This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
Various articles have previously addressed the introduction of new surgical laser therapies for an enlarged prostate gland causing obstructive symptoms. The objective of this study was to report the feasibility of performing the thulium laser vapo-enucleation of the prostate (ThuVEP) procedure for benign prostatic obstruction in a 1-day surgery.
Materials and Methods
From September 2011 to September 2013, we conducted a prospective study on patients who underwent ThuVEP in a 1-day surgery. The primary outcomes measured perioperatively included operative time, resected tissue weight, hemoglobin decrease, transfusion rate, postoperative irrigation and catheterization time, and postoperative hospital stay. Also, the preoperative and postoperative International Prostate Symptom Score (IPSS) and results of uroflowmetry performed on the 7th and 30th postoperative days were recorded. All perioperative and postoperative complications were monitored.
Results
A total of 53 patients underwent the surgical treatment in a 1-day surgery. Seven patients continued antiaggregant therapy with aspirin. Mean preoperative prostatic adenoma volume was 56.6 mL. Mean operative time was 71 minutes. The average catheter time was 14.8 hours. The peak urinary flow rate on day 7 improved from 9.3 to 17.42 mL/s (p<0.001) and the IPSS improved from 18 to 10.2 (p<0.01). Patients were routinely discharged on the day of catheter removal. No complications were recorded.
Conclusions
ThuVEP can be safely conducted as a 1-day surgical procedure. This strategy results in cost savings. ThuVEP shows good standardized outcomes with respect to improvement in flow parameters and length of bladder catheterization.
Keywords: Lasers, Prostate, Prostatic hyperplasia, Thulium
INTRODUCTION
Transurethral resection of the prostate (TURP) is considered the reference standard in the surgical therapy of symptomatic bladder outlet obstruction (BOO) secondary to benign prostatic hypertrophy (BPH) between 30 and 80 mL [
1].
Recently, various studies have dealt with the introduction of new surgical laser therapy techniques for treating an enlarged prostate gland causing obstructive symptoms [
2,
3,
4,
5]. Laser prostatectomy has become increasingly popular owing to reduced peri- and postoperative morbidity, shorter catheterization and hospitalization times, and the ability to treat patients with bleeding disorders or those who are taking anticoagulative drugs.
A recent technological advance in the surgical treatment of BOO is the thulium laser. This new surgical laser may have several advantages over other lasers, including improved spatial beam quality, more precise tissue incision, and operation in continuous wave and pulsed modes [
6]. Since its first use, the thulium laser has proved capable of rapid vaporization and coagulation of prostate tissue [
6].
"One-day surgery" is a hospitalization involving the patient's accommodation on the day of surgery only. "Day surgery" is not a subspecialty, but represents a new operating model that enables rationalization of surgical activity. If properly applied, this discipline allows the treatment of relevant and common diseases with both effectiveness and efficiency.
The objective of this study was to report the feasibility of performing thulium laser vapo-enucleation of the prostate (ThuVEP) for benign prostatic obstruction in a 1-day surgery.
MATERIALS AND METHODS
1. Patient selection
A prospective study was conducted from September 2011 to September 2013 on patients who underwent ThuVEP as a 1-day surgery. The study was approved by our Institutional Review Board. All candidates for surgical therapy presented with lower urinary tract symptoms due to prostate gland enlargement.
All patients had lower urinary tract symptoms that were refractory to medical management. According to international guidelines, the following complications were also considered strong indications for surgery: refractory urinary retention, recurrent urinary infection, recurrent hematuria refractory to medical treatment with 5-alpha reductase inhibitors, renal insufficiency due to BPH, and bladder stones [
1]. Prostate carcinoma was ruled out by prostate-specific antigen measurement, digital rectal examination, transrectal ultrasonography, and biopsies when necessary. Patients with prostate carcinoma were excluded from the study, as were those with concomitant urethral strictures and bladder tumors and those with a history of urethral or prostatic surgery. Written consent was obtained from each patient.
2. Surgical technique
Thulium laser prostatectomy was performed by use of a Quanta Cyber TM Thulium Laser (Quanta System, Olona, Italy). The operative technique adopted for ThuLEP was that described by Herrmann et al. [
7] in 2010. All patients were in the lithotomy position, and epidural or general anesthesia was achieved. This technique included five steps: semicircumferential incision of the verumontanum, incision to reach the prostatic capsule at 5 and 7 o'clock and removal of the median lobe, apical incision of the lateral lobes, removal of the lateral lobes, and morcellation (
Video clip, Supplementary material). The level of tissue dissection was between the adenomatous tissue and the prostatic capsule. The result was an open prostatic fossa. A Quanta Cyber TM Thulium:YAG (Quanta System) laser was used at three different energy levels: 120 W for incision and enucleation, 70 W for coagulation of the large capsular artery, and 150 W for vaporization of small residues of adenoma at the end of the procedure. Laser energy was transmitted through an 800-µ laser fiber that could be reused 15 times.
A Wolf resectoscope (Richard Wolf GmbH, Knittlingen, Germany) with a separate operative channel for the fiber was used with a 10° optic. Isotonic saline solution (NaCl 0.9%) at room temperature was used for irrigation. Morcellation was performed by use of a Wolf 2303 Power Stick morcellator drawn toward the blades by suction with a Wolf Piranha 2208 suction peristaltic pump. The use of a morcellator allows the retrieval of tissue to a specimen container suitable for histologic analysis. A standard three-way 20-Fr Foley catheter was routinely used. Irrigations were stopped in the first postoperative day and catheters were removed after 2 hours if the urine color was satisfactorily light. All patients were kept in the hospital for 2 hours after catheter removal and were then discharged.
3. Data analysis
Perioperatively, the primary outcomes measured included operative time (time that the resectoscope sheath was within the urethra), resected tissue weight (actual weight of tissue retrieved), hemoglobin decrease (determined as the difference between pre- and postoperative hemoglobin concentration), transfusion rate, postoperative irrigation and catheterization time, and postoperative hospital stay. Also, the preoperative and postoperative International Prostate Symptom Score (IPSS) and the results of uroflowmetry performed on the 7th and 30th postoperative days were recorded. All perioperative and postoperative complications were monitored.
Data were presented by using means and standard deviations, medians and quartiles, and minimum and maximum recorded values. A paired t-test was used to test the hypothesis of no change between repeated measurements in time for all the considered variables, such as day peak urinary flow between the 7th and 30th postoperative days and preoperative and postoperative IPSS.
RESULTS
A total of 53 patients underwent surgical treatment in a 1-day surgery.
Table 1 lists the baseline characteristics of the men. Seven patients continued antiaggregant therapy with aspirin. The patients' mean age was 71.8 years. Mean preoperative prostatic adenoma volume, as measured by transrectal ultrasonography, was 56.6 mL. Mean maximal flow rate (Qmax) was 9.3 mL/s. Six of the patients had an urethral catheter. All procedures were performed under spinal anesthesia. Prophylaxis with second-generation cephalosporin was performed. Only a mild analgesic (paracetamol 1000 mg) was administered in the postoperative period according to patient demand.
Perioperative data are listed in
Table 2. Mean total operative time, including cystoscopy, enucleation, and morcellation, was 71 minutes. An average of 27.5 g of tissue was retrieved, although it must be kept in mind that tissue retrieval was underestimated owing to the initial significant amount of vaporization during the procedure.
The average Foley catheter time was 14.8 hours. Patients were routinely discharged the same day as catheter removal. Mean hospital stay was 1 day. Pathological assessment revealed no patients with incidental adenocarcinoma of the prostate. No complications were recorded during the immediate or short-term postoperative course. None of the patients showed intra- or postoperative bleeding requiring blood transfusions.
The improvement in Qmax and decrease in IPSS were statistically significant. The peak urinary flow rate on day 7 improved from 9.3 to 17.42 mL/s (7.5-35.3 mL/s) (p<0.001) and IPSS improved from 18 to 10.2 (p<0.01). On day 30, the peak urinary flow rate improved to 19.6 mL/s (8-51.8 mL/s) (p<0.001) and IPSS improved to 6.5 (p<0.001). Mean hemoglobin loss was 1.1 mg/dL.
Eight patients presented with irritative symptoms that resolved completely in the first week after surgery. Five of these patients had a ureteral catheter placed before surgery.
Mean follow-up was 14 months (range, 1-24 months). None of the patients required readmission or urgent urological evaluation after discharge. No patients presented with long-term complications requiring reintervention. No urethral stenoses were observed. No sclerosis of the prostatic fossa or of the bladder neck was observed.
DISCUSSION
"Day surgery" represents an innovative operating model that enables rationalization of surgical activity, better management of human resources, and the containment of health care costs. If properly planned and applied, this discipline allows the treatment of relevant disease with effectiveness and efficiency. The many expected benefits begin with a lower risk of hospital infections and thromboembolism and extend to psychological benefits linked to an early return home and the rapid resumption of activities.
In the past decade, various new technologies have been developed in the transurethral treatment of BOO in an effort to decrease the existing morbidity of TURP. The disadvantages of TURP include the need for bladder catheterization and prolonged washout. The possible complications include catheter blockage by blood clots or unevacuated prostate chips, lower urinary tract infections, hemorrhage requiring transfusion, extraperitoneal fluid collection, and subtrigonal catheter displacement. TURP syndrome (fluid reabsorption with hyponatremia and toxic effects of mannitol), although rare, is a major complication.
The cost of TURP and its associated morbidity are important factors in decision-making and in choosing between different surgical options. The length of hospital stay represents one of the major costs of TURP, especially for prostates with a large volume [
8].
In this clinical picture, laser treatment of benign prostatic enlargement is gaining international acceptance in daily urologic practice. In particular, Greenlight vaporization (PVP, or photoselective vaporization) and holmium laser enucleation (HoLEP) have been studied intensively and challenge the widely accepted treatment option of TURP [
6].
If we reflect on this trend, however, a question arises. Why do we say that TURP is the standard of care? This is the only technique that urologist have had in their hands for the past several years. Thus, in previous literature, no studies have been performed to compare this "standard" with other endoscopic surgical strategies and energy. Laser energy and its new application in endourology offers a new point of discussion and a new strategy for treating BPH. Now and in the future we could change this standard of care.
The thulium laser is a new type of surgical laser that has recently been applied in urology. Its initial advantage is that the center wavelength of the laser is tunable between 1.75 mm and 2.22 mm, allowing the wavelength to exactly match the 1.92-mm water absorption peak in tissue [
8]. Higher absorption of the laser radiation at the thulium wavelength results in more efficient and rapid tissue cutting [
9]. At the same time, it causes a smaller thermal damage zone in the tissue. The incision in tissue is clear and smooth. Thereby, the surgeon can cut at the desired point and is not as dependent on finding the exact layer of the surgical capsule between the adenoma and peripheral zone as a surgical pathway at the very beginning of the procedure.
Furthermore, attempts at early catheter removal owing to the ablation and hemostasis obtained with this laser, and thus the resolution of BOO in a day surgery, have made this an ideal treatment.
This concept of prostate surgery has been made possible through improvements in instrumentation, anesthetic management during and after surgery, and increased experience with new laser techniques. The advent of ThuVEP has revolutionized the concept of the surgical treatment of BPH. ThuVEP combines the best features of previous laser prostatectomy technologies, including minimum complications and morbidity, with the efficacy and immediacy of voiding outcomes associated with conventional TURP, while eliminating the shortcomings of earlier lasers [
10].
This study has presented the initial results of ThuVEP performed as a 1-day surgical procedure, showing significant short-term relief of obstructive symptoms in patients with symptomatic benign prostatic obstruction. This experience shows that ThuVEP is a relatively bloodless surgery that results in a brief catheterization and hospital stay (overnight), immediate symptomatic improvement, and minimal irritative symptoms.
Although no patient in the present study was discharged with the catheter in place, there was no significant morbidity related to early catheter removal.
Finally, there are some considerations about cost. Interestingly, several studies have shown that laser therapy, such as HoLEP and GreenLight PVP, have a significant cost advantage compared with TURP mainly because of shorter hospitalizations and less morbidity [
11,
12]. In our experience, ThuVEP also offers significant improvements over TURP in terms of catheterization time, length of hospital stay, request for analgesics, risk of bleeding, and incidence of untoward events while offering equivalent outcomes in terms of rapid relief of symptoms and improved urodynamic parameters [
10]. ThuVEP offers a 27.5% cost savings over TURP when in-hospital and cost and events are analyzed. On the basis of the current capital costs, and the fact that the fiber could be reused up to 10 times on bladder stones, 100 procedures annually for 2 to 3 years would achieve complete machine payback including fiber and service costs. Additional cost-effectiveness can be achieved by using the 1-day discharge policy. Further investigation in larger populations as well as with different hospitalization protocols and return to work times is deemed necessary to reinforce the conclusions of the present study related to cost savings.
There are significant differences between different national health policies and health systems. In Italy, for example, the day surgery intervention led to a reduction of 25% of the reimbursement provision compared with ordinary wards. Therefore, this strategy, if implemented, would also lead to reduced costs for national health systems.
The limitations of this work are related to the number of patients undergoing the procedure, the lack of a more prolonged follow-up in order to define long-term complications, and the initial bias in selecting patients with reduced comorbidity and small prostate size.
CONCLUSIONS
ThuVEP can be safely conducted as a 1-day surgery procedure. ThuVEP shows good standardized outcomes considering improvement in flow parameters and length of bladder catheterization. Early catheter removal is not associated with a significant increase in morbidity. This strategy results in cost savings. Our results suggest that the surgical strategy in the management of BOO due to prostatic enlargement could be changed with respect to the standard TURP.
Figures and Tables
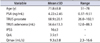
Table 1
Baseline preoperative characteristics of all patients (n=53)
|
Variable |
Mean±SD |
Range |
|
Age (y) |
71.8±8.8 |
51-78 |
|
PSA (ng/mL) |
4.22±2.45 |
0.37-9.51 |
|
TRUS prostate |
68.9±20.1 |
26.0-102.1 |
|
TRUS adenoma (mL) |
56.6±13.3 |
12.0-88.3 |
|
IPSS |
16±3 |
- |
|
QoL |
3.5±1 |
- |
|
Qmax (mL/s) |
9.3±3.8 |
2.3-16.6 |
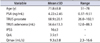
Table 2
Operative data and parameters of surgical efficacy related to the postoperative periods

|
Variable |
Value |
|
Operative time (min) |
71±32 (35-105) |
|
Resected weight (g) |
27.5±10 (15-45) |
|
Preoperative hemoglobin (g/dL) |
14.1 (13.2-15.3) |
|
Postoperative hemoglobin (g/dL) |
13 (12.5-15.0) |
|
Hemoglobin decrease (g/dL) |
1.1 (1.6-0.3) |
|
Transfusion rate (%) |
0 |
|
Mean catheterization time (hr) |
14.8 |
|
Mean hospital stay (day) |
1 |
|
Preoperative IPSS |
16±3 (14-20) |
|
Postoperative IPSS 7th day |
10.2±2 (12-7) |
|
Postoperative IPSS 30th day |
6.5±2 (4-8) |
 Scan this QR code to see the accompanying video, or visit www.kjurology.org or www.youtube.com/KJUrology.
Scan this QR code to see the accompanying video, or visit www.kjurology.org or www.youtube.com/KJUrology. Scan this QR code to see the accompanying video, or visit www.kjurology.org or www.youtube.com/KJUrology.
Scan this QR code to see the accompanying video, or visit www.kjurology.org or www.youtube.com/KJUrology.