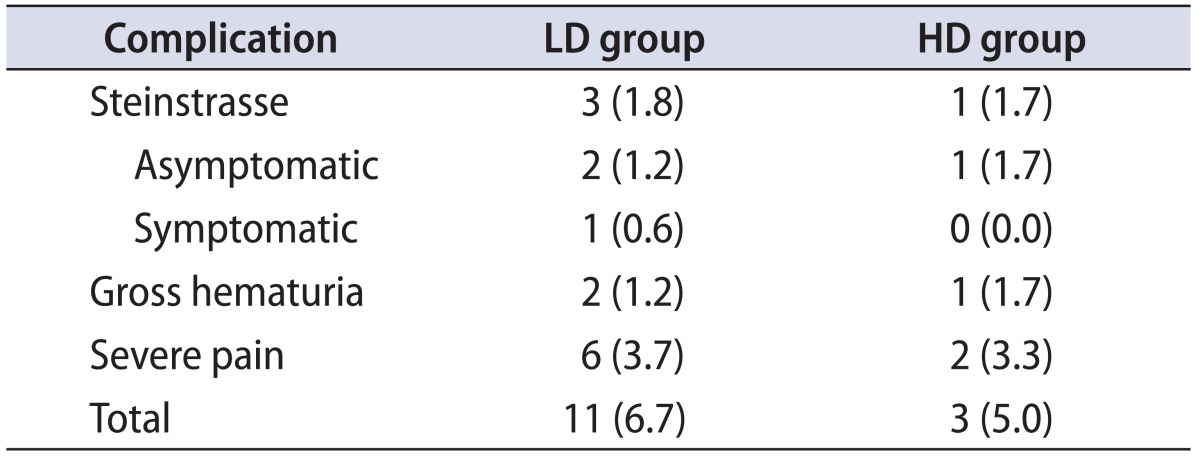
Overall success rates in the LD and HD groups were 82.1% and 60.0%, respectively (p=0.007). Mean time to SF status and the average number of SWL sessions required for success in the two groups were 21.7±35.8 days compared with 39.2±48.0 days and 1.8±1.2 compared with 2.3±1.5, respectively (p=0.036 and p=0.039, respectively). In the subgroup analysis divided by stone size and stone location, significant differences in the analysis of patients with smaller stone or proximal ureter stone were found between the groups (Table 2). Post-ESWL complication rates were comparable between the two groups (Table 3).
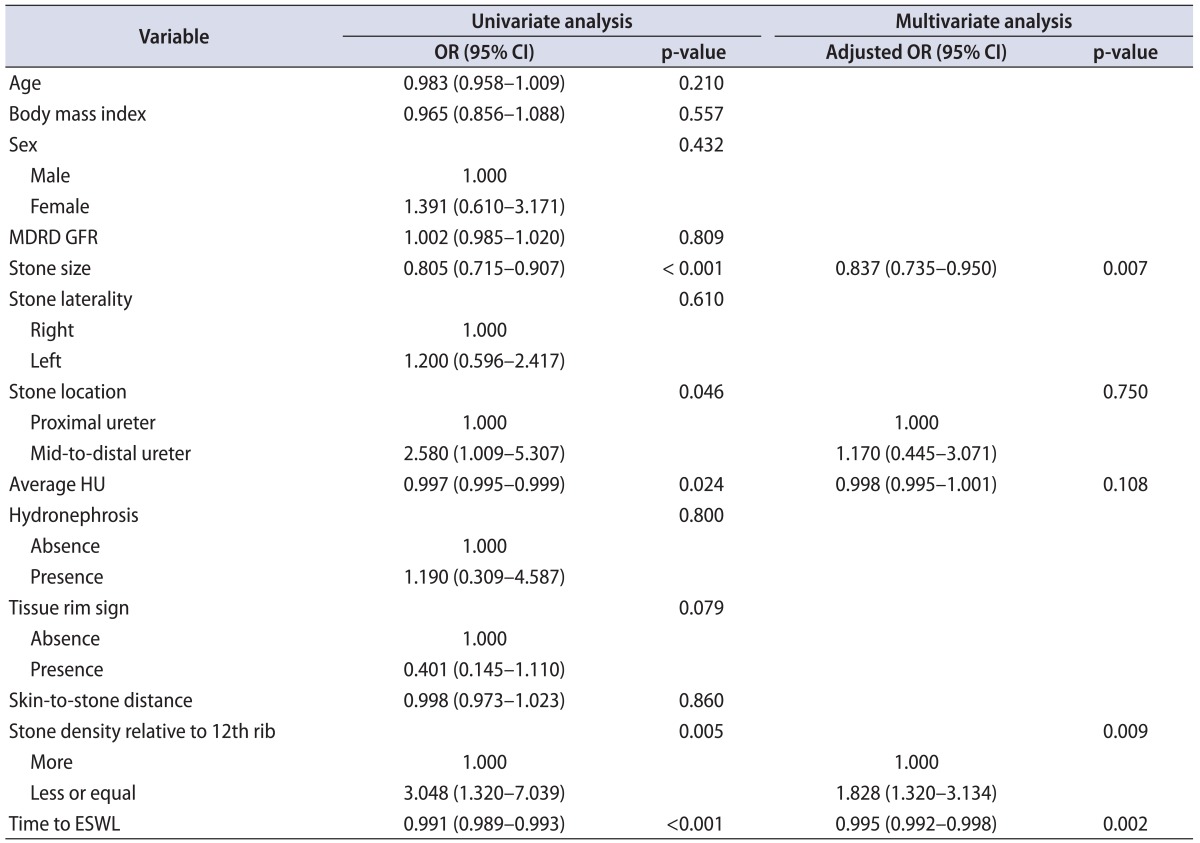
On univariate logistic analysis, stone size, location (mid-to-distal ureter compared with proximal ureter), time to ESWL, and average HU and stone densities were significantly associated with ESWL success. On multivariate analysis, stone size, time to ESWL, and stone density were independent predictors of successful ESWL (Table 4).
In the propensity-score matching analysis, there was no significant difference in the baseline characteristics between the two groups, except for the average HU density (Table 1). The success rates of ESWL in the LD and HD groups were 78.3% and 60.0%, respectively (p=0.027). Mean time to SF status and the average number of SWL sessions required for success in the two groups were 22.3±24.7 days compared with 39.2±48.0 days and 1.9±1.3 compared with 2.3±1.5, respectively (p=0.043 and p=0.046, respectively). However, the subgroup analysis divided by stone size and stone location was not performed because the sample size was relatively small for accurate analysis.
Since the 1980s, ESWL has been established as the preferred method for treating ureteric calculi, due to its minimally invasive character, no requirement for anesthesia, and low morbidity [9]. The outcome of ESWL depends on many factors, including stone size, location, composition, radiological characteristics, type of shockwave generator, and the presence of obstruction or infection [2]. Of these factors, the fragility of stone is correlated with stone composition and effective transmission of shockwave energy [10]. It is well known that calcium oxalate monohydrate, cysteine, and brushite stones are hard and resistant to ESWL [11]. Several trials are currently evaluating the relationship between radiological characteristics and stone composition [12]. Recently, some studies have investigated stone composition by using radiological data such as dual-energy CT, but this modality is still experimental [13].
