Abstract
Purpose
To evaluate the oncologic outcomes and postoperative complications of high-intensity focused ultrasound (HIFU) as a salvage therapy after external-beam radiotherapy (EBRT) failure in patients with prostate cancer.
Materials and Methods
Between February 2002 and August 2010, we retrospectively reviewed the medical records of all patients who underwent salvage HIFU for transrectal ultrasound-guided, biopsy-proven locally recurred prostate cancer after EBRT failure (by ASTRO definition: prostate-specific antigen [PSA] failure after three consecutive PSA increases after a nadir, with the date of failure as the point halfway between the nadir date and the first increase or any increase great enough to provoke initiation of therapy). All patients underwent prostate magnetic resonance imaging and bone scintigraphy and had no evidence of distant metastasis. Biochemical recurrence (BCR) was defined according to the Stuttgart definition (PSA nadir plus 1.2 ng/mL).
Results
A total of 13 patients with a median age of 68 years (range, 60-76 years) were included. The median pre-EBRT PSA was 21.12 ng/mL, the pre-HIFU PSA was 4.63 ng/mL, and the period of salvage HIFU after EBRT was 32.7 months. The median follow-up after salvage HIFU was 44.5 months. The overall BCR-free rate was 53.8%. In the univariate analysis, predictive factors for BCR after salvage HIFU were higher pre-EBRT PSA (p=0.037), pre-HIFU PSA (p=0.015), and short time to nadir (p=0.036). In the multivariate analysis, there were no significant predictive factors for BCR. The complication rate requiring intervention was 38.5%.
The worldwide incidence of prostate cancer is increasing rapidly [1,2]. This cancer is the second most common cause of cancer-related death in the United States [3]. Of newly diagnosed prostate cancers, 70% are detected early, are organ-confined, and may be suitable for a local curative therapy [1]. In the United States, approximately one-third of patients who are diagnosed with localized prostate cancer undergo external-beam radiotherapy (EBRT) as a primary curative treatment [4]. However, men who undergo EBRT for localized prostate cancer have a 20% to 63% chance of experiencing biochemical recurrence (BCR) [5,6].
The vast majority of patients who experience a prostate-specific antigen (PSA) level increase after EBRT will receive androgen deprivation therapy (ADT) as a palliative treatment option [7]. For patients with metastatic prostate cancer or a life expectancy of less than 5 years, this treatment may be appropriate. However, for patients with a locally recurrent prostate cancer and a life expectancy of greater than 5 years, a local curative treatment may still be possible.
Salvage therapy is defined as any treatment in an attempt to cure cancer following the failure of an initial treatment. Radical prostatectomy (RP) is an established treatment option for salvage therapy for patients with a life expectancy greater than 5 years after failure of EBRT [8]. However, most surgeons are reluctant to perform this surgery because of potentially severe postoperative complications [9]. Recently, minimally invasive treatments have been recommended as alternatives to surgery for local recurrence after EBRT failure. High-intensity focused ultrasound (HIFU) is one of the available minimally invasive salvage treatments. Ultrasound is emitted from a transrectal transducer and is focused so that it causes coagulation and necrosis in target tissue [10]. However, very few series have reported HIFU as a salvage therapy after failure of EBRT [11-13]. The aim of this study was to evaluate the oncologic outcomes and postoperative complications of HIFU as a salvage therapy after EBRT failure in patients with prostate cancer and to investigate the predictive factors for BCR after salvage HIFU treatment.
This retrospective study was approved by the Institutional Review Board of the Samsung Medical Center (IRB no. 2013-07-014). Between February 2002 and August 2010, 13 patients with prostate cancer after EBRT failure by American Society for Radiation Oncology definition (PSA failure after three consecutive PSA increases after a nadir, with the date of failure as the point halfway between the nadir date and the first increase or any increase great enough to provoke initiation of therapy [14]) underwent salvage HIFU treatment at Samsung Medical Center as a definitive local therapy. Eligibility criteria for salvage HIFU treatment included transrectal ultrasound-guided, biopsy-proven, locally recurred prostate cancer and negative metastatic evaluation confirmed by chest radiography, prostatic magnetic resonance imaging (MRI), and bone scintigraphy. Prostate MRI and bone scintigraphy were performed approximately 1 month after prostate biopsy. All patients did not want to undergo RP or were not suitable for surgery owing to comorbidities. Patients were divided into three groups according to the National Comprehensive Cancer Network (NCCN) risk classification as follows: low, intermediate, and high [15].
The salvage HIFU treatment was performed by using an Ablatherm HIFU device (EDAP SA, Lyon, France). This device uses an endorectal probe that incorporates both a 7.5-MHz imaging transducer for real-time imaging and a 3-MHz treatment transducer to ablate a volume ranging from 1.7 mm × 1.7 mm × 19 mm (0.05 mL) to 1.7 mm × 1.7 mm × 26 mm (0.08 mL). An A-mode ultrasound detection system with an external ultrasound scanner measures the length from the rectal wall, and this real-time safety monitor reduces the risk of rectal wall coagulation.
All procedures were performed under combined spinal and epidural anesthesia. Before salvage HIFU treatment, all patients received a suprapubic catheter under cystoscopic guidance to guarantee proper urinary drainage and which was planned to be removed 2 weeks after treatment, dependant on urethral voiding function. A limited transurethral resection of the prostate (TURP) was performed to reduce prolonged urinary retention before HIFU treatment when prostate volume was greater than 40 mL or a median lobe was present.
After TURP was performed and a urethral catheter was inserted, the patient was placed in the right lateral decubitus position, and the endorectal probe was inserted into the rectum and fixed in position to the HIFU table by an articulating arm. Following localization of targeted tissue boundaries by use of an integrated ultrasound imaging system, HIFU shots were delivered to the targeted lesion. The HIFU protocol included treatment of the whole gland from the bladder neck to the apex. The prostate volume was divided into four or five sections, two or three per lobe, dependent on prostate size and site of recurred prostate cancer. Initially, the left most two or three sections were ablated, and after the urethral catheter was removed, a further two or three sections were ablated. On completion of the procedure, the urethral catheter was reinserted and kept in place until discharge. Patients were discharged 2 days after the procedure with the suprapubic catheter in place.
If urethral voiding was adequate (voided volume ≥100 mL and postvoiding residual volume ≤50 mL) [16,17], the suprapubic catheter was removed after 2 weeks. After that, the patients were scheduled for a follow-up visit 1 month later, every 3 months for the first year, every 6 months until the third year, and annually thereafter, if asymptomatic. During the follow-up period, information, including continence status, digital rectal examination, and serum PSA, were routinely obtained. If there was no evidence of BCR, imaging evaluations were not performed. The PSA nadir was defined as the lowest recorded PSA level during the follow-up period, and the time to nadir was evaluated. BCR was defined according to the Stuttgart post-HIFU definition of failure (PSA nadir plus 1.2 ng/mL). Imaging evaluations, such as prostate MRI and bone scintigraphy, were performed in cases of BCR to determine if there was evidence of local recurrence or distal metastasis. Complications that occurred during the follow-up period were categorized according to the Clavien-Dindo classification of surgical complications [18] and stratified into minor (Clavien grades I-II) and major (Clavien grades III-V) complications [19].
Distributions of the BCR-free survival rate were calculated according to the Kaplan-Meier estimation method. Cox proportional hazard regression analysis was used to analyze predictive factors for BCR. A p-value <0.05 was considered statistically significant. All statistical analyses were performed with IBM SPSS ver. 20.0 (IBM Co., Armonk, NY, USA).
Patient demographics and preoperative data are summarized in Table 1. A total of 13 patients with a median age of 68 years (range, 60-76 years) were followed up for a median duration of 44.5 months. The median pre-EBRT PSA and pre-HIFU PSA were 21.12 ng/mL and 4.63 ng/mL, respectively. The pre-EBRT Gleason score was 6 to 7 in nine patients and ≥8 in three patients. The pre-HIFU Gleason score was 6 to 7 in seven patients and ≥8 in six patients. Eight of the 13 patients received ADT before HIFU treatment, and the median duration of treatment was 2 months. The median interval between HIFU and radiation therapy was 32.7 months. The median prostate volume at the time of salvage HIFU treatment was 25.0 mL. During HIFU treatment, TURP was performed in nine patients, and the median prostate resection weight was 2.0 g. The percentiles of low to intermediate and high-risk groups according to NCCN risk classification were 53.8% (n=7) and 46.2% (n=6), respectively. Comorbidities included hypertension in nine patients, diabetes mellitus in six patients, and arrhythmia in three patients. Individual clinical and pathologic characteristics are summarized according to BCR in Table 2.
The overall BCR-free survival rate was 53.8% (95% confidence interval, 26.8-80.8; Fig. 1). The pre-EBRT PSA of the patients with BCR was higher (median, 28.8 ng/mL) than that of the BCR-free patients (median, 14.1 ng/mL; p=0.046). The pre-HIFU PSA of patients with BCR was also higher (median, 8.9 ng/mL) than that of the BCR-free patients (median, 3.3 ng/mL; p=0.019). Patients with BCR had a shorter time to PSA nadir (median, 40.3 days) than did the BCR-free group (median, 112.8 days; p=0.014).
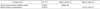
In the univariate analysis to identify factors for predicting BCR, we found that higher pre-EBRT PSA (p=0.037), pre-HIFU PSA (p=0.015), and short time to PSA nadir (p=0.036) were significant predictive factors. Age, Gleason score, NCCN risk, time from RT to HIFU, and prostate volume did not differ significantly between the BCR-free and BCR groups (Table 3). In the multivariate analysis, there were no significant predictive factors for BCR after salvage HIFU treatment.
After salvage HIFU treatment, the median hospital stay was 4 days. No patients required blood transfusion or suffered a stroke, deep vein thrombosis, or bowel dysfunction. One patient was hospitalized for 16 days secondary to a desire to have the suprapubic catheter removed and to confirm urethral voiding. During the follow-up period, three patients had grade I (requiring 0-1 pad per day) and one patient had grade II (more than one pad per day) incontinence that was resolved after pelvic floor muscle exercises. Bladder neck obstruction (grade IIIa) was seen in 5 of 13 patients who were treated by TURP, without serious complications (Table 4). No cases of acute urinary retention, urinary tract infection, anal incontinence, rectal injury, urethro-rectal fistula, or urethral stricture were observed. There was no clinical progression or metastasis in BCR-free patients.
In the present study, we investigated the BCR-free rate and postoperative complications of HIFU as a salvage therapy after EBRT failure in patients with prostate cancer and evaluated the predictive factors for BCR after salvage HIFU treatment. This study is the first to determine the role of HIFU as a salvage therapy after EBRT failure for patients with prostate cancer in Korea.
Patients with BCR after EBRT may have either a local recurrence, metastatic disease, or both. Definite local treatment after EBRT failure is indicated for local recurrence without evidence of metastasis. However, it is sometimes difficult to distinguish local recurrence from distant metastasis in the early phase of PSA elevation because bone scintigraphy, abdominal CT, or pelvic MRI may not identify micrometastatic bone and lymph node involvement [20]. Additionally, PSA is not an accurate measurement of BCR within 2 years of EBRT because the PSA "bounces" have no clinical significance during this period [21]. Moreover, prostate biopsies within this period should be interpreted carefully because delayed apoptotic cell death may confuse the pathologic results [22]. In our study, the median time from EBRT to salvage HIFU therapy was 32.7 months. This duration is sufficient to draw meaningful conclusions regarding rates of recurrence.
Patients who are thought to have localized prostate cancer after EBRT failure have been offered ADT, RP, or active surveillance. However, ADT and active surveillance are not curative options. Theoretically, salvage RP may be an excellent treatment option if recurrent prostate cancer is indeed localized. Nguyen et al. [23] reviewed the literature for oncologic outcomes of salvage RP after EBRT failure published since 1990 and reported that this treatment had a 31% to 83% cancer control rate (estimated 5-year BCR-free status). However, because the operative field exposed to radiation was altered owing to fibrosis and the affected tissue plane was obliterated, it is a technically difficult procedure and is associated with high-risk complications [24]. Touma et al. [25] reviewed reports for clinical outcomes of salvage RP after EBRT failure and reported that complication rates of rectal injury, bladder neck contracture, and incontinence were 3.3% to 50%, 9% to 28%, and 10% to 80%, respectively. Therefore, salvage RP should be considered in healthy patients with a life expectancy greater than 10 years. For other patients who have medical comorbidities or are not tolerable to the expected complications, minimally invasive and less complicated modalities have been investigated for salvage therapy after EBRT failure.
Recently, several reviews reported oncologic outcomes and postoperative complications of salvage HIFU therapy after EBRT failure. Kimura et al. [24] reviewed reports for oncologic efficacy of salvage HIFU and reported that the BCR-free survival rates were 46% to 61%. Complication rates of urinary incontinence, bladder neck obstruction, and urethro-rectal fistula after salvage HIFU therapy were 7% to 49.5%, 8.5% to 36%, and 3% to 7%, respectively [14,22,26]. In the current study, the BCR-free survival rate after salvage HIFU was 53.8%, the incontinence rate was 30.8%, there were no cases of grade III incontinence that required an artificial sphincter, and there was no rectal injury during the follow-up period. However, the occurrence of bladder neck obstruction that required intervention, such as TURP, was relatively high at 38.5%.
In general, bladder neck obstruction after HIFU therapy is caused by necrotic debris from the prostate or scar tissue. If the prostate volume exceeds 40 mL or the bladder neck is elevated, performing TURP before HIFU therapy is recommended not only to adapt the prostate gland to the limited penetration depth of ultrasound, but also to reduce the occurrence of prolonged urinary retention and bladder outlet obstruction [22,27]. In the current study, combined TURP was performed in 69.2% (9/13) of patients, and the median resection weight of the prostate was 2 g. Careful preoperative examination and combined TURP with HIFU may decrease postoperative urinary obstruction.
In the univariate analysis of pre-HIFU variables for predicting BCR after salvage HIFU therapy, pre-EBRT PSA, pre-HIFU PSA, and time to PSA nadir were significant predictors in the present study. The median time to PSA nadir of the BCR group was shorter than that of the BCR-free group (40.3 days vs. 112.8 days, p=0.014). Ganzer et al. [28] reported that the PSA nadir is an important factor for predicting BCR after HIFU. The present results not only support the role of the PSA nadir, but also suggest that the time to PSA nadir itself is a significant risk factor.
Our study had several limitations. First, it was a retrospective study and had a small population size, thus raising concerns for selection bias. Second, a relatively short follow-up period (44.5 months) may be a limitation because cancer recurrences and significant complications may be detected only with an extended follow-up period. Finally, approximately two-thirds of patients were treated by ADT before salvage HIFU and this may confound interpretations of oncologic outcomes of salvage HIFU.
Salvage HIFU provided effective oncologic control for locally recurrent prostate cancer after EBRT failure. This retrospective analysis demonstrated an overall BCR-free rate of 53.8%. The pre-EBRT PSA, pre-HIFU PSA, and time to reach PSA nadir were predictive factors for BCR. The post-HIFU complication rate requiring intervention was 38.4% and it was relatively high. Patients should be aware of the benefits and risks of salvage HIFU therapy before considering it as a treatment option. Prospective randomized controlled trials with adequate recruitment and follow-up are required to verify the effectiveness of HIFU as a salvage therapy and to manage the expected complications.
Figures and Tables
FIG. 1
Kaplan-Meier curve demonstrating the biochemical recurrence (BCR)-free survival rate after salvage high-intensity focused ultrasound (HIFU) therapy. The 5-year biochemical recurrence-free survival rate is 53.8% (95% confidence interval, 26.8-80.8).

TABLE 3
Univariate analysis of the pre-HIFU variables for predicting biochemical recurrence after salvage HIFU therapy

References
1. American Society for Therapeutic Radiology and Oncology Consensus Panel. Consensus statement: guidelines for PSA following radiation therapy. Int J Radiat Oncol Biol Phys. 1997; 37:1035–1041.
2. Crouzet S, Murat FJ, Pasticier G, Cassier P, Chapelon JY, Gelet A. High intensity focused ultrasound (HIFU) for prostate cancer: current clinical status, outcomes and future perspectives. Int J Hyperthermia. 2010; 26:796–803.
3. Ferlay J, Parkin DM, Steliarova-Foucher E. Estimates of cancer incidence and mortality in Europe in 2008. Eur J Cancer. 2010; 46:765–781.
4. Uchida T, Nakano M, Hongo S, Shoji S, Nagata Y, Satoh T, et al. High-intensity focused ultrasound therapy for prostate cancer. Int J Urol. 2012; 19:187–201.
5. Acher PL, Thwaini A, Shergill IS, Barua JM. High-intensity focused ultrasound: a potential salvage treatment for recurrent prostate cancer following radiotherapy. Expert Rev Anticancer Ther. 2006; 6:969–970.
6. Agarwal PK, Sadetsky N, Konety BR, Resnick MI, Carroll PR. Cancer of the Prostate Strategic Urological Research Endeavor (CaPSURE). Treatment failure after primary and salvage therapy for prostate cancer: likelihood, patterns of care, and outcomes. Cancer. 2008; 112:307–314.
7. Uddin Ahmed H, Cathcart P, Chalasani V, Williams A, McCartan N, Freeman A, et al. Whole-gland salvage high-intensity focused ultrasound therapy for localized prostate cancer recurrence after external beam radiation therapy. Cancer. 2012; 118:3071–3078.
8. Uchida T, Shoji S, Nakano M, Hongo S, Nitta M, Usui Y, et al. High-intensity focused ultrasound as salvage therapy for patients with recurrent prostate cancer after external beam radiation, brachytherapy or proton therapy. BJU Int. 2011; 107:378–382.
9. Sanderson KM, Penson DF, Cai J, Groshen S, Stein JP, Lieskovsky G, et al. Salvage radical prostatectomy: quality of life outcomes and long-term oncological control of radiorecurrent prostate cancer. J Urol. 2006; 176:2025–2031.
10. Rukstalis DB. Treatment options after failure of radiation therapy: a review. Rev Urol. 2002; 4:Suppl 2. S12–S17.
11. Vallancien G, Prapotnich D, Cathelineau X, Baumert H, Rozet F. Transrectal focused ultrasound combined with transurethral resection of the prostate for the treatment of localized prostate cancer: feasibility study. J Urol. 2004; 171(6 Pt 1):2265–2267.
12. Berge V, Baco E, Karlsen SJ. A prospective study of salvage high-intensity focused ultrasound for locally radiorecurrent prostate cancer: early results. Scand J Urol Nephrol. 2010; 44:223–227.
13. Crouzet S, Murat FJ, Pommier P, Poissonnier L, Pasticier G, Rouviere O, et al. Locally recurrent prostate cancer after initial radiation therapy: early salvage high-intensity focused ultrasound improves oncologic outcomes. Radiother Oncol. 2012; 105:198–202.
14. Zacharakis E, Ahmed HU, Ishaq A, Scott R, Illing R, Freeman A, et al. The feasibility and safety of high-intensity focused ultrasound as salvage therapy for recurrent prostate cancer following external beam radiotherapy. BJU Int. 2008; 102:786–792.
15. D'Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998; 280:969–974.
16. Trumbeckas D, Milonas D, Jievaltas M, Danilevicius M, Matjosaitis AJ. Influence of catheter on urinary flow during urodynamic pressure-flow study in men with symptomatic benign prostatic hyperplasia. Medicina (Kaunas). 2006; 42:15–21.
17. Kelly CE. Evaluation of voiding dysfunction and measurement of bladder volume. Rev Urol. 2004; 6:Suppl 1. S32–S37.
18. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.
19. Agarwal PK, Sammon J, Bhandari A, Dabaja A, Diaz M, Dusik-Fenton S, et al. Safety profile of robot-assisted radical prostatectomy: a standardized report of complications in 3317 patients. Eur Urol. 2011; 59:684–698.
20. Breeuwsma AJ, Pruim J, van den Bergh AC, Leliveld AM, Nijman RJ, Dierckx RA, et al. Detection of local, regional, and distant recurrence in patients with psa relapse after external-beam radiotherapy using (11)C-choline positron emission tomography. Int J Radiat Oncol Biol Phys. 2010; 77:160–164.
21. Rosser CJ, Kuban DA, Levy LB, Chichakli R, Pollack A, Lee AK, et al. Prostate specific antigen bounce phenomenon after external beam radiation for clinically localized prostate cancer. J Urol. 2002; 168:2001–2005.
22. Murat FJ, Poissonnier L, Rabilloud M, Belot A, Bouvier R, Rouviere O, et al. Mid-term results demonstrate salvage high-intensity focused ultrasound (HIFU) as an effective and acceptably morbid salvage treatment option for locally radiