Abstract
The da Vinci S surgical system (Intuitive Surgical) was approved as a medical device in 2009 by the Japanese Ministry of Health, Labour and Welfare. Robotic surgery has since been used in gastrointestinal, thoracic, gynecological, and urological surgeries. In April 2012, robotic-assisted laparoscopic radical prostatectomy (RALP) was first approved for insurance coverage. Since then, RALP has been increasingly used, with more than 3,000 RALP procedures performed by March 2013. By July 2014, 183 institutions in Japan had installed the da Vinci surgical system. Other types of robotic surgeries are not widespread because they are not covered by public health insurance. Clinical trials using robotic partial nephrectomy and robotic gastrectomy for renal and gastric cancers, respectively, have recently begun as advanced medical treatments to evaluate health insurance coverage. These procedures must be evaluated for efficacy and safety before being covered by public health insurance. Other types of robotic surgery are being evaluated in clinical studies. There are several challenges in robotic surgery, including accreditation, training, efficacy, and cost. The largest issue is the cost-benefit balance. In this review, the current situation and a prospective view of robotic surgery in Japan are discussed.
The da Vinci S surgical system (Intuitive Surgical, Sunnyvale, CA, USA) was approved by the Japanese Ministry of Health, Labour and Welfare (MHLW) in November 2009. Subsequently, robotic surgery has been applied in general, thoracic, gynecological, and urological surgery programs at several Japanese academic institutions. In April 2012, robotic-assisted laparoscopic radical prostatectomy (RALP) was approved as an insured medical treatment, and by March 2013, more than 3,000 RALP procedures had been performed. By July 2014, 183 institutions had installed the da Vinci surgical system.
No robotic procedures other than RALP are covered by public health insurance, and mixed billing is prohibited. This has limited the use of other robotic surgeries.
The possible superiority of a robotic approach over open or laparoscopic approaches is a current subject of controversy in a wide range of surgical procedures. There are several approaches in radical prostatectomy procedures, including open, minimum incision, conventional laparoscopy, and robotic-assisted laparoscopy. At the 27th Congress of the Japanese Society of Endourology (JSE) in 2013, a symposium was held to discuss several surgical options and potential challenges for radical prostatectomy. Here, I review the current situation and provide a prospective view on robotic urological surgery in Japan.
In Japan, the da Vinci Standard surgical system was first introduced in the Keio University Hospital for clinical studies in March 2000 [1]. Thereafter, it was introduced in the Kyushu University Hospital. The ZEUS robotic surgical system (Computer Motion Inc, Santa Barbara, CA, USA) was also introduced in a few institutions including the Kyushu University Hospital. These robotic systems were used in the field of general digestive surgery, thoracic surgery, and urology as clinical studies and were evaluated by the MHLW. But neither system had been approved for a medical device and the Zeus surgical system was withdrawn from the market.
The da Vinci S, the next-generation surgical system, was introduced for RALP as a clinical study in Tokyo Medical Hospital in 2006 and was approved as a medical device in Japan in November 2009. The fields of indication are as follows: general digestive surgery, thoracic surgery (excluding cardiac surgery), urology, and gynecology. Concerning approval, the MHLW established the following guidelines:
(1) Compliance with "the Guidelines for Endoscopic Surgery (established on August 29, 1992)" established by the Japan Society for Endoscopic Surgery (JSES).
(2) Compliance with "the perspectives on new medical devices" announced by JSES.
(3) Regarding institutions, physicians, and medical teams: constant records of endoscopic surgery in gastroenterological surgery, thoracic surgery, urology, and gynecology (presence of a JSES board-certified surgeon).
(4) The presence of a medical team with knowledge of the performance and use of the device.
(5) Physicians and medical teams conducting surgery must participate in training programs provided by the company and have obtained certification. The validity of the program content must be evaluated and reviewed by JSES.
(6) Infrastructure allowing for procedures (e.g., thoracotomy, laparotomy) to be performed in emergencies.