Stone composition is related to the attenuation value in radiological modalities. Many studies tried to ascertain that the attenuation value of calculi would predict stone fragility. The attenuation value is measured in two ways: HU density by NCCT and radiodensity by KUB [14]. Increasing evidence suggests that stone measurement by NCCT can help to predict treatment outcomes of ESWL [15]. The density of stone varies with its composition and affects the fragility of calculus, which ultimately governs the clinical outcome of ESWL. Shah et al. [16] found that the number of shocks required for stone fragmentation increases as the HU density of calculus increases. In addition, the mean intensity of shock impulses sufficient enough to clear stone is proportional to the HU density of the stone [16]. Bandi et al. [17] reported that peak HU density and mean HU density can predict SWL success on univariate analysis. HU density was shown to be intensely related with ESWL success and was significantly associated in our data [18,19].
Radiodensity on plain x-ray tends to be higher, because it is increasing in HU density [20]. In our data, mean HU density scores were significantly different between the two groups that were divided by radiodensity. Several studies about stone density measured by KUB and ESWL results have been conducted. Dretler [6] proposed the ability of a plain KUB to indicate stone fragility on the basis of radiographic patterns. Bon et al. [7] found that calculi that appeared denser than bone (12th rib or transverse process) responded poorly to SWL. Aeberli et al. [21] did not find a correlation between stone density and stone fragility; however, the analysis was not stratified by stone size. In our study, stone density relative to that of bone on KUB was an independent predictor of ESWL failure, and the patients with a stone density equal to or lower than that of bone on KUB had a relatively higher probability of ESWL success than did those with a density higher than that of bone. Furthermore, HU density and radiodensity were strongly correlated.
Stone contour is an important factor for renal stone fragmentation. In the study by Bon et al. [7], stone contour in the SF group was predominantly rough (63.5%) and had a density lower than or equal to that of bone (71%), whereas calculi in the non-SF series were most often smooth (57.3%) and denser than bone (57.8%). However, our data showed no difference in success rates on the basis of surface contour. We thought that this discrepancy was due to stone location. In the study by Bon et al. [7], most stones were renal stones (94.2%), and the total SF rate was lower than that in our study (54%). We evaluated ureteral stones and excluded renal stones; we found higher SF rates and concluded that stone surface was not a predictive factor.
