Abstract
Purpose
Endoscopic treatment (ET) has become a widely accepted procedure for treating vesicoureteral reflux (VUR). However, patients followed up after ET over long periods have reported persistent or recurrent VUR. We evaluated the natural course of failed ET in patients who required further treatments to help physicians in making decisions on the treatment of VUR.
Materials and Methods
We retrospectively reviewed the medical records of patients who were diagnosed with VUR and underwent ET from January 2006 to December 2009. A total of 165 patients with 260 ureters underwent ET. We compared the parameters of the patients according to ET success or failure and evaluated the natural course of the patients after ET failure.
Results
Mean VUR grade and positive photon defect were higher in the failed ET group than in the successful ET group. Six months after the operation, persistent or recurrent VUR was observed in 76 ureters (29.2%), and by 16.3 months after the operation, VUR resolution was observed in 18 ureters (23.7%). Twenty-five ureters (32.9%) without complications were observed conservatively. Involuntary detrusor contraction was found in 1 of 9 (11.1%) among the secondary ET success group, whereas in the secondary ET failure group, 4 of 6 (66.7%) had accompanying involuntary detrusor contraction.
The typical treatment of vesicoureteral reflux (VUR) is to wait for improvement of the reflux with bladder maturation. However, a prerequisite to deciding to wait is the absence of ongoing renal parenchymal damage. To avoid renal damage, patients with VUR must take prophylactic antibiotics, manage constipation, or be periodically checked for urinary tract infection (UTI). Because endoscopic treatment (ET) is simple, has low morbidity, and has the advantage that patients can discontinue antibiotic prophylaxis, it is supported as a first-line treatment for VUR [1,2]. Moreover, ET has replaced most open surgeries owing to its high success rate, simplicity, and convenience [3]. However, ET success is often short-lived [4]. In most studies, the success rate of ET is determined 3 months after surgery. Thus, if follow-up periods were longer, the recurrence rate may be higher. Unlike open or laparoscopic surgery, ET is performed on the assumption that it may fail. Therefore, the natural course after ET failure is essential to choosing the treatment.
Many studies have investigated the causes of failed ET or the effect of performing a second ET on the patient [5,6,7,8,9]. However, studies about the natural course of persistent or recurrent VUR after ET failure are extremely rare. In addition, the role of voiding dysfunction in the resolution of VUR and the success rate of surgical procedures for VUR have been well elucidated [10,11,12]. However, the relationship between bladder overactivity and ET success in VUR is still controversial [10,13].
We evaluated the natural course of VUR after ET failure. Furthermore, we evaluated the relationship between involuntary detrusor contraction (IDC) and resolution of VUR and ET success.
Following Institutional Review Board approval of the study, we retrospectively reviewed the medical records of children diagnosed with VUR who underwent ET from January 2006 to December 2009. The patients had been followed up for more than 1 year after ET. Patients with prior antireflux surgery, duplex system, ureterocele, ectopic ureter, megaureter, neurogenic abnormalities, or structural anomalies of the bladder and urethra were excluded. A total of 165 patients with 260 ureters were included in this study.
All patients underwent urinalysis, ultrasonography, dimercaptosuccinic acid (DMSA) renal scan, and voiding cystourethrography (VCUG). VCUG and DMSA renal scan were performed after the resolution of fever and confirmation of a negative urine culture. VUR was graded by using the system defined by the international Reflux Study Committee [14]. Follow-up ultrasonography was performed at 1 month after ET and we observed the presence or absence of a Deflux (hyaluronic acid/dextranomer) mound (Salix Pharmaceuticals, Raleigh, NC, USA). VCUG and DMSA were performed at 6 months after ET. For patients who had remnant VUR after ET, VCUG was performed every 1 year until spontaneous resolution of VUR.
A urodynamic study (UDS) was performed on all children with prior ET from January 2008. UDS was performed by using Medtronic multi-P cystometry (Duet, Medtronic, Denmark), with a 6-Fr double-lumen urethral catheter and an 8-Fr rectal tube. No patient was placed under sedation. The infusion rate was set at 10% of expected bladder capacity per minute and we used ≥30 mL (30×age in years) to calculate the expected bladder capacity [15]. The temperature of the infusion saline was set to 30℃ and maintained so. Bladder capacity was defined as the volume at which the patients started to void. IDC was defined as any involuntary contraction during the filling phase. Dysfunctional voiding (DV) was defined as an intermittent or fluctuating uroflow rate from involuntary intermittent contractions of the striated muscle of the external urethral sphincter or pelvic floor during voiding [16].