There are two paths for the approval of individual medical technologies for health insurance coverage. One route involves the submission of a request by a relevant scientific society to the Medical Technology Evaluation Subcommittee. The review results are sent to the Central Social Insurance Medical Council. The second route involves a proposal from a medical institution sent to the Advanced Medical Treatment Expert Meeting. If a medical technology is approved as an advanced medical treatment, an associated medical cost other than the advanced medical treatment is covered by public health insurance. The mixed billing of the advanced medical fee and the health insured fee is exceptionally permitted by MHLW. Data are accumulated as advanced medical treatment data, and the results of the evaluation for health insurance coverage are sent to the Central Social Insurance Medical Council. Reimbursement prices for the devices themselves are not determined for expensive medical devices; instead, they are evaluated on the basis of newly defined technical fees. The cost-effectiveness of medical devices, particularly surgery-assisting robots, is evaluated by the Central Social Insurance Medical Council. If the price of a device remains high without higher efficacy, it may be rejected from health insurance coverage for Japanese citizens. In this case, the comparison target will be laparoscopic surgery. The verification of not only the inferiority but also the superiority of short-term (e.g., suture failure, complication) and long-term (e.g., survival) outcomes immediately after surgery compared to control operations is required. Meanwhile, although reductions in burden and fatigue on surgeons should also be considered as increased efficacy in evaluations, this point is unfortunately not debated much.
For laparoscopic surgery, the JSES and the JSE have established the board certification system for physicians [2]. However, the system is not mandatory for medical care that is covered by health insurance. No board certification system exists for either society for robotic surgery, and thus certification must be obtained from Intuitive Surgical Inc.
The guideline for da Vinci-assisted surgery for urological disease was established in April 2010 by the Japanese Urological Association and the JSE and was revised on November 30, 2012. The recommendations in this guideline include starting robotic surgery ideally with radical prostatectomy, experience with 10 or more patients undergoing robotic surgery, including observation and instructor-supervised surgery, and approval from the institutional ethics committees for each operative procedure besides radical prostatectomy. In addition, it is recommended that a board-certified surgeon skilled in urological laparoscopic techniques participate or provide instruction at the beginning of renal or adrenal gland surgery. However, in radical prostatectomy, there is no reference to the participation of or instruction from a board-certified surgeon skilled in urological laparoscopic technique. Therefore, it is possible for institutions to alternate between open radical prostatectomy and RALP. JSES announced a similar recommendation in July 2011 (http://www.jses.or.jp/member/pdf_regulation/robot_20120815.pdf).
In November 2014, the first proctor training session was held at the 28th Congress of JSE. The roles of proctors are to (1) introduce safe and smooth robotic surgery, and (2) provide feedback to the JSE regarding any problems experienced. This proctor system is scheduled to be implemented starting in 2015 and is likely to be proactively used in institutions introducing robotic-assisted laparoscopic partial nephrectomy (RALPN) and robotic-assisted laparoscopic radical cystectomy (RALRC).
In Japan, surgeries to treat localized prostate cancer include retropubic radical prostatectomy (RRP), perineal radical prostatectomy (PRP), minimum-incision endoscopic radical prostatectomy (MIERP), laparoscopic radical prostatectomy (LRP), and RALP.
RRP has been the standard therapy used to achieve long-term cancer control, as well as preserve urinary and sexual functional. RRP has the advantage of being an extraperitoneal procedure with the use of tactile sensation. Importantly, RRP also provides a good open surgery training opportunity for young surgeons. However, the drawbacks of this procedure include a long skin incision and the risk of blood loss, which have led urological surgeons to opt for less invasive surgery.
Although PRP has the advantages of less blood loss [3] and postoperative pain [4] compared to RRP, this procedure has been used in a limited number of institutions in Japan because pelvic lymph node dissection cannot be performed simultaneously through the same approach.
LRP was first reported by Schuessler in 1997 [5]. After reports of the improved outcome of patients undergoing this surgery by Guillonneau et al. [6,7,8], LRP was introduced in Japanese clinical practice in 1999. After evaluating the efficacy and safety of LRP performed at accredited institutions, this procedure was approved for health insurance coverage by the MHLW in 2006. Surgeons and institutions must be accredited to perform LRP. Thus far, LRP has not been widely accepted in Japan because of the technical difficulties involved in the handling of the pelvis, such as during bladder neck incision, neurovascular bundle preservation, prostatic apex incision, and urethra and bladder neck anastomosis.
MIERP was first performed by Kihara et al. [9] and was approved by the MHLW in 2006 as an advanced medical treatment; this procedure has been covered by public health insurance since 2008. Surgeons and their institutions must be accredited to perform MIERP. The procedure has been widely applied as a minimally invasive surgery [10], and 77 institutions were accredited in 2011. The characteristics of this procedure include a minimal incision of around 5 cm in length, an extraperitoneal approach, and a magnified view using endoscopy. Because the incision length can be adjusted according to the intraoperative condition, surgeons skilled in RRP can safely perform MIERP. Although special retractors are needed, neither carbon dioxide nor a cannula port is required. Therefore, MIERP is economical compared with LRP or RALP. Despite this, MIERP has not been widely adopted because of the technical difficulty in the execution of the procedure through a small incision.
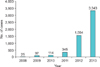
RALP was introduced in 2006 [11]. Tokyo Medical University applied for RALP to be considered an advanced medical treatment and the MHLW approved the treatment in 2008. Without a large prospective comparative study after 3-year usage, the public health insurance program began to cover the cost of RALP in April 2012. Since then, the number of RALP procedures performed has been increasing rapidly (Fig. 1).
The da Vinci surgical system has allowed more free and delicate movement of forceps and scissors than other procedures under a three-dimensional view. On the other hand, there are disadvantages to the procedure; for example, there is no tactile sensation, there is an added risk of steep Trendelenburg position, and the cost is higher.
Initial concerns about RALP in Japan were its safety and efficacy. Surgeons should be aware of the possibility of traction or pressure injury due to the loss of tactile sensation, particularly in early cases. The difference in positive surgical margins between RALP and LRP at the site of surgery was reported by Nagoya City University [12]; excessive counter-traction to the posterior prostate might cause capsular cleavage, leading to posterior positive surgical margins.
Because the Trendelenburg position significantly increases cerebral and intraocular pressure, neurological or vision complications are a concern, particularly in patients with intracranial disease or glaucoma. In patients without pre-existing ocular disease, short-term steep Trendelenburg positioning during the procedures appears to pose little or no increase in the risk of intraocular pressure [13]. A neuro-ocular benefit has been reported from the use of a modified Trendelenburg position [14].
The perioperative outcomes of RALP during its initial year were recently reported by Sugihara et al. [15]. In this report, RALP was compared with other types of radical prostatectomy by using the Japanese Diagnosis Procedure Combination database (April 2012-March 2013), including 7,202 RRP/PRP (55.4%), 2,483 LRP (19.1%), 1,181 MIERP (9.1%), and 2,126 RALP (16.4%) cases. Even in its initial year, RALP was associated with a significantly lower complication rate (0.8% overall) despite the long anesthesia time and high cost. The anesthesia time during RALP was 42.6%, 6.9%, and 23.9% more than that during RRP/PRP, LRP, and MIERP, respectively. The total cost of RALP was 52.4%, 13.2%, and 22.8% higher than that of RRP/PRP, LRP, and MIERP, respectively. The cost differences are mainly due to the official fee for the surgery itself, which is approximately 4,108 United States dollar (USD), 7,743 USD, 5,978 USD, and 9,528 USD for RRP/PRP, LRP, MIERP, and RALP, respectively (These costs were calculated at the currency rate of 100 Japanese Yen=1 USD in April 2012).
Partial nephrectomy is widely accepted as a standard therapy for localized renal tumors. Surgical approaches such as open laparoscopy-assisted minimum incision have been chosen according to institutional mastership. Laparoscopic partial nephrectomy (LPN) has been performed in Japan since the 1990s, and by 2013, LPN was performed in 1,149 cases according to the results of the 12th JSES survey. However, advanced skills are required for the precise resection and suturing involved in the procedure within a limited ischemic time. Furthermore, laparoscopic procedures are challenging, and their difficulty depends on the location of the tumor, such as the renal sinus. In this regard, RALPN is very attractive for its free motion under a three-dimensional view. In 2013, 119 renal tumors were treated with RALPN according to the results of the 12th JSES survey (Fig. 2). Kobe University applied for RALPN to be considered an advanced medical treatment and it was approved by the MHLW in June 2014.
Multi-institutional clinical trials have only started to prove the clear benefits of RALPN over LPN. The primary endpoints of this procedure are renal function and cancer control. The goals of the rates of negative surgical margin and the ischemic time (≤25 minutes) are >98% and >40%, respectively. The clinical data of 1354 LPN cases from 54 Japanese institutions were used as a historical control [16]. This is a single-arm open-label trial for 100 patients with renal cell carcinoma (cT1N0M0) (http://www.mhlw.go.jp/file/05-Shingikai-12401000-Hokenkyoku-Soumuka/0000053764.pdf). If this trial is able to prove the clinical benefits of RALPN, the procedure will subsequently be covered by public health insurance in Japan.
Other types of robotic surgery for urological disease have also been performed as clinical trials in a limited number of institutions in Japan. These include RALRC and robot-assisted laparoscopic pyeloplasty (RALPP). The acceptable outcomes of RALRC were reported from Tokyo Medical University [17]. There were several presentations on the preliminary results of RALRC and RALPP for a small number of patients at the 28th Congress of JSE. These presentations mainly addressed the issues of feasibility and safety. These robotic procedures will also be submitted for approval as an advanced medical treatment.
Laparoscopic surgery for gastric cancer is an emerging minimally invasive surgery. Japan demonstrated a 10-fold increase in the use of laparoscopic surgery between 1991 and 2009 [18], accounting for 42% of laparoscopic operations for stages I and II gastric cancer in 2010 [18]. Laparoscopic distal and total gastrectomies were performed in 7,341 and 1,103 patients, respectively, in 2009 [18]. Despite the large numbers of cases performed, conclusive evidence on the long-term oncologic safety of laparoscopic gastric surgery is still pending for early gastric cancer and is certainly lacking for advanced gastric cancer [19,20]. The Japanese Gastric Cancer Association defined standard gastrectomy as resection of not less than two-thirds of the stomach with a D2 lymph node dissection with extended dissection around the stomach and upper border of the pancreas [21]. Because laparoscopic gastrectomy requires advanced surgical skills, the robotic advantages are believed to ease the learning curve [22] and also to improve surgical outcomes [23]. Fujita Health University applied for robotic-assisted gastrectomy to be considered an advanced medical treatment and this was approved by the MHLW in July 2014. A multi-institutional clinical trial has begun to prove the safety, clinical efficacy, and cost-effectiveness of the procedure. The trial is a single-arm open-label trial for 330 patients with stages I and II gastric cancer. The primary endpoint is postoperative complications corresponding to Clavien-Dindo classification [24,25,26] greater than grade III. The goal is for a complication rate of less than 6.4%. The complication rate among 801 laparoscopic gastrectomy cases from Fujita Health University, Kyoto University, and Saga University are being used as a historical control (http://www.mhlw.go.jp/file/05-Shingikai-12401000-Hokenkyoku-Soumuka/0000056538.pdf). The verification of superiority of robotic-assisted laparoscopic gastrectomy in this trial will be required for public health insurance coverage for this procedure.
Laparoscopic surgery is widely performed for rectal cancer in Japan. However, the open conversion rate is relatively high and long-term results remain a critical concern for this procedure [27]. The ability to carry out total mesorectal excision laparoscopically requires intensive training [28]. Robotic-assisted rectal surgery is attracting attention as an approach to overcome the limitations in intrapelvic operations in conventional laparoscopic surgery. However, no evidence of superiority over laparoscopic surgery has yet been found [28,29,30,31]. It has been reported that disadvantages in the early period after robot introduction include longer operation time and interference with forceps and arms [28,29,30,31]. Recently, the short-term outcomes for 113 cases including advanced rectal cancer were reported from Shizuoka Cancer Center Hospital. That report showed low morbidity and a low conversion rate, even for cases requiring complicated, robot-assisted, lateral lymph node dissection [32].
Laparoscopic surgery is a technique generally performed for treating benign gynecological diseases. Regarding malignant diseases, laparoscopic hysterectomy for endometrial cancer has recently been approved for health insurance coverage.
