Abstract
Purpose
Xp11.2 translocation renal cell carcinoma (RCC) is characterized by various translocations of the TFE3 transcription factor gene. These rare cancers occur predominantly in children and young adults. Here, we review the clinicopathological features of Xp11.2 translocation RCC.
Materials and Methods
We identified 21 patients with Xp11.2 translocation RCC. We retrospectively analyzed patient characteristics, clinical manifestations, and specific pathological features to assess definitive diagnosis, surgical and systemic treatments, and clinical outcomes.
Results
The mean age at diagnosis was 43.4±20.0 years (range, 8-80 years; 8 males and 13 females). Eleven patients were incidentally diagnosed, nine patients presented with local symptoms, and one patient presented with systemic symptoms. The mean tumor size was 6.2±3.8 cm (range, 1.9-14 cm). At the time of diagnosis, 11, 1, and 5 patients showed stage I, II, and III, respectively. Four patients showed distant metastasis. At analysis, 15 patients were disease-free after a median follow-up period of 30.0 months. Four patients received target therapy but not effectively.
Conclusions
Xp11 translocation RCC tends to develop in young patients with lymph node metastasis. Targeted therapy did not effectively treat our patients. Surgery is the only effective therapy for Xp11 translocation RCC, and further studies are needed to assess systemic therapy and long-term prognosis.
Renal cell carcinomas (RCCs) are heterogeneous tumors that account for approximately 90% of all adult renal malignancies. The most common subtypes are clear cell (60%-75%), papillary (10%-15%), chromophobe (5%), and collecting duct carcinoma, and each is associated with unique features at the molecular and genetic levels. Recent progress in understanding the molecular alterations that define kidney tumorigenesis has led to the development of these tumor subclassifications [1,2]. Tomlinson et al. [3] published the first pediatric case report on Xp11.2 translocation RCC, which developed in a 17-month-old child. Xp11 translocation RCC was recently recognized as a distinct subset of renal carcinomas, and RCC is associated with a number of genetic rearrangements of the TFE3 gene on chromosome Xp11.2. The 2004 World Health Organization classifications list Xp11.2 translocation RCC as a distinct entity of renal tumor [4].
Xp11.2 translocation RCC occurs predominantly in children and young adults; young adults account for 20% to 75% of pediatric RCC cases and about 1.5% of RCC adult cases [5,6]. However, actual incidence largely remains underestimated. RCCs are defined by several TFE3 translocations on chromosome Xp11.2, resulting in gene fusion between TFE3 and at least 6 possible partners. The most commonly observed translocations are t(X;17)(p11.2;q25), t(X;1)(p11.2;p34), and t(X;1)(p11.2;q21), which lead to gene fusions between TFE3 and ASPL, PSF, and PRCC, respectively [7,8,9].
Xp11.2 translocation RCC typically demonstrates nested or papillary architecture and is composed of cells with voluminous, clear, or eosinophilic cytoplasm that histologically mimic clear cell and papillary renal carcinoma [10,11]. Translocations involving TFE3 induce protein overexpression and can be specifically identified on immunohistochemistry (IHC) by using an antibody for the C-terminal portion of TFE3, which has been reported in all fusion products. Nuclear labeling for TFE3 protein by IHC is specific to Xp11.2 translocation RCC, but cannot detect RCC in normal tissue or other tumor types. IHC analysis for nuclear TFE3 staining can confirm the diagnosis of Xp11 translocation RCC in archived tissues. A recently developed antibody for TFE3 protein is considered a highly sensitive (97.5%) and specific (99.6%) marker of these tumors [12].
Previously published reports on Xp11.2 translocation RCC have documented the pathological and clinical features of this rare form of renal carcinoma [9]. However, there are relatively few reported case studies in Korea [13]. Here, we report the clinicopathological features of Xp11.2 translocation RCC and oncologic outcomes in our institution.
