Abstract
Purpose
Our objective was to evaluate the use of a holmium laser for transurethral deroofing of a prostatic abscess in patients with severe and multiloculated prostatic abscesses.
Materials and Methods
From January 2011 to April 2014, eight patients who were diagnosed with prostatic abscesses and who underwent transurethral holmium laser deroofing at Pusan National University Hospital were retrospectively reviewed.
Results
Multiloculated or multifocal abscess cavities were found on the preoperative computed tomography (CT) scan in all eight patients. All patients who underwent transurethral holmium laser deroofing of a prostatic abscess had successful outcomes, without the need for secondary surgery. Of the eight patients, seven underwent holmium laser enucleation of the prostate (HoLEP) for the removal of residual adenoma. Markedly reduced multiloculated abscess cavities were found in the follow-up CT in all patients. No prostatic abscess recurrence was found. Transient stress urinary incontinence was observed in three patients. The stress urinary incontinence subsided within 3 weeks in two patients and improved with conservative management within 2 months in the remaining patient.
Conclusions
Transurethral holmium laser deroofing of prostatic abscesses ensures successful drainage of the entire abscess cavity. Because we resolved the predisposing conditions of prostatic abscess, such as bladder outlet obstruction and prostatic calcification, by simultaneously conducting HoLEP, there was no recurrence of the prostatic abscesses after surgery. We recommend our method in patients requiring transurethral drainage.
Prostatic abscess is an uncommon disease caused by the widespread use of modern antibiotics [1]. However, because of the high mortality rate of prostatic abscess, which ranges from 3% to 16%, adequate and proper treatment is needed when the disease is diagnosed [2]. Once clinical suspicion of prostatic abscess is established, parenteral or oral administration of antibiotics or surgical drainage is required to reduce serious complications. However, surgical intervention is often needed, because medical treatment is usually insufficient [3,4]. Among the surgical interventions, such as open perineal drainage, transrectal ultrasound (TRUS)-guided needle aspiration, and transurethral resection of the prostatic abscess, transurethral drainage of the prostatic abscess is often performed in patients diagnosed with multiloculated abscesses, recurrent or residual abscesses, and associated bladder outlet obstruction [5]. Although many reports have focused on managing prostatic abscesses by use of conventional transurethral drainage, the use of a holmium laser to perform the transurethral approach has not yet been reported [4,5,6]. In this study, we describe the technical details of using a transurethral holmium laser for deroofing prostatic abscesses and we evaluate the effect of that procedure.
Eight patients who were diagnosed with prostatic abscesses and who underwent transurethral holmium laser deroofing at Pusan National University Hospital between January 2011 and April 2014 were included in this study. All procedures were performed in our clinic by one experienced urologist. The site of the abscess cavity was preoperatively anticipated with the findings from contrast-enhanced computed tomography (CT) scans. All patients were initially treated with parenteral antibiotics consisting of intravenous third-generation cephalosporin in combination with metronidazole. Clinical data on demographic characteristics, the surgical procedure, and preoperative and follow-up medical records were retrospectively collected in a computerized database. The study was approved by the Pusan National University Ethics Committee (PNUH IRB E-2014059).
All patients were placed in the lithotomy position under spinal anesthesia or general anesthesia depending on their general condition. The holmium:yttrium aluminium garnet laser machine (VersaPulse PowerSuite, Lumenis, Yokneam, Israel) and a 550-µm end-fire laser fiber (SlimLine 550, Lumenis) were used for the procedure. Cystoscopy was performed and the laser f iber was advanced through the working channel of the endoscope. An incision was made initially at either the 5 o'clock or the 7 o'clock position depending on the largest prostatic abscess as determined by the preoperative CT imaging. Incisions were made starting from the verumontanum and ending at the bladder neck. An additional incision at the opposite site, at 7 o'clock or 5 o'clock, may also be needed to ensure complete drainage. As the abscess cavity was opened up, the pus was drained from the cavity. During the procedure, most of the pus in the abscess cavity was washed out with continuous normal saline irrigation (Fig. 1). Unlike holmium laser enucleation of the prostate (HoLEP), transurethral holmium laser deroofing of a prostatic abscess requires no further incision or resection between 10 o'clock and 2 o'clock, because the prostatic abscess is usually not located in the anterior zone of the fibromuscular stroma [6]. During this procedure, HoLEP was performed in patients with any residual obstructive adenoma [7]. If enucleation of the residual obstructive adenoma was performed, the tissue morcellator system (VersaCut Morcellator, Lumenis) was introduced through the resectoscope and the tissue was removed. A 22-French three-way Foley catheter was inserted and continuous normal saline irrigation was instituted until the gross hematuria disappeared. All patients were catheterized during the immediate postoperative period for 1 to 7 days.