Stone location in the ureter has been found to be a contributing factor to ESWL success [5]. In our study, we found a significant difference in ESWL success rates, in the number of ESWL sessions, and in the time to SF status in proximal ureter stone, but not in mid- and distalureter stone. Generally, SF rates tend to be lower in the proximal ureter than in the lower ureter [5]. Therefore, the proximal ureter stones were more affected by stone density. This result is not completely understood; however, the relatively greater frequency of stones in the proximal ureter could be a contributing factor.
Stone size was considered to be an ESWL-success indicator in many studies. Ng et al. [15] showed that greater stone volume and mean stone density were significant predictors of a lower SF rate. The optimal cutoff points were stone volume at 0.2 mL, mean stone density at 593 HU, and SSD at 9.2 cm [15]. In our study, stone size was an independent predictive factor for ESWL success. In the smaller-stone group (diameter less than 10 mm), a difference in SF rates and numbers of sessions was observed. A significant difference in stone location and size was found only in the group (proximal ureter and less than 10 mm in diameter) with more effective results on ESWL.
Our study had several limitations. First, we could not completely control for the subjectivity of the radiologists when they determined the radiodensity of the stones based on KUB. However, we tried to diminish it. Two radiologists evaluated the radiodensity independently. In cases of disagreement, another radiologist made the final decision, which we abided by. Second, the definition of success was not clear, and there was no consensus on it. Thus, we defined success as being SF within 1 month after ESWL. Third, other factors influencing ESWL outcomes, such as massive hydration and natural elimination, were not considered in our analysis. Last, because this review was done retrospectively, bias could have inadvertently been introduced.
In our study, stone density on plain x-ray was correlated with HU density on CT. Stone with a density greater than that of the 12th rib had a relatively higher risk of ESWL failure than did stone with a lower density. Stone density on plain x-ray may be one of independent predicting factors for successful ESWL, together with stone size and time to ESWL. Thus, radiological findings on the preoperative KUB may be helpful for predicting ESWL outcomes. Further well-designed prospective studies with larger cohorts are needed to validate these findings.
References
1. Stamatelou KK, Francis ME, Jones CA, Nyberg LM, Curhan GC. Time trends in reported prevalence of kidney stones in the United States: 1976-1994. Kidney. 2003; 63:1817–1823.
2. Tiselius HG, Ackermann D, Alken P, Buck C, Conort P, Gallucci M, et al. Guidelines on urolithiasis. Eur Urol. 2001; 40:362–371. PMID: 11713390.
3. Tanaka M, Yokota E, Toyonaga Y, Shimizu F, Ishii Y, Fujime M, et al. Stone attenuation value and cross-sectional area on computed tomography predict the success of shock wave lithotripsy. Korean J Urol. 2013; 54:454–459. PMID: 23878688.

4. Pareek G, Hedican SP, Lee FT Jr, Nakada SY. Shock wave lithotripsy success determined by skin-to-stone distance on computed tomography. Urology. 2005; 66:941–944. PMID: 16286099.

5. Preminger GM, Tiselius HG, Assimos DG, Alken P, Buck AC, Gallucci M, et al. 2007 Guideline for the management of ureteral calculi. Eur Urol. 2007; 52:1610–1631. PMID: 18074433.

6. Dretler SP. Stone fragility: a new therapeutic distinction. J Urol. 1988; 139:1124–1127. PMID: 3361657.

7. Bon D, Dore B, Irani J, Marroncle M, Aubert J. Radiographic prognostic criteria for extracorporeal shock-wave lithotripsy: a study of 485 patients. Urology. 1996; 48:556–560. PMID: 8886060.

8. Choi HJ, Jung JH, Bae J, Cho MC, Lee HW, Lee KS. Usefulness of early extracorporeal shock wave lithotripsy in colic patients with ureteral stones. Korean J Urol. 2012; 53:853–859. PMID: 23301130.

9. Wang M, Shi Q, Wang X, Yang K, Yang R. Prediction of outcome of extracorporeal shock wave lithotripsy in the management of ureteric calculi. Urol Res. 2011; 39:51–57. PMID: 20401653.

10. Williams JC Jr, Saw KC, Paterson RF, Hatt EK, McAteer JA, Lingeman JE. Variability of renal stone fragility in shock wave lithotripsy. Urology. 2003; 61:1092–1096. PMID: 12809867.

11. Dretler SP, Polykoff G. Calcium oxalate stone morphology: fine tuning our therapeutic distinctions. J Urol. 1996; 155:828–833. PMID: 8583586.

13. Hidas G, Eliahou R, Duvdevani M, Coulon P, Lemaitre L, Gofrit ON, et al. Determination of renal stone composition with dual-energy CT: in vivo analysis and comparison with x-ray diffraction. Radiology. 2010; 257:394–401. PMID: 20807846.

14. Motley G, Dalrymple N, Keesling C, Fischer J, Harmon W. Hounsfield unit density in the determination of urinary stone composition. Urology. 2001; 58:170–173. PMID: 11489691.

15. Ng CF, Siu DY, Wong A, Goggins W, Chan ES, Wong KT. Development of a scoring system from noncontrast computerized tomography measurements to improve the selection of upper ureteral stone for extracorporeal shock wave lithotripsy. J Urol. 2009; 181:1151–1157. PMID: 19152949.

16. Shah K, Kurien A, Mishra S, Ganpule A, Muthu V, Sabnis RB, et al. Predicting effectiveness of extracorporeal shockwave lithotripsy by stone attenuation value. J Endourol. 2010; 24:1169–1173. PMID: 20575686.

17. Bandi G, Meiners RJ, Pickhardt PJ, Nakada SY. Stone measurement by volumetric three-dimensional computed tomography for predicting the outcome after extracorporeal shock wave lithotripsy. BJU Int. 2009; 103:524–528. PMID: 19007365.

