Abstract
Purpose
We conducted a prospective single-center study to evaluate the possibility of discontinuation of dutasteride after combination therapy with an alpha blocker for benign prostatic hyperplasia (BPH).
Materials and Methods
We prospectively treated BPH patients with an alpha blocker and dutasteride (0.5 mg/d). Patients who had been treated with alpha blockers against BPH for more than 2 months were eligible, and 20 patients were included in the study. After 6 months of combination therapy, dutasteride was discontinued. Patients were followed for 12 months after cessation. Prostate volume, intraprostatic architecture determined by transrectal ultrasound, peak urinary flow rate, postvoid residual urine volume, and the serum prostate-specific antigen level were evaluated every 6 months, and the International Prostate Symptom Score and overactive bladder symptom score (OABSS) every 3 months. Patients were allowed to restart dutasteride during the follow-up period according to their desire.
Results
Twelve patients (12/20, 60%) restarted the combination therapy from 6 to 12 months into the follow-up period. For patients who restarted dutasteride, the prostate volume and OABSS had increased and worsened after discontinuation, respectively. A visible transition zone with a clear border on transrectal ultrasound at baseline and regrowth of the prostate after discontinuation of dutasteride were risk factors for restarting the therapy (Mann-Whitney U test: p=0.008, p=0.017).
Conclusions
Prostatic enlargement after discontinuation of dutasteride differs among patients. Rapid regrowth of the prostate leads to deterioration of storage symptoms and a tendency to restart dutasteride. Baseline intraprostatic architecture may be a predictive factor for whether the patient is a good candidate for discontinuation.
Dutasteride is a useful drug against benign prostatic hyperplasia (BPH) [1]. Combination therapy using dutasteride with an alpha blocker makes it possible to manage BPH patients for a long duration [2]. Combination of the two drugs, which have different mechanisms of action against BPH, may relieve lower urinary tract symptoms (LUTS) better than monotherapy with either alone [3]. The characteristic effect of dutasteride against BPH is shrinkage of the prostate. Because large prostate volume may lead to severe symptomatic progression or surgical intervention [4], medical reduction of the prostate volume by dutasteride may change the clinical course of BPH patients [1]. The results of the the symptom management after reducing therapy (SMART-1) study suggest that after reduction, monotherapy using an alpha blocker may be feasible [5]. On the other hand, withdrawal of dutasteride is not fully understood. Some patients may not be good candidates for withdrawal even though it will reduce the medical cost. Thus, we performed a single-center prospective study of dutasteride withdrawal after combination therapy with an alpha blocker against BPH.
We performed a prospective study of BPH patients who visited our hospital from 2012 to 2013. Patients who had been given alpha blockers for more than 2 months were eligible for the study. All patients underwent evaluation of the serum prostate-specific antigen (PSA) level, prostate volume, intraprostatic architecture by transrectal ultrasound [6], peak urinary flow rate (Qmax), postvoid residual urine volume (PVR), the International Prostate Symptom Score (IPSS), and the overactive bladder symptom score (OABSS) [7] at baseline. Intraprostatic architecture was divided into 3 groups. Group 1 was defined as BPH with an undetectable transitional zone, group 2 as a detectable transitional zone with an unclear border, and group 3 as a transitional zone with a clear border. The IPSS and OABSS were evaluated every 3 months and the serum PSA level, prostate volume, Qmax, and PVR were evaluated every 6 months. PVR was evaluated by transabdominal ultrasound. Active discontinuation of dutasteride was planned after 6 months of combination therapy with an alpha-1 blocker. Alpha-1 blocker monotherapy was planned to continue for 12 months. However, patients were allowed to restart dutasteride during the follow-up period according to their clinical desire. Twenty-three patients were included in the study. Examination for adverse events such as urinary retention and symptomatic urinary tract infection was conducted at every visit to our outpatient clinic.
Statistical analysis was performed by using the Mann-Whitney U test for intergroup comparisons. The Wilcoxon signed-rank test was performed to evaluate differences in parameters among treatment periods. All values were considered to be statistically significant at p<0.05. Statistical analyses were performed by using SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA). Informed consent was obtained from patients and the study was approved by the Institutional Review Board of NTT East Corporation Sapporo Hospital (No. 13-106).
Twenty-three patients were included in the study but only 20 completed the evaluation. Three patients dropped out owing to withdrawal of consent. Eighteen and two patients were administrated silodosin and naftopidil, respectively. The alpha blocker or dose was not changed for any patient during the study. Mean prostate volume was 36.82 mL at baseline and the mean reduction rate was 22.1% in the 20 patients after 6 months of combination therapy.
Finally, 12 patients (12/20, 60%) restarted combination therapy in the follow-up period. No patient restarted dutasteride within 6 months after its discontinuation. Although only 2 patients restarted at 6 months after discontinuation, another 10 patients hoped to restart between 9 and 12 months.
The prostate volume, IPSS, and OABSS significantly improved after 6 months of combination therapy. Only prostate volume worsened at 6 months after cessation of dutasteride (Fig. 1A). In the 12 patients who restarted dutasteride, the prostate volume and OABSS had deteriorated at the time of restarting dutasteride compared to after 6 months of combination therapy (Fig. 1B). During the follow-up period, no significant change was observed in Qmax or PVR (data not shown). Comparison between patients who restarted combination therapy (n=12) and those who were able to continue monotherapy (n=8) did not reveal any significant differences in baseline parameters (Table 1) other than the intraprostatic architecture. However, for the regrowth rate of the prostate from after 6 months of combination therapy to 6 months after cessation of dutasteride, a significant difference existed between the groups (13.5% vs. 3.0%, Mann-Whitney U test, p=0.017) (Fig. 2). Although IPSS and prostate volume improved in the monotherapy group at 6 months after combination therapy, Qmax and OABSS did not differ statistically during the study period (data not shown).
Combination therapy using an alpha blocker and dutasteride will improve LUTS in BPH patients, especially in patients with a large prostate [2]. It is well known that combination therapy is more effective than monotherapy against BPH. Jeong et al. [8] reported that regrowth of the prostate occurs after discontinuation of 5-alpha reductase inhibitors and results in worsening of the IPSS. They concluded that lifelong use of a 5-alpha reductase inhibitor may be needed. It is true that BPH is a progressive disease. However, Lee et al. [9] reported the effectiveness of discontinuation of tamsulosin after combination therapy with dutasteride. They concluded that discontinuation of tamsulosin did not result in worsening of the IPSS in BPH patients with moderate IPSS. Barkin et al. [5] also reported in their prospective randomized (SMART-1) study that BPH patients with moderate IPSS might be able to discontinue alpha blocker use after combination therapy with dutasteride. However, patients with a severe IPSS (>20) experienced deterioration of their symptoms. Those authors concluded that such patients might benefit from continuous combination therapy.
Fukuta et al. [6] reported the natural history of BPH and categorized it into 3 groups according to the internal architecture of the prostate on transrectal ultrasound. They concluded that future prostatic enlargement differed among the architecture types. In group 3, the prostate was more likely to enlarge rapidly than in the other two groups. The same regrowth phenomenon may occur even after shrinkage by dutasteride depending on the intraprostatic architecture. In other words, in some patients, the effect of dutasteride will be maintained even after discontinuation of the medication.
Our study showed that patients with rapid regrowth after discontinuation tended to hope to restart dutasteride (Fig. 2). Thus, regrowth of the prostate after discontinuation was a risk factor for restarting dutasteride. However, we have to seek predictive factors for future rapid regrowth to select good candidates for withdrawal treatment at baseline. In this study, nine of the ten patients in group 3 restarted dutasteride. Thus, being in group 3 was a risk factor for restarting compared with the other groups at baseline (p=0.008, Mann-Whitney U test) (Table 1). Considering that, the intraprostatic architecture may be useful to distinguish patients able to withdraw from dutasteride from others at the start of combination therapy.
Although previous studies [5,8,9] evaluated patients' symptoms after discontinuation of dutasteride or the alpha-1 blocker according to the IPSS, storage symptoms were not reported in detail. Our study prospectively evaluated storage symptoms by using the OABSS. BPH patients with OAB often suffer from bother and it is hard to treat symptoms like nocturia [10]. Evaluation for changes in storage symptoms during discontinuation of combination therapy is essential for maintaining the patient's quality of life. In our study, worsening of the OABSS after discontinuation was seen and eventually led to restarting the 5-alpha reductase inhibitor. Thus, after discontinuation, rapid prostatic regrowth occurred in some patients and storage symptoms worsened, which finally resulted in restarting combination therapy. Therefore, rapid regrowth may be a surrogate phenomenon to determine if discontinuation is sustainable. In addition, detailed evaluation of the patient's intraprostatic architecture at baseline and the deterioration of storage symptoms during follow-up may help clinicians decide if continuation of withdrawal is feasible. On the other hand, no significant change was observed in Qmax or PVR. Therefore, Qmax and PVR might not be appropriate surrogate parameters. In this study, no patient with acute urinary retention was observed even after discontinuation.
Patients with group 3 intraprostatic architecture at baseline may experience rapid regrowth, which will result in restarting combination therapy. Follow-up of patients treated with the withdrawal strategy should be conducted by using transrectal ultrasound to evaluate prostate regrowth, and a questionnaire should be used to determine storage symptoms.
There were some limitations to our study. Multivariate analysis was not capable because of the small sample size. In addition, interpretation of the type of intraprostatic architecture evaluated by transrectal ultrasound may differ by operator, which could lead to bias to some extent. In addition, prostate volume was not strictly defined in the inclusion criteria of the study. Although intraprostatic architecture may be a factor for predicting future regrowth after the withdrawal of treatment, the continued monotherapy group had a low proportion of group 3 patients. To verify our conclusions, a study with a large number of patients is essential in the future.
Figures and Tables
 | Fig. 1(A) Changes of clinical parameters (mean values) in all 20 patients from baseline to 6 months after discontinuation of dutasteride. (B) Changes of clinical parameters (mean values) in 12 patients from baseline to the point of restarting dutasteride. IPSS, International Prostate Symptom Score; OABSS, overactive bladder symptom score; Qmax, peak urinary flow rate; NS, not significant. **p<0.01.***p<0.001. Wilcoxon signed-rank test. |
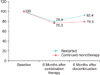 | Fig. 2Changes of prostate volume (mean values) for groups 1 and 2 from baseline to 6 months after discontinuation. |
Table 1
Background and comparison of clinical factors between the groups at baseline

References
1. Wu XJ, Zhi Y, Zheng J, He P, Zhou XZ, Li WB, et al. Dutasteride on benign prostatic hyperplasia: a meta-analysis on randomized clinical trials in 6460 patients. Urology. 2014; 83:539–543.
2. Roehrborn CG, Barkin J, Siami P, Tubaro A, Wilson TH, Morrill BB, et al. Clinical outcomes after combined therapy with dutasteride plus tamsulosin or either monotherapy in men with benign prostatic hyperplasia (BPH) by baseline characteristics: 4-year results from the randomized, double-blind Combination of Avodart and Tamsulosin (CombAT) trial. BJU Int. 2011; 107:946–954.
3. Roehrborn CG, Barkin J, Tubaro A, Emberton M, Wilson TH, Brotherton BJ, et al. Influence of baseline variables on changes in International Prostate Symptom Score after combined therapy with dutasteride plus tamsulosin or either monotherapy in patients with benign prostatic hyperplasia and lower urinary tract symptoms: 4-year results of the CombAT study. BJU Int. 2014; 113:623–635.
4. Masumori N, Tsukamoto T, Rhodes T, Girman CJ. Natural history of lower urinary tract symptoms in men: result of a longitudinal community-based study in Japan. Urology. 2003; 61:956–960.
5. Barkin J, Guimaraes M, Jacobi G, Pushkar D, Taylor S, van Vierssen Trip OB. Alpha-blocker therapy can be withdrawn in the majority of men following initial combination therapy with the dual 5alpha-reductase inhibitor dutasteride. Eur Urol. 2003; 44:461–466.
6. Fukuta F, Masumori N, Mori M, Tsukamoto T. Internal prostatic architecture on transrectal ultrasonography predicts future prostatic growth: natural history of prostatic hyperplasia in a 15-year longitudinal community-based study. Prostate. 2011; 71:597–603.
7. Homma Y, Yoshida M, Seki N, Yokoyama O, Kakizaki H, Gotoh M, et al. Symptom assessment tool for overactive bladder syndrome: overactive bladder symptom score. Urology. 2006; 68:318–323.
8. Jeong YB, Kwon KS, Kim SD, Kim HJ. Effect of discontinuation of 5alpha-reductase inhibitors on prostate volume and symptoms in men with BPH: a prospective study. Urology. 2009; 73:802–806.
9. Lee JY, Kang DH, Park SY, Lee SW, Kim YT, Choi HY. Effect of discontinuation of tamusulosin in Korean men with benign prostatic hyperplasia taking tamusulosin and dutasteride: An open-label prospective, randomized pilot study. LUTS. 2012; 4:35–40.
10. Yoshimura K, Ohara H, Ichioka K, Terada N, Matsui Y, Terai A, et al. Nocturia and benign prostatic hyperplasia. Urology. 2003; 61:786–790.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download