Indications for ET were breakthrough UTI, noncompliance with medication, development of new renal scars, or decreased renal function over grade II VUR. Grade I VUR was treated only when it was associated with contralateral high-grade VUR. To avoid sample bias, the ET group included only patients who received Deflux hyaluronic acid/dextranomer injection.
Patients received general anesthesia before undergoing ET. We used an 8- to 9.8-Fr cystoscope, which facilitated hyaluronic acid/dextranomer injection via a prefilled polycarbonate syringe and cannula (3.5 Fr×35 cm.). Surgical procedures were performed on a case-by-case basis at the discretion of the surgeon by the subureteric transurethral injection (STING) method or hydrodistention-implantation technique (HIT). The success of ET was determined at 6 months after surgery. Success was defined as no VUR or grade I VUR on VCUG.
Statistical analyses were performed by using IBM SPSS Statistics ver. 19.0 (IBM Co., Armonk, NY, USA). We compared variables by using Student t-test, the chi-square test, and Fisher exact test. A p-value of less than 0.05 was considered statistically significant.
The patients' mean age at diagnosis was 22.34±26.62 months (range, 0.9-96 months). The mean VUR grade was 2.76±0.94. Photon defects were seen in 96 kidney units (36.9%).
According to the results of the VCUG performed 6 months after ET, we divided patients into two groups: success or failure. ET success was seen in 184 of 260 ureters (70.8%). There were no significant differences in sex, laterality, or febrile UTI between the two groups. However, the preoperative VUR grade was 2.59±0.95 in the success group and 3.19±0.80 in the failure group (p=0.012). Photon defects were seen in 61 kidney units (33.1%) in the success group and in 35 units (46.1%) in the failure group (p=0.05). The indications for ET were breakthrough UTI (n=241), noncompliance with medication (n=7), and decreased renal function or newly developed renal scarring (n=12). There was no significant difference between the success and failure groups in the indications for ET (p=0.302). The mean injected volume of hyaluronic acid/dextranomer was not significantly different between the success and failure groups: 0.97±0.52 and 1.16±0.64, respectively (p=0.42). When the mound morphology was a volcano shape, ET success was observed in 78.7% of cases. The percentage of material mound seen in postoperative ultrasonography was significantly different in the success and failure groups (p=0.002) (Table 1).
Those with a higher grade VUR had a lower ET success rate. The success rates, according to reflux grade, were 100% (26/26), 79.7% (55/69), 66.4% (73/110), 57.1% (28/49), and 33.3% (2/6) for grades I to V, respectively.
In cases in which UDS was performed, IDC was observed in 35 of 163 ureters (21.4%), but IDC did not show a significant correlation with ET success. The mean maximum cystometric capacity, maximum detrusor pressure at voiding, postvoiding residual urine volume, and the number of cases of DV were also not significantly different between the success and failure groups (Table 2).
Postoperative UTI was observed in 5% of the ET success group and 52% of the ET failure group. Persistent VUR was observed in 76 ureters (29.2%) after ET. Among these, 43 ureters (56.6%) were treated conservatively and 33 ureters (43.4%) required surgical treatment. Fifty-two of the 76 ureters (68.4%) were observed to have a downgrading of VUR, based on comparisons between preoperative VCUG. In 18 ureters (23.7%), VUR resolution was observed at a mean time of 16.3 months after ET; the other 25 ureters (32.9%) were followed up with conservative treatment. For the conservative treatment group after ET failure, the mean VUR grade decreased from 3.13±0.19 to 2.04±0.04. In the conservative treatment group after ET failure, volcano shape mounds were seen in 77.2% (Table 3).
The results of Kaplan-Meier survival analysis showed that the resolution time of VUR in the ET group was significantly shorter than in the conservative treatment groups (9.27±0.75 months for the ET group, 18.8±0.97 months for the conservative treatment group, p<0.001). The conservative treatment group included 309 ureters diagnosed with VUR and followed up conservatively in our hospital in the same follow-up period. In looking at the curve of VUR resolution in the ET failure group, VUR resolution occurred at 21.01±2.36 months after ET, which was not significantly different from the 18.8±0.97 months for the conservative treatment group (p=0.42) (Fig. 1).
In cases with secondary surgical treatment who suffered a recurrent febrile UTI, newly developed renal scar, or decreased renal function after ET failure, secondary ET was performed in 19 ureters and ureteral reimplantation was performed for 14 ureters. When newly developed renal scarring or decreased renal function was observed, we performed ureteral reimplantation rather than a secondary ET. The mean time to a secondary operation was 12.8 months (range, 5-32 months) after ET. The success rate of secondary ET was 68.4%. Among six ureters with failed secondary ET, two were followed up conservatively and the other four underwent ureteral reimplantation (Fig. 2).
In cases with available UDS from the ET failure group, IDC was observed in 2 of 37 ureters (5.4%) in the conservative treatment group and in 7 of 27 (25.9%) in the secondary procedure group (p=0.025) (Table 3). IDC was found in 1 of 9 ureters (11.1%) among the secondary ET success group, whereas in the secondary ET failure group, 4 of 6 (66.7%) had accompanying IDC.
ET was first described by Matouschek [17], O'Donnel and Puri [18], who further popularized this method. Stenberg and Lackgren [19] were the first to describe the application of Deflux hyaluronic acid/dextranomer. Enthusiasm for this material, which culminated in its approval by the U.S. Food and Drug Administration, increased the rate of development of the product. Since the mid-2000s, ET has been used in 88% of surgical interventions for VUR [3]. Numerous reports have investigated hyaluronic acid/dextranomer injections in the context of primary VUR and redo cases, highlighting the efficacy of the procedure. Recently, Kirsch et al. [20] presented a hydrodistention modification that yielded cure rates as high as 92% for primary low-grade VUR.
However, Lee et al. [4] concluded that ET success might be temporary and that long-term follow-up is necessary, even though post-ET VCUG does not show VUR. In their series of reports, an initial success rate (6 to 12 weeks) of 73% was found, but after 1 year of follow-up, they found 39 of 150 ureters had recurring VUR with an overall success rate of 46%. Sedberry-Ross et al. [6] reported that 12 of 45 (27%) of their ET success patients had a febrile UTI on long-term follow-up and 10 of 12 (92%) of these were found to have a recurrence of VUR. Like this study, many studies reported that mound morphology, preoperative VUR grade, and material presence on postoperative ultrasonography were factors predicting ET success [21,22,23]. In most studies, ET success was judged by VCUG after 3 months of ET, and patients discontinued taking antibiotics after confirmation of success [24,25]. However, we performed VCUG 6 months after ET and prophylactic antibiotics were discontinued immediately after ET. We deferred postoperative VCUG to 6 months after ET because we have not seen febrile UTIs develop between 3 and 6 months after ET. A longer interval between ET and post-ET VCUG is more effective in determining whether ET is successful. In our study, we found a 70.8% success rate of ET, which is not inferior to other series using VCUG within 3 months after ET.
We regard it difficult to evaluate the result of ET in the management of VUR owing to the characteristics of VUR. VUR can spontaneously resolve with time, although VUR of grade V generally needs surgical correction. For the cases that reported the disappearance of VUR after ET, this finding may be the result of a natural resolution of VUR rather than a therapeutic effect of ET. In other words, persistent or recurrent VUR may also resolve without further treatment if febrile UTI does not occur. In many studies, when ET failure was observed, repeat ET was considered [8,26]. In our study, 18 of the 76 ureters (23.7%) with persistent VUR at 6 months after ET reported VUR resolution an average of 16.3 months after ET. The other 25 ureters (32.8%) were treated conservatively. This showed that some cases did not require additional surgical treatment even with ET failure. The Kaplan-Meier survival curve showed that the curve of the natural course after ET failure was not worse than the spontaneous resolution curve for VUR, 21.01±2.36 and 18.8±0.97 months, respectively (p=0.42).
Many studies have shown that the success rate of ET differs according to whether the STING or HIT method is used [20,22]. In this study, the success rate was higher with HIT than with STING. However, HIT (6 ureters) and double HIT (6 ureters) was performed in only 12 ureters (4.6%); STING was performed in most ureters (248 ureters, 95.4%). Therefore, we did not compare the success rate according to the method used.
In many studies, voiding dysfunction is thought to be the causal factor for VUR as well as the main factor affecting VUR progress [10,11,12]. Before children reach the age of bladder control, most studies show that low-capacity, high voiding pressure and incoordination at voiding are normal findings [27,28]. Most patients in the present study were younger than the age of bladder control; thus, their IDCs were unlikely to be pathological but could have affected VUR. IDC was not associated with ET success in this study; however, the secondary procedure rate was higher in the IDC-positive group (25.9%) than in the IDC-negative group (5.4%). That is, IDC did not influence ET success but indirectly increased the need for a secondary procedure through other factors like febrile UTI and further renal damage. Furthermore, IDC was seen more frequently in cases in the secondary ET failure group (failure in 66.7% vs. success in 11.1%). One possible explanation for the discrepancy between the role of IDC in the first and second ET might be that there are two types of IDC that are pathologic: one affecting VUR and the other not.
In this study, DV did not influence the success or failure of the initial ET. Regretfully, we could not evaluate whether DV affects the success rate of the second ET owing to the small number of patients. Higham-Kessler et al. [5] reported that DV might not influence the success or failure of the initial ET but could be a factor in a second ET (44% DV vs. 14% normal voiding on second injection). Therefore, we recommend that it is unnecessary to perform pre-ET UDS, but that UDS is essential in deciding whether to perform a secondary procedure after the initial ET failure.
A limitation of this study was its retrospective design. In cases with remnant VUR, when breakthrough UTI or decreased renal function occurred, we were not able to exclude the possibility that a secondary procedure would have been necessary after ET failure among patients in the conservative treatment group. Also, we could not distinguish the two types of pathologic IDC. We suggest that a prospective, large-scale study will be needed to clarify this matter in the future.
We suggest that ET-failed patients can be observed for spontaneous resolution of VUR unless they have febrile UTI or decreased renal function. We also suggest that UDS can be helpful in deciding whether a secondary procedure after ET failure is necessary. In cases with IDC, when patients need a secondary procedure, we recommend open or laparoscopic surgery instead of ET.
Figures and Tables
Fig. 1
Vesicoureteral reflux (VUR) resolution curve. VUR resolution occurred in 21.01±2.36 months after endoscopic treatment (ET), which was not significantly different from 18.8±0.97 months for the conservative treatment group (p=0.42). Number of patients in each group: conservative treatment (Tx) group (n=309), ET group (n=260), and ET failure group (n=76).
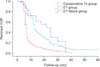
Fig. 2
Algorithm of treatment for failed endoscopic treatment (ET). A secondary procedure was performed in cases of recurrent febrile urinary tract infection or newly developed renal scarring or a decrease in renal function after ET failure. When a newly developed renal scar or decreased renal function was observed, we performed ureteral reimplantation rather than secondary ET.

Table 1
Characteristics of the ET success versus the ET failure group

Table 2
Comparison of the urodynamic parameters between the ET success and ET failure groups

Table 3
Characteristics of the conservative treatment group versus the secondary procedure group after ET failure

References
1. Lackgren G, Wahlin N, Skoldenberg E, Stenberg A. Long-term followup of children treated with dextranomer/hyaluronic acid copolymer for vesicoureteral reflux. J Urol. 2001; 166:1887–1892.
2. Elder JS, Shah MB, Batiste LR, Eaddy M. Part 3: Endoscopic injection versus antibiotic prophylaxis in the reduction of urinary tract infections in patients with vesicoureteral reflux. Curr Med Res Opin. 2007; 23:Suppl 4. S15–S20.
3. Molitierno JA, Scherz HC, Kirsch AJ. Endoscopic treatment of vesicoureteral reflux using dextranomer hyaluronic acid copolymer. J Pediatr Urol. 2008; 4:221–228.
4. Lee EK, Gatti JM, Demarco RT, Murphy JP. Long-term follow-up of dextranomer/hyaluronic acid injection for vesicoureteral reflux: late failure warrants continued followup. J Urol. 2009; 181:1869–1874.
5. Higham-Kessler J, Reinert SE, Snodgrass WT, Hensle TW, Koyle MA, Hurwitz RS, et al. A review of failures of endoscopic treatment of vesicoureteral reflux with dextranomer microspheres. J Urol. 2007; 177:710–714.
6. Sedberry-Ross S, Rice DC, Pohl HG, Belman AB, Majd M, Rushton HG. Febrile urinary tract infections in children with an early negative voiding cystourethrogram after treatment of vesicoureteral reflux with dextranomer/hyaluronic acid. J Urol. 2008; 180:4 Suppl. 1605–1609.
7. Mendez R, Somoza I, Tellado MG, Liras J, Sanchez A, Pais E, et al. Predictive value of clinical factors for successful endoscopic correction of primary vesicoureteral reflux grades III-IV. J Pediatr Urol. 2006; 2:545–550.
8. Alkan M, Ciftci AO, Senocak ME, Tanyel FC, Buyukpamukcu N. Endoscopic treatment of vesicoureteral reflux in children: our experience and analysis of factors affecting success rate. Urol Int. 2008; 81:41–46.
9. Lee DW, Kang KM, Oh WS, Kim JS, Chung SK. Risk factors for treatment failure after endoscopic subureteral injection of dextranomer/hyaluronic acid copolymer (Deflux(R)) for vesicoureteral reflux. Korean J Urol. 2009; 50:61–66.
10. Taylor CM, Corkery JJ, White RH. Micturition symptoms and unstable bladder activity in girls with primary vesicoureteric reflux. Br J Urol. 1982; 54:494–498.
11. Koff SA, Murtagh DS. The uninhibited bladder in children: effect of treatment on recurrence of urinary infection and on vesicoureteral reflux resolution. J Urol. 1983; 130:1138–1141.
12. Yeung CK, Sreedhar B, Sihoe JD, Sit FK. Renal and bladder functional status at diagnosis as predictive factors for the outcome of primary vesicoureteral reflux in children. J Urol. 2006; 176:1152–1156.
13. Kraft KH, Molitierno JA Jr, Dewhurst L, Geers C, Gunderson K, Scherz HC, et al. Is endoscopic injection therapy a reasonable treatment option for low-grade vesicoureteral reflux in association with overactive bladder? Urology. 2011; 78:675–678.
14. Medical versus surgical treatment of primary vesicoureteral reflux: report of the International Reflux Study Committee. Pediatrics. 1981; 67:392–400.
15. Koff SA. Estimating bladder capacity in children. Urology. 1983; 21:248.
16. Neveus T, von Gontard A, Hoebeke P, Hjalmas K, Bauer S, Bower W, et al. The standardization of terminology of lower urinary tract function in children and adolescents: report from the Standardisation Committee of the International Children's Continence Society. J Urol. 2006; 176:314–324.
17. Matouschek E. New concept for the treatment of vesico-ureteral reflux. Endoscopic application of teflon. Arch Esp Urol. 1981; 34:385–388.
18. O'Donnell B, Puri P. Treatment of vesicoureteric reflux by endoscopic injection of Teflon. 1984. J Urol. 2002; 167:1808–1809.
19. Stenberg A, Lackgren G. A new bioimplant for the endoscopic treatment of vesicoureteral reflux: experimental and short-term clinical results. J Urol. 1995; 154(2 Pt 2):800–803.
20. Kirsch AJ, Perez-Brayfield M, Smith EA, Scherz HC. The modified sting procedure to correct vesicoureteral reflux: improved results with submucosal implantation within the intramural ureter. J Urol. 2004; 171(6 Pt 1):2413–2416.
21. Lavelle MT, Conlin MJ, Skoog SJ. Subureteral injection of Deflux for correction of reflux: analysis of factors predicting success. Urology. 2005; 65:564–567.
22. Yucel S, Gupta A, Snodgrass W. Multivariate analysis of factors predicting success with dextranomer/hyaluronic acid injection for vesicoureteral reflux. J Urol. 2007; 177:1505–1509.
23. Kajbafzadeh AM, Tourchi A, Aryan Z. Factors that impact the outcome of endoscopic correction of vesicoureteral reflux: a multivariate analysis. Int Urol Nephrol. 2013; 45:1–9.
24. Puri P, Chertin B, Velayudham M, Dass L, Colhoun E. Treatment of vesicoureteral reflux by endoscopic injection of dextranomer/hyaluronic Acid copolymer: preliminary results. J Urol. 2003; 170(4 Pt 2):1541–1544.
25. Chi A, Gupta A, Snodgrass W. Urinary tract infection following successful dextranomer/hyaluronic acid injection for vesicoureteral reflux. J Urol. 2008; 179:1966–1969.
26. Capozza N, Lais A, Matarazzo E, Nappo S, Patricolo M, Caione P. Influence of voiding dysfunction on the outcome of endoscopic treatment for vesicoureteral reflux. J Urol. 2002; 168(4 Pt 2):1695–1698.
27. Bachelard M, Sillen U, Hansson S, Hermansson G, Jodal U, Jacobsson B. Urodynamic pattern in asymptomatic infants: siblings of children with vesicoureteral reflux. J Urol. 1999; 162:1733–1737.
28. Jansson UB, Hanson M, Hanson E, Hellström AL, Sillen U. Voiding pattern in healthy children 0 to 3 years old: a longitudinal study. J Urol. 2000; 164:2050–2054.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download