The study protocol was approved by the Institutional Review Board of the Asan Medical Center (2014-0498). The medical records of the Asan Medical Center, a tertiary referral center, were screened for patients who had been pathologically diagnosed with Xp11.2 translocation RCC. In total, 2573 patients underwent radical or partial nephrectomy for RCC treatment and 293 patients underwent renal biopsy for RCC diagnosis between December 2006 and May 2013 at Asan Medical Center. An additional 21 cases of Xp11.2 translocation RCC diagnosed between December 2006 and May 2013 were retrieved from the surgical pathological archives. In this retrospective chart review, clinicopathologic data were analyzed, including patient characteristics, clinical manifestations, surgical techniques, pathologic findings, radiology, and clinical outcomes. All patients underwent staging evaluation at the time of diagnosis, including clinical examination, blood investigations, chest x-ray, computed tomography (CT) of the abdomen and pelvis, and bone scan. According to the signs and symptoms, some patients underwent chest CT and brain imaging.
All pathological examinations were performed by a pathologist according to the 2010 TNM classification system. All patients received follow-up with laboratory and radiological examinations according to the final TNM stage and tumor grade. IHC analysis for nuclear TFE3 staining confirmed the diagnosis of Xp11 translocation RCC. TFE3 stain was performed in young patients or in samples with histological features suggestive of translocation carcinoma, which have a papillary architecture and clear to eosinophilic cytoplasm. Twenty-one cases of Xp11.2 translocation RCC were analyzed by IHC staining to detect TFE3 in each tumor and tissue microarray block (catalog No. sc-5958; Santa Cruz Biotechnology, Santa Cruz, CA, USA).
Angiogenesis marker IHC analysis of the tumour tissue samples was performed by using the Ventana XT auto immunostainer (Roche, San Francisco, CA, USA) with the Optiview Dab Detection Kit (Roche) according to the manufacturer's instructions. IHC results were independently evaluated by two specialized pathologists blind to the clinical data. A semiquantitative scoring system was used based on staining intensity (0, negative; 1, weak; 2, intermediate; 3, strong), which corresponds to the percentage of positive-stained cells (0, <5% positive; 1, 5%-33.3% positive; 2, 33.3%-66.7% positive; 3, ≥66.7% positive). A score ≥1 indicates positive immunohistochemical identification of a marker. The Fuhrman nuclear grading system, which uses a four-point multiparametric scale based on nuclear features, size, shape, color, and nucleolar prominence, was also used [14]. Tumor sizes were evaluated by measuring the largest diameter of the surgically removed mass.
The clinical characteristics of the patients are listed in Table 1. The mean age at presentation was 43.4±20.0 years (range, 8-80 years), including 8 males and 13 females. Eleven of 21 patients were incidentally diagnosed. Five patients (33.3%) presented with flank pain, three patients (14.3%) with gross hematuria, one patient with a palpable mass, and one patient with cough (pleural metastasis). The tumor was located on the right side in 14 patients (66.7%) and on the left side in 7 patients (33.3%). No bilateral disease was observed. One patient had multifocal disease. The greatest dimension of the tumor ranged from 1.9 to 12 cm (mean tumor size, 6.2±3.8 cm). Ten patients underwent radical nephrectomy for the primary tumor (eight open radical nephrectomy, one laparoscopic radical nephrectomy, and one hand-assisted laparoscopic radical nephrectomy). Eight patients underwent partial nephrectomy (three robotic partial nephrectomy and five open partial nephrectomy). Six patients underwent lymph node dissection. Four patients were diagnosed with lymph node metastasis.
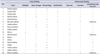
Three patients underwent preoperative renal biopsy, but all three cases were misdiagnosed as clear cell RCC owing to the brown or yellow macroscopic appearance of the tumor. Under our care, three patients were misdiagnosed with clear cell RCC by preoperative renal biopsy (two patients were treated at another hospital). These biopsies often confirmed cystic change (31%), hemorrhage (43%), necrosis (25%), change to sarcomatoid (12.5%), calcification (12.5%), and lymphovascular invasion (12.5%) (Table 2). Microscopically, the RCC tumor cells demonstrate an abundant and clear to eosinophilic cytoplasm and distinct cell borders that form the papillary architecture. The Fuhrman grade was 2 in 4 patients, 3 in 11 patients, and 4 in 3 patients.
All tumors demonstrated IHC staining for TFE3. IHC analysis of the surgically obtained tissue samples was performed by using antibodies for tumor angiogenesis markers. Sixteen patients demonstrated strongly positive vascular endothelial growth factor (VEGF) staining intensity, and one patient demonstrated weakly positive staining intensity. By IHC analysis, one patient demonstrated strongly positive and one patient demonstrated weakly positive VEGF receptor 2 (VEGFR2) staining. Two patients demonstrated strongly positive and eight patients demonstrated weakly positive platelet-derived growth factor-beta (PDGF-β) IHC staining. In addition, one patient demonstrated strong and one weak PDGF receptor-beta (PDGFR-β) staining.
The pathological stage was T1a in five patients, T1b in seven patients, T2b in one patient, and T3a in five patients. On pathologic examination for diagnosis, 11, 1, and 5 patients were diagnosed as stages I, II, or III RCC (including 4 patients with lymph node metastasis), respectively. Only four patients were diagnosed with distant metastasis (three pulmonary metastasis and one bone metastasis). At the time of this study, 15 patients had maintained a diseasefree status for a median duration of 30.0 months (range, 18-96.4 months). One patient was diagnosed with regional lymph node metastasis at 5 months postoperatively, but refused further treatment. Another patient developed bone metastasis at 4 months postoperatively. A female patient with bone metastasis received targeted sunitinib therapy for 4 months and everolimus for 2 months but died 14 months after treatment.
Another patient with distant metastasis (pulmonary metastasis) underwent preoperative renal biopsy but was misdiagnosed with clear cell RCC. He received targeted pazopanib therapy for 9 months before surgery (radical nephrectomy and lung bilobectomy). His disease progressed despite prior targeted therapy. After surgery, the patient received targeted temsirolimus therapy for 7 weeks but refused further treatment. The patient died 11.4 months after the operation.
Three patients diagnosed with Xp11 translocation RCC on kidney biopsy had a distant metastasis at the time of diagnosis. Two of these patients received targeted therapy. One patient with bone metastasis received targeted sunitinib therapy and radiation therapy; after that, disease status remained stable for 18 months. However, the disease progressed despite prior targeted therapy, and she received axitinib. The other patient with lung metastasis received temsirolimus for 5 weeks but died of cancer progression at 2 months.
Xp11.2 translocation RCC, a recently classified distinct subtype of RCC, is a rare tumor that usually affects children and adolescents; only a few adult cases have been reported to date [15,16]. In our experience, Xp11.2 translocation RCC accounts for 0.7% of all RCCs. In our institution, however, TFE3 stain is performed in young patients and in patients with histological features suggestive of translocation carcinoma. Xp11 translocation RCCs can also present with unusual morphology mimicking other types of RCCs, including multilocular cystic RCC-like features, pleomorphic giant cells, tubular growth reminiscent of collecting duct carcinoma, and well-developed fascicles of spindled neoplastic cells with bland nuclei and focal myxoid stroma [17]. Thus, the accuracy of diagnosis is variable. In the past, the incidence of Xp11.2 translocation RCC may have been underestimated.
The mean age of our current study population was 43.4 years, and the male:female ratio was 8:13. The mean tumor size in this series was 6.2 cm. Our cases demonstrated smaller tumor sizes than those reported in Patard's and Philippe's previous series (6.0-6.8 cm) and in the clinical experiences of Taipei Veterans General Hospital (9.2 cm). Also, our patients were older on average than in previous studies [18,19]. The pT stage also differed in our series compared with previous studies: Xp11.2 translocation RCC diagnosis was more advanced (50% pT3/T4) in our series. Only five of our patients (33.3%) were diagnosed with pT3 stage, and pT4 (0%) has never been diagnosed in our hospital [18,19]. Lymph node and distal metastasis was diagnosed in 28.5% of our patients compared with 37.5% to 50% in other studies [18,19].
Morphologically, Xp11.2 translocation RCC is composed of cells with abundant clear or pale cytoplasm with nested or papillary architecture on routine hematoxylin and eosin-stained sections. This may overlap with clear cell RCC, such that three of our cases were misdiagnosed with clear cell RCC on preoperative renal biopsy. The incidence of Xp11.2 translocation RCC may be underestimated when diagnoses are made by using renal biopsies.