The demographic and clinical features of the eight patients who underwent transurethral holmium laser deroofing of a prostatic abscess are shown in Table 1. The mean patient age at the time of surgery was 66 years. Of the eight patients, three (37.5%) had diabetes mellitus, three (37.5%) had a recent history of an indwelling urethral catheter, and two (25%) had a history of urethral injury. The most common symptom was dysuria (100%). Four patients (66.6%) had perineal pain. Three patients (37.5%) presented with acute urinary retention. All eight patients had fever and leukocytosis. The average volume of the prostate was 83.5 mL (range, 42-162 mL). Multiloculated or multifocal abscess cavities were found on the preoperative CT scan in all eight patients (Fig. 2). The microbiological data are shown in Table 1.
All patients who underwent transurethral holmium laser deroofing had successful outcomes, without the need for secondary surgery. Of the eight patients, seven underwent HoLEP for the removal of residual adenoma. Mean operative time was 41.5 minutes (range, 28-59 minutes). The mean duration of deroofing and enucleation of the prostate was 38.5 minutes, and the mean duration of the morcellation was 3.1 minutes. No prostatic capsular perforation occurred during the operation. Our surgical procedure is demonstrated in a supplementary video clip (see Fig. 1 or Supplementary material).
All patents were treated in the hospital until a blood test determined that their leukocytosis and C-reactive protein values were normalized. A catheter-free trial was given after a mean interval of 3 days (range, 1-7 days), with all men voiding successfully. Mean length of hospitalization after surgery was 11.6 days (range, 5-32 days).
Markedly reduced multiloculated or multifocal abscess cavities were found in the follow-up CT in all patients. No prostatic abscess recurrence was found. Transient stress urinary incontinence was observed in three patients. It subsided within 3 weeks in two patients and improved with conservative management within 2 months in the remaining patient.
Prostatic abscess is a rare disease that accounts for only 0.5% to 2.5% of all prostatic diseases. Common predisposing conditions include an indwelling urethral catheter, bladder outlet obstruction, and acute and chronic prostatitis. Systemically, patients with chronic kidney disease, diabetes mellitus, and human immunodeficiency virus are also prone to the disease [8]. Once clinical suspicion of prostatic abscess is established, parenteral or oral administration of antibiotics or surgical drainage is required to reduce serious complications [9]. However, surgical interventions are of ten needed, because a monotherapy approach to medical treatment is usually insufficient [3,4]. Only one study has shown that medical treatment is successful if the abscess cavities are smaller than 1 cm in diameter, whereas larger abscesses were treated by aspiration or continuous drainage [10]. Traditionally, open perineal drainage of the prostatic abscess has been used. However, nowadays, minimally invasive drainage procedures are preferable.
Minimally invasive drainage procedures for the management of prostatic abscesses include TRUS-guided needle aspiration and transurethral drainage. TRUS-guided needle aspiration of a prostatic abscess is indicated for young patients and moribund patients [11]. Transurethral drainage is performed in patients with multiloculated abscesses, recurrent and residual abscesses, and associated bladder outlet obstruction [5]. Because all the patients in our case had multiloculated prostatic abscesses, we performed transurethral deroofing of the prostatic abscess.
Holmium laser therapy has an established role in endoscopic urology, in particular for the treatment of benign prostatic hyperplasia and urolithiasis [12,13]. Although many studies have reported on managing prostatic abscesses with conventional transurethral resection [5,6], using a holmium laser to perform a transurethral approach has not yet been reported. Compared with conventional transurethral resection of the prostatic abscess, using a holmium laser to perform transurethral deroofing of a prostatic abscess has several advantages. First, simultaneous HoLEP for the removal of residual adenoma can be performed. Indeed, some studies have reported that up to one-third of patients with prostatic abscess ultimately require transurethral resection of the prostate [6,14].
In the present study, of the eight patients who were included in our study, seven underwent HoLEP for the removal of residual adenoma. Because the prostatic abscesses of the seven patients were located between the prostate adenoma and the prostate capsule, residual adenoma was definitely observed after deroofing of the prostatic abscess. Indeed, the average volume of the prostate in our case was 83.5 mL (range, 42-162 mL). Of the eight patients, one did not undergo simultaneous HoLEP. Although his prostate volume was 70 mL, there was no obvious obstructive residual adenoma after abscess drainage. Furthermore, during the procedure, small prostatic calcifications were also removed (Fig. 1).
Shoskes et al. [15] reported that prostatic calcifications detected during TRUS are associated with prostatic inflammation and positive bacterial cultures. Indeed, in this series, small prostatic calcifications were observed during the procedure in all patients. In this context, because we removed the residual adenoma and small prostatic calcification, there was no recurrence of the prostatic abscess after surgery.
A second benefit of this procedure is that better hemostasis and shorter hospital stay can be achieved. Urosepsis is frequently observed in patients with a prostatic abscess [3]. In patients with severe infections, coagulation disorders, such as decreased platelets and disseminated intravascular coagulation, can occur [16]. Indeed, one study found that, compared to conventional transurethral resection of the prostate, HoLEP can be safely performed in fully warfarinized patients or in those who have been transitioned to low molecular weight heparin and elongated international normalized ratio [17]. Because the general condition of prostatic abscess patients tends to make them vulnerable to hemostasis, the shorter operation time achieved by using a holmium laser can result in decreased hospital stays and improved patient health recovery.
Third, there is no risk of transurethral resection syndrome. During a conventional transurethral resection procedure, we usually use nonelectrolyte solutions containing glycine, mannitol, or sorbitol. However, adverse effects due to fluid absorption may occur. These adverse effects can arise in both the cardiovascular and nervous systems [18]. However, because we use normal saline for irrigation fluid during the procedure, there is no risk of transurethral resection (TUR) syndrome. Furthermore, because the pus and debris are washed away during the procedure, better clinical outcomes for managing infection can be achieved.
During conventional transurethral drainage of a prostatic abscess, the major difficulty is that it is hard to estimate the exact depth of the prostatic abscess because the abscess is usually located between the prostate adenoma and the prostate capsule or is deep-seated in the transitional zone [5]. Because the resection plane of a prostatic abscess is the same as the resection plane for HoLEP, simultaneous HoLEP during transurethral deroofing of a prostatic abscess can be performed (Fig. 3). Furthermore, unlike HoLEP, use of a transurethral holmium laser for deroofing of prostatic abscesses requires no further incision between 10 o'clock and 2 o'clock because the prostatic abscess is usually not located at the anterior zone of the fibromuscular stroma [6]. Therefore, incisions that start at 5 o'clock or 7 o'clock of the verumontanum to the bladder neck are the easiest way to find the roof of the prostatic abscess. In this regard, transurethral holmium laser deroofing is preferable to conventional TUR drainage in the case of a prostatic abscess.
The reported rate of stress urinary incontinence at the 1-month follow-up after HoLEP ranges from 7.1% to 44.0% [19]. In our study, transient stress urinary incontinence was observed in three patients. Although their symptoms disappeared with conservative management within 2 months, the exact reason for the transient stress urinary incontinence remains speculative and multifactorial. First, over-resection of the abscess cavity can contribute to incontinence [6]. In our cases, because all the patients had a multiloculated prostatic abscess, we tended to over-resect so as to drain all the abscess cavities. Second, detrusor overactivity may be responsible for transient urinary incontinence. It has been reported that detrusor overactivity is one of the most common etiologies of urinary incontinence after transurethral resection of the prostate [20]. Furthermore, the laser energy that is applied during the procedure may contribute to postoperative urinary incontinence [21]. Third, transient external sphincter dysfunction in response to inflammation of the prostatic fossa may be responsible for transient stress urinary incontinence. In addition, the stretching of the external sphincter due to positioning the resectoscope across the external sphincter during the procedure may exasperate the normal function of the external sphincter [22].
In addition to the previously mentioned factors, use of careful surgical techniques to prevent urinary incontinence is necessary. During the surgical procedure, the bladder neck should not be resected. When the external urinary sphincter is reached, special care must be taken. For example, making an incision to the roof of the abscess cavity and the adenoma should be avoided, eliminating any guesswork about stretching and damaging the external urinary sphincter.
A limitation of this study was that a randomized control group was not available owing to the rare incidence of prostatic abscesses in the era of antibiotic use. Other limitations included the retrospective nature of the study and the short-term duration of the follow-up data.
This is the first study to report on the use of a holmium laser to drain prostatic abscesses. Transurethral holmium laser deroofing of prostatic abscesses ensures successful drainage of the entire abscess cavity. Furthermore, because we resolved the predisposing conditions of the prostatic abscess, such as bladder outlet obstruction and prostatic calcification, by simultaneously conducting HoLEP, there was no recurrence of prostatic abscesses after surgery. We recommend the use of a transurethral holmium laser for deroofing of prostatic abscesses in patients requiring transurethral drainage, especially if the abscess is multiloculated.
Figures and Tables
Fig. 1
Intraoperative images. (A) As the abscess cavity was opened up, the pus was drained from the cavity. The pus in the abscess cavity was washed out with continuous normal saline irrigation. (B) Small prostatic calcifications in the abscess cavity. Scan this QR code to see the accompanying video, or visit www.kjurology.org or http://youtu.be/zSq-kk7dQ_E.


Fig. 2
Preoperative and postoperative computed tomography (CT) scans of a patient. (A) Preoperative CT scan showing multiloculated prostatic abscesses. (B) Postoperative CT scan, which was performed at 2 weeks after surgery, showing a markedly reduced multiloculated abscess cavity.

Fig. 3
Transrectal ultrasound (TRUS) image and intraoperative image. (A) TRUS image showing that the abscess cavity (asterisk) is located between the prostate adenoma and the prostate capsule. (B) Intraoperative image showing that the opening of the prostate abscess (arrow) is located below the prostate adenoma (asterisk).
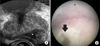
Table 1
Demographic and clinical features of eight patients with prostatic abscesses

ACKNOWLEDGMENTS
This work was supported by a clinical research grant from Pusan National University Hospital in 2013.
References
1. Weinberger M, Cytron S, Servadio C, Block C, Rosenfeld JB, Pitlik SD. Prostatic abscess in the antibiotic era. Rev Infect Dis. 1988; 10:239–249.
2. Oliveira P, Andrade JA, Porto HC, Filho JE, Vinhaes AF. Diagnosis and treatment of prostatic abscess. Int Braz J Urol. 2003; 29:30–34.
3. Aravantinos E, Kalogeras N, Zygoulakis N, Kakkas G, Anagnostou T, Melekos M. Ultrasound-guided transrectal placement of a drainage tube as therapeutic management of patients with prostatic abscess. J Endourol. 2008; 22:1751–1754.
4. Jang K, Lee DH, Lee SH, Chung BH. Treatment of prostatic abscess: case collection and comparison of treatment methods. Korean J Urol. 2012; 53:860–864.
5. El-Shazly M, El-Enzy N, El-Enzy K, Yordanov E, Hathout B, Allam A. Transurethral drainage of prostatic abscess: points of technique. Nephrourol Mon. 2012; 4:458–461.
6. Goyal NK, Goel A, Sankhwar S, Dalela D. Transurethral resection of prostate abscess: is it different from conventional transurethral resection for benign prostatic hyperplasia? ISRN Urol. 2013; 2013:109505.
7. Dusing MW, Krambeck AE, Terry C, Matlaga BR, Miller NL, Humphreys MR, et al. Holmium laser enucleation of the prostate: efficiency gained by experience and operative technique. J Urol. 2010; 184:635–640.
8. Granados EA, Riley G, Salvador J, Vincente J. Prostatic abscess: diagnosis and treatment. J Urol. 1992; 148:80–82.
9. Becker LE, Harrin WR. Prostatic abscess: a diagnostic and therapeutic approach. J Urol. 1964; 91:582–585.
10. Chou YH, Tiu CM, Liu JY, Chen JD, Chiou HJ, Chiou SY, et al. Prostatic abscess: transrectal color Doppler ultrasonic diagnosis and minimally invasive therapeutic management. Ultrasound Med Biol. 2004; 30:719–724.
11. Lim JW, Ko YT, Lee DH, Park SJ, Oh JH, Yoon Y, et al. Treatment of prostatic abscess: value of transrectal ultrasonographically guided needle aspiration. J Ultrasound Med. 2000; 19:609–617.
12. Aho TF. Holmium laser enucleation of the prostate: a paradigm shift in benign prostatic hyperplasia surgery. Ther Adv Urol. 2013; 5:245–253.
13. Pierre S, Preminger GM. Holmium laser for stone management. World J Urol. 2007; 25:235–239.
14. Bhagat SK, Kekre NS, Gopalakrishnan G, Balaji V, Mathews MS. Changing profile of prostatic abscess. Int Braz J Urol. 2008; 34:164–170.
15. Shoskes DA, Lee CT, Murphy D, Kefer J, Wood HM. Incidence and significance of prostatic stones in men with chronic prostatitis/chronic pelvic pain syndrome. Urology. 2007; 70:235–238.
16. Levi M, Schultz M, van der Poll T. Sepsis and thrombosis. Semin Thromb Hemost. 2013; 39:559–566.
17. Elzayat E, Habib E, Elhilali M. Holmium laser enucleation of the prostate in patients on anticoagulant therapy or with bleeding disorders. J Urol. 2006; 175:1428–1432.
18. Hahn RG. Fluid absorption in endoscopic surgery. Br J Anaesth. 2006; 96:8–20.
19. Cho MC, Park JH, Jeong MS, Yi JS, Ku JH, Oh SJ, et al. Predictor of de novo urinary incontinence following holmium laser enucleation of the prostate. Neurourol Urodyn. 2011; 30:1343–1349.
20. Chang PL, Tsai LH, Huang ST, Wang TM, Hsieh ML, Tsui KH. The early effect of pelvic floor muscle exercise after transurethral prostatectomy. J Urol. 1998; 160:402–405.
21. Naspro R, Bachmann A, Gilling P, Kuntz R, Madersbacher S, Montorsi F, et al. A review of the recent evidence (2006-2008) for 532-nm photoselective laser vaporisation and holmium laser enucleation of the prostate. Eur Urol. 2009; 55:1345–1357.
22. Shah HN, Mahajan AP, Hegde SS, Bansal MB. Peri-operative complications of holmium laser enucleation of the prostate: experience in the first 280 patients, and a review of literature. BJU Int. 2007; 100:94–101.
SUPPLEMENTARY MATERIALS
An accompanying video can be found in the 'urology in motion' section of the journal homepage (www.kjurology.org). The supplementary data can also be accessed by scanning a QR code located on the Fig. 1 of this article, or be available on YouTube (http://youtu.be/zSq-kk7dQ_E).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download