Similarly, robotic surgery is considered highly useful in lymphadenectomy and uterine cancer surgery, which require delicate surgical operations in a deep narrow area of the pelvic cavity [33].
In Japan, the first robotic-assisted laparoscopic radical hysterectomy (RALH) was performed in March 2009 at Tokyo Medical University; a total of 261 patients have undergone robotic surgery since then. Among them, 127 patients had malignant disease. When classified by operative procedure, RALH plus pelvic lymph node dissection were performed in 86 patients, RALH in 16, extended RALH in 15, and robotic-assisted laparoscopic semiradical hysterectomy in 10. Although one patient (0.4%) switched to laparotomy and two received allogeneic blood transfusions, no patient experienced serious complications, such as postoperative bleeding or vaginal stump dehiscence [34].
Preliminary results of RALH from several institutions were presented at the 27th annual meeting of the JSES in 2014. Although requiring a long operative time, RALH plus paraaortic or pelvic lymph node dissection was performed safely and effectively without serious complications. There have been specific issues in the gynecological field; for example, laparoscopic surgery for infertility has mainly developed, and the number of radical hysterectomies has decreased.
Transoral robotic surgery (TORS) has been reported as an otolaryngology clinical application [35,36]. In TORS, a three-dimensional endoscope and two arms of the robot are inserted through the mouth cavity to extract tumors in cases of middle or lower pharyngeal and larynx cancer. This procedure has not been widely adopted in Japan to date, because its use in the field of otolaryngology is not yet approved. In 2014, Tokyo Medical University, Kyoto University, and Tottori University jointly started a multicenter TORS clinical trial as a science research promotion project through the MHLW. A clinical trial is being conducted with 20 patients treated with TORS as advanced medical treatment, which is scheduled to be submitted for marketing approval.
Robotic-assisted thyroid surgery has been reported in a clinical study conducted in 2014 patients at four Korean institutions [37], as well as in Europe [38]. In all of these studies, this procedure exhibited superiority and resulted in comparable or fewer complications compared with the conventional method. In Japan, this procedure has been performed for a small number of patients in Tokyo Medical University and Kanazawa Medical University alone.
Long-term clinical outcomes from robotic-assisted thymectomy and lobectomy have recently been reported from Germany and the United States [40,41,42]. In Japan, outstanding operability under three-dimensional vision, a characteristic of robotic-assisted surgery, is considered useful for mediastinal disease, and the possibility of its superiority over thoracoscopic surgery is a current subject of controversy. Thymus disease of the anterior mediastinum is found in a narrow region with a major blood vessel nearby, making thoracoscopic surgery difficult in some cases. Robotic-assisted surgery, which can be sufficiently performed with a lateral approach, is considered useful for thymectomy, thymoma, and myasthenia gravis requiring elaborate surgery. The advantages of robotic-assisted surgery include its use in treating tumors at the top of the chest, tumors near the diaphragm in the posterior mediastinum, or esophageal tumors that require suturing.
Furthermore, preoperative simulation and intraoperative navigation using the SYNAPSE VINCENT (Fujifilm Corp., Tokyo, Japan) for robot-assisted thoracic surgery (RATS) have been reported to enable efficient planning of the operation settings, allowing the tumor location and depicting surrounding tissues to be detected quickly, accurately, and safely [43]. However, due to the cost of RATS, this technique has not been widely adopted. It is reported that at least 300 RATS cases per year at one institution are required to prevent a deficit in income under the Japanese Health Insurance System [44]. The judges of the Advanced Medical Treatment Expert Meeting requested that RATS be verified for higher cost-benefit performance compared to the conventional video-assisted thoracic surgery.
In curative surgery for thoracic esophageal cancer, it is important to thoroughly dissect the upper mediastinal lymph node centered around the recurrent laryngeal nerve. The major issues of this procedure are recurrent laryngeal nerve palsy and associated postoperative laryngopharynx functional impairment. An endoscopic surgery-assisting robot has several characteristics that address the issues of conventional thoracoscopic surgery, including a clear enlarged view with a three-dimensional monitor, as well as joint, motion scaling, and blurring prevention functions. A reduced incidence of recurrent laryngeal nerve palsy with the use of a robotic system was reported in a study from Fujita Health University [45].