The most distinct immunochemical feature of Xp11.2 translocation RCCs is IHC TFE3 staining, which can provide a definitive diagnosis. A recently developed antibody for the TFE3 protein is a highly sensitive (97.5%) and specific (99.6%) marker of these tumors. In our current series, all 21 patients demonstrated IHC TFE3 staining.
In a recent study, TFE3 break-apart fluorescence in situ hybridization (FISH) was found to be useful for diagnosing Xp11.2 translocation RCC. In other studies, some patients were negative for immunohistochemical TFE3 staining but could be diagnosed on FISH, such that the incidence of Xp11.2 translocation RCC will change if FISH is used to diagnose this cancer [20,21].
Previous studies have not reported tumor angiogenesis markers in Xp11.2 translocation RCC. We tested for tumor angiogenesis markers. VEGF was strongly positive in 16 patients, whereas VEGFR2, PDGF-β, and PDGFR-β stained more weakly than VEGF (Table 3). At the time of analysis, 15 of our patients were disease-free for a median duration of 30.0 months. Four patients received targeted therapy, but only one patient with bone metastasis received targeted sunitinib therapy and has been stable for 1 year. As a result, we treated metastatic Xp11.2 translocation RCC using targeted therapy, but almost all patients progressed and no targeted agent was effective. In a recent study, VEGFR-2 expression was suggested to be a useful biomarker for predicting the response to sunitinib in clear cell RCC [22]. Identifying angiogenesis markers can be an important method for predicting response to targeted therapy in Xp11.2 translocation RCC. Further studies are needed to assess the relationship between targeted agents and angiogenesis markers.
The limitations in this study were the small number of patients analyzed, the retrospective design, the short duration, and the single-center setting.
In conclusion, we report here the clinical presentation, pathological features, and clinical outcomes of 21 recently diagnosed patients with Xp11.2 translocation RCC who were treated at our hospital. Xp11 translocation RCC tends to develop in young patients and shows lymph node metastasis. Targeted therapy is not effective in our experience; surgical treatment is the only effective therapy for Xp11 translocation RCC. Further studies are needed to assess systemic therapies and long-term prognosis with regard to this cancer.
Figures and Tables
Table 1
Clinical characteristics of the study patients
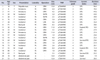
Table 2
Pathological characteristics of the study patients
ACKNOWLEDGMENTS
This study was supported by a grant of the Korean Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (HI06C0868 and HI10C2014).
References
1. Linehan WM, Zbar B. Focus on kidney cancer. Cancer Cell. 2004; 6:223–228.
2. Linehan WM, Bratslavsky G, Pinto PA, Schmidt LS, Neckers L, Bottaro DP, et al. Molecular diagnosis and therapy of kidney cancer. Annu Rev Med. 2010; 61:329–343.
3. Tomlinson GE, Nisen PD, Timmons CF, Schneider NR. Cytogenetics of a renal cell carcinoma in a 17-month-old child. Evidence for Xp11.2 as a recurring breakpoint. Cancer Genet Cytogenet. 1991; 57:11–17.
4. Lopez-Beltran A, Scarpelli M, Montironi R, Kirkali Z. 2004 WHO classification of the renal tumors of the adults. Eur Urol. 2006; 49:798–805.
5. Bruder E, Passera O, Harms D, Leuschner I, Ladanyi M, Argani P, et al. Morphologic and molecular characterization of renal cell carcinoma in children and young adults. Am J Surg Pathol. 2004; 28:1117–1132.
6. Ramphal R, Pappo A, Zielenska M, Grant R, Ngan BY. Pediatric renal cell carcinoma: clinical, pathologic, and molecular abnormalities associated with the members of the mit transcription factor family. Am J Clin Pathol. 2006; 126:349–364.
7. Argani P, Antonescu CR, Illei PB, Lui MY, Timmons CF, Newbury R, et al. Primary renal neoplasms with the ASPL-TFE3 gene fusion of alveolar soft part sarcoma: a distinctive tumor entity previously included among renal cell carcinomas of children and adolescents. Am J Pathol. 2001; 159:179–192.