18. Gupta NP, Ansari MS, Kesarvani P, Kapoor A, Mukhopadhyay S. Role of computed tomography with no contrast medium enhancement in predicting the outcome of extracorporeal shock wave lithotripsy for urinary calculi. BJU Int. 2005; 95:1285–1288. PMID: 15892818.

19. Yoshida S, Hayashi T, Ikeda J, Yoshinaga A, Ohno R, Ishii N, et al. Role of volume and attenuation value histogram of urinary stone on noncontrast helical computed tomography as predictor of fragility by extracorporeal shock wave lithotripsy. Urology. 2006; 68:33–37. PMID: 16806419.

20. Huang CC, Chuang CK, Wong YC, Wang LJ, Wu CH. Useful prediction of ureteral calculi visibility on abdominal radiographs based on calculi characteristics on unenhanced helical CT and CT scout radiographs. Int J Clin Pract. 2009; 63:292–298. PMID: 19196367.

21. Aeberli D, Muller S, Schmutz R, Schmid HP. Predictive value of radiological criteria for disintegration rates of extracorporeal shock wave lithotripsy. Urol Int. 2001; 66:127–130. PMID: 11316972.

Fig. 1
Stone density classification compared with the density of the 12th rib: lower (arrow, A), equal (arrow, B), and higher density (arrow, C).

Table 1
Baseline characteristics
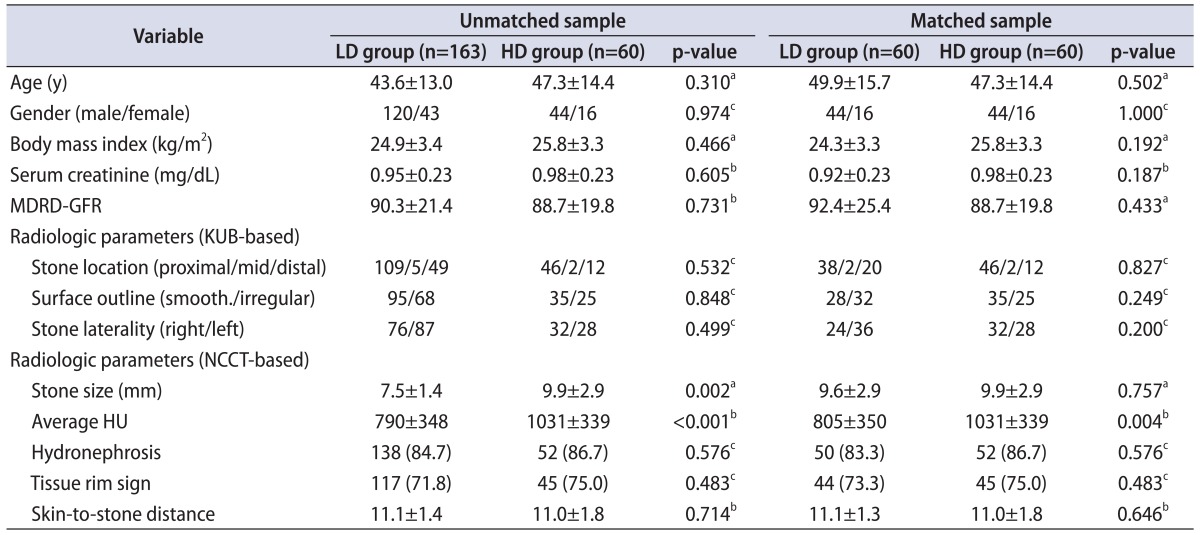
Values are presented as mean±standard deviation or number (%).
LD, lower density; HD, higher density; MDRD GFR, modification of diet in renal disease glomerular filtration rate (calculated using the abbreviated MDRD study equation); NCCT, noncontrast computed tomography; HU, Hounsfield unit.
a:Independent t test. b:Mann-Whitney U test. c:Chi-square test.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download