Recently, transhiatal robotic manipulation has also been reported. In this approach, the middle mediastinal lymph node is dissected by use of a robotic approach after performing upper mediastinal lymph dissection through a cervical incision. Thus, radical esophagectomy together with three-field lymphadenectomy can be completed without any transthoracic procedure [46].
Currently, more than 180 institutions have installed the da Vinci surgical system in Japan. The most commonly performed procedure is RALP because of the limitations of health insurance coverage. Robotic-assisted partial nephrectomy and robotic-assisted gastrectomy have recently begun as advanced medical treatment to be evaluated for health insurance coverage. Other types of robotic surgery have been performed as clinical trials. The verification of superiority of outcome and cost-benefit balance over conventional laparoscopic surgery will be required. Despite the potential advantages of robotic use, robotic surgery will have a tough road to be utilized for a wide range of surgical treatments without a downward price revision of the robotic equipment.
Figures and Tables
ACKNOWLEDGMENTS
I sincerely thank Dr Fujiwara in the Department of Digestive Surgery, Osaka Medical Center for Cancer and Cardiovascular Disease, for his kind assistance in preparing the manuscript.
References
1. Yoshida M, Furukawa T, Morikawa Y, Kitagawa Y, Kitajima M. The developments and achievements of endoscopic surgery, robotic surgery and function-preserving surgery. Jpn J Clin Oncol. 2010; 40:863–869.
2. Matsuda T, Ono Y, Terachi T, Naito S, Baba S, Miki T, et al. The endoscopic surgical skill qualification system in urological laparoscopy: a novel system in Japan. J Urol. 2006; 176:2168–2172.
3. Martis G, Diana M, Ombres M, Cardi A, Mastrangeli R, Mastrangeli B. Retropubic versus perineal radical prostatectomy in early prostate cancer: eight-year experience. J Surg Oncol. 2007; 95:513–518.
4. Namiki S, Egawa S, Terachi T, Matsubara A, Igawa M, Terai A, et al. Changes in quality of life in first year after radical prostatectomy by retropubic, laparoscopic, and perineal approach: Multi-institutional longitudinal study in Japan. Urology. 2006; 67:321–327.
5. Schuessler WW, Schulam PG, Clayman RV, Kavoussi LR. Laparoscopic radical prostatectomy: initial short-term experience. Urology. 1997; 50:854–857.
6. Guillonneau B, Cathelineau X, Barret E, Rozet F, Vallancien G. Laparoscopic radical prostatectomy: technical and early oncological assessment of 40 operations. Eur Urol. 1999; 36:14–20.
7. Guillonneau B, Vallancien G. Laparoscopic radical prostatectomy: the Montsouris experience. J Urol. 2000; 163:418–422.
8. Guillonneau B, Vallancien G. Laparoscopic radical prostatectomy: the Montsouris technique. J Urol. 2000; 163:1643–1649.
9. Kihara K, Kawakami S, Fujii Y, Masuda H, Koga F. Gasless single-port access endoscopic surgery in urology: minimum incision endoscopic surgery, MIES. Int J Urol. 2009; 16:791–800.
10. Kawakami S, Kihara K. Japanese Association for Minimum-Incision Endoscopic Surgery. Japanese Urological Association. Surgical practices for urological tumors: a nation-wide survey in Japan in 2005. Int J Urol. 2009; 16:257–262.
11. Yoshioka K, Hatano T, Nakagami Y, Ozu C, Horiguchi Y, Sakamoto N, et al. First 24 Japanese cases of robotic-assisted laparoscopic radical prostatectomy using the daVinci Surgical System. Hinyokika Kiyo. 2008; 54:333–338.
12. Tozawa K, Yasui T, Umemoto Y, Mizuno K, Okada A, Kawai N, et al. Pitfalls of robot-assisted radical prostatectomy: a comparison of positive surgical margins between robotic and laparoscopic surgery. Int J Urol. 2014; 21:976–979.
13. Hoshikawa Y, Tsutsumi N, Ohkoshi K, Serizawa S, Hamada M, Inagaki K, et al. The effect of steep Trendelenburg positioning on intraocular pressure and visual function during robotic-assisted radical prostatectomy. Br J Ophthalmol. 2014; 98:305–308.
14. Raz O, Boesel TW, Arianayagam M, Lau H, Vass J, Huynh CC, et al. The effect of the modified Z trendelenburg position on intraocular pressure during robotic assisted laparoscopic radical prostatectomy: a randomized, controlled study. J Urol. 2014; 10. 23. [Epub]. http://dx.doi.org/10.1016/j.juro.2014.10.094.
15. Sugihara T, Yasunaga H, Horiguchi H, Matsui H, Fujimura T, Nishimatsu H, et al. Robot-assisted versus other types of radical prostatectomy: population-based safety and cost comparison in Japan, 2012-2013. Cancer Sci. 2014; 105:1421–1426.
16. Saito H, Matsuda T, Tanabe K, Kawauchi A, Terachi T, Nakagawa K, et al. Surgical and oncologic outcomes of laparoscopic partial nephrectomy: a Japanese multi-institutional study of 1375 patients. J Endourol. 2012; 26:652–659.
17. Gondo T, Yoshioka K, Nakagami Y, Okubo H, Hashimoto T, Satake N, et al. Robotic versus open radical cystectomy: prospective comparison of perioperative and pathologic outcomes in Japan. Jpn J Clin Oncol. 2012; 42:625–631.
18. Etoh T, Inomata M, Shiraishi N, Kitano S. Minimally invasive approaches for gastric cancer-Japanese experiences. J Surg Oncol. 2013; 107:282–288.
19. Yasunaga H, Horiguchi H, Kuwabara K, Matsuda S, Fushimi K, Hashimoto H, et al. Outcomes after laparoscopic or open distal gastrectomy for early-stage gastric cancer: a propensity-matched analysis. Ann Surg. 2013; 257:640–646.
20. Antonakis PT, Ashrafian H, Isla AM. Laparoscopic gastric surgery for cancer: where do we stand? World J Gastroenterol. 2014; 20:14280–14291.
21. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011; 14:113–123.
22. Heemskerk J, van Gemert WG, de Vries J, Greve J, Bouvy ND. Learning curves of robot-assisted laparoscopic surgery compared with conventional laparoscopic surgery: an experimental study evaluating skill acquisition of robot-assisted laparoscopic tasks compared with conventional laparoscopic tasks in inexperienced users. Surg Laparosc Endosc Percutan Tech. 2007; 17:171–174.
23. Suda K, Man-I M, Ishida Y, Kawamura Y, Satoh S, Uyama I. Potential advantages of robotic radical gastrectomy for gastric adenocarcinoma in comparison with conventional laparoscopic approach: a single institutional retrospective comparative cohort study. Surg Endosc. 2015; 29:673–685.
24. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.
25. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196.
26. Lee JH, Park do J, Kim HH, Lee HJ, Yang HK. Comparison of complications after laparoscopy-assisted distal gastrectomy and open distal gastrectomy for gastric cancer using the Clavien-Dindo classification. Surg Endosc. 2012; 26:1287–1295.
27. Toda S, Kuroyanagi H. Laparoscopic surgery for rectal cancer: current status and future perspective. Asian J Endosc Surg. 2014; 7:2–10.
28. Mak TW, Lee JF, Futaba K, Hon SS, Ngo DK, Ng SS. Robotic surgery for rectal cancer: A systematic review of current practice. World J Gastrointest Oncol. 2014; 6:184–193.
29. Hara M, Sng K, Yoo BE, Shin JW, Lee DW, Kim SH. Robotic-assisted surgery for rectal adenocarcinoma: short-term and midterm outcomes from 200 consecutive cases at a single institution. Dis Colon Rectum. 2014; 57:570–577.
30. Yamaguchi T, Kinugasa Y, Shiomi A, Sato S, Yamakawa Y, Kagawa H, et al. Learning curve for robotic-assisted surgery for rectal cancer: use of the cumulative sum method. Surg Endosc. 2014; 10. 03. [Epub]. http://dx.doi.org/10.1007/s00464-014-3855-5.
31. Kagawa H, Kinugasa Y, Shiomi A, Yamaguchi T, Tsukamoto S, Tomioka H, et al. Robotic-assisted lateral lymph node dissection for lower rectal cancer: short-term outcomes in 50 consecutive patients. Surg Endosc. 2014; 08. 19. [Epub]. http://dx.doi.org/10.1007/s00464-014-3760-y.
32. Shiomi A, Kinugasa Y, Yamaguchi T, Tomioka H, Kagawa H. Robot-assisted rectal cancer surgery: short-term outcomes for 113 consecutive patients. Int J Colorectal Dis. 2014; 29:1105–1111.
33. Isaka K, Kato R, Ito H. Uterine cancer. Gan To Kagaku Ryoho. 2014; 41:1354–1357.
34. Isaka K. Robotic-assisted surgery for malignant tumor of the uterus. In : The proceeding of the 52nd Annual Meeting of Japan Society of Clinical Oncology; 2014 Aug 28-30; Yokohama, Japan. Tokyo: Japan Society of Clinical Oncology;2014. p. 696.
35. O'Leary P, Kjærgaard T. Transoral robotic surgery and oropharyngeal cancer: a literature review. Ear Nose Throat J. 2014; 93:E14–E21.
36. Kelly K, Johnson-Obaseki S, Lumingu J, Corsten M. Oncologic, functional and surgical outcomes of primary Transoral Robotic Surgery for early squamous cell cancer of the oropharynx: a systematic review. Oral Oncol. 2014; 50:696–703.
37. Lee J, Kang SW, Jung JJ, Choi UJ, Yun JH, Nam KH, et al. Multicenter study of robotic thyroidectomy: short-term postoperative outcomes and surgeon ergonomic considerations. Ann Surg Oncol. 2011; 18:2538–2547.
38. Kuppersmith RB, Holsinger FC. Robotic thyroid surgery: an initial experience with North American patients. Laryngoscope. 2011; 121:521–526.
39. Lin HS, Folbe AJ, Carron MA, Zuliani GF, Chen W, Yoo GH, et al. Single-incision transaxillary robotic thyroidectomy: challenges and limitations in a North American population. Otolaryngol Head Neck Surg. 2012; 147:1041–1046.
40. Rückert JC, Swierzy M, Ismail M. Comparison of robotic and nonrobotic thoracoscopic thymectomy: a cohort study. J Thorac Cardiovasc Surg. 2011; 141:673–677.
41. Park BJ, Melfi F, Mussi A, Maisonneuve P, Spaggiari L, Da Silva RK, et al. Robotic lobectomy for non-small cell lung cancer (NSCLC): long-term oncologic results. J Thorac Cardiovasc Surg. 2012; 143:383–389.
42. Louie BE, Farivar AS, Aye RW, Vallieres E. Early experience with robotic lung resection results in similar operative outcomes and morbidity when compared with matched video-assisted thoracoscopic surgery cases. Ann Thorac Surg. 2012; 93:1598–1604.
43. Kajiwara N, Akata S, Hagiwara M, Yoshida K, Kato Y, Kakihana M, et al. High-speed 3-dimensional imaging in robot-assisted thoracic surgical procedures. Ann Thorac Surg. 2014; 97:2182–2184.
44. Kajiwara N, Patrick Barron J, Kato Y, Kakihana M, Ohira T, Kawate N, et al. Cost-benefit performance of robotic surgery compared with video-assisted thoracoscopic surgery under the Japanese National Health Insurance System. Ann Thorac Cardiovasc Surg. 2014; 05. 16. [Epub]. http://dx.doi.org/10.5761/atcs.oa.14-00076.
45. Suda K, Ishida Y, Kawamura Y, Inaba K, Kanaya S, Teramukai S, et al. Robot-assisted thoracoscopic lymphadenectomy along the left recurrent laryngeal nerve for esophageal squamous cell carcinoma in the prone position: technical report and short-term outcomes. World J Surg. 2012; 36:1608–1616.
46. Mori K, Yamagata Y, Wada I, Shimizu N, Nomura S, Seto Y. Robotic-assisted totally transhiatal lymphadenectomy in the middle mediastinum for esophageal cancer. J Robot Surg. 2013; 7:385–387.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download