8. Argani P, Lui MY, Couturier J, Bouvier R, Fournet JC, Ladanyi M. A novel CLTC-TFE3 gene fusion in pediatric renal adenocarcinoma with t(X;17)(p11.2;q23). Oncogene. 2003; 22:5374–5378.
9. Argani P, Olgac S, Tickoo SK, Goldfischer M, Moch H, Chan DY, et al. Xp11 translocation renal cell carcinoma in adults: expanded clinical, pathologic, and genetic spectrum. Am J Surg Pathol. 2007; 31:1149–1160.
10. Zhong M, De Angelo P, Osborne L, Paniz-Mondolfi AE, Geller M, Yang Y, et al. Translocation renal cell carcinomas in adults: a single-institution experience. Am J Surg Pathol. 2012; 36:654–662.
11. Zou H, Kang X, Pang LJ, Hu W, Zhao J, Qi Y, et al. Xp11 translocation renal cell carcinoma in adults: a clinicopathological and comparative genomic hybridization study. Int J Clin Exp Pathol. 2013; 7:236–245.
12. Argani P, Lal P, Hutchinson B, Lui MY, Reuter VE, Ladanyi M. Aberrant nuclear immunoreactivity for TFE3 in neoplasms with TFE3 gene fusions: a sensitive and specific immunohistochemical assay. Am J Surg Pathol. 2003; 27:750–761.
13. Kim SH, Choi Y, Jeong HY, Lee K, Chae JY, Moon KC. Usefulness of a break-apart FISH assay in the diagnosis of Xp11.2 translocation renal cell carcinoma. Virchows Arch. 2011; 459:299–306.
14. Fuhrman SA, Lasky LC, Limas C. Prognostic significance of morphologic parameters in renal cell carcinoma. Am J Surg Pathol. 1982; 6:655–663.
15. Altinok G, Kattar MM, Mohamed A, Poulik J, Grignon D, Rabah R. Pediatric renal carcinoma associated with Xp11.2 translocations/TFE3 gene fusions and clinicopathologic associations. Pediatr Dev Pathol. 2005; 8:168–180.
16. Koie T, Yoneyama T, Hashimoto Y, Kamimura N, Kusumi T, Kijima H, et al. An aggressive course of Xp11 translocation renal cell carcinoma in a 28-year-old man. Int J Urol. 2009; 16:333–335.
17. Srigley JR, Delahunt B, Eble JN, Egevad L, Epstein JI, Grignon D, et al. The International Society of Urological Pathology (ISUP) Vancouver Classification of Renal Neoplasia. Am J Surg Pathol. 2013; 37:1469–1489.
18. Argani P, Lae M, Hutchinson B, Reuter VE, Collins MH, Perentesis J, et al. Renal carcinomas with the t(6;11)(p21;q12): clinicopathologic features and demonstration of the specific alpha-TFEB gene fusion by immunohistochemistry, RT-PCR, and DNA PCR. Am J Surg Pathol. 2005; 29:230–240.
19. Patard JJ, Leray E, Rioux-Leclercq N, Cindolo L, Ficarra V, Zisman A, et al. Prognostic value of histologic subtypes in renal cell carcinoma: a multicenter experience. J Clin Oncol. 2005; 23:2763–2771.
20. Green WM, Yonescu R, Morsberger L, Morris K, Netto GJ, Epstein JI, et al. Utilization of a TFE3 break-apart FISH assay in a renal tumor consultation service. Am J Surg Pathol. 2013; 37:1150–1163.
21. Rao Q, Williamson SR, Zhang S, Eble JN, Grignon DJ, Wang M, et al. TFE3 break-apart FISH has a higher sensitivity for Xp11.2 translocation-associated renal cell carcinoma compared with TFE3 or cathepsin K immunohistochemical staining alone: expanding the morphologic spectrum. Am J Surg Pathol. 2013; 37:804–815.
22. You D, Song SH, Cho YM, Lee JL, Jeong IG, Song C, et al. Predictive role of tissue-based molecular markers in patients treated with sunitinib for metastatic renal cell carcinoma. World J Urol. 2015; 33:111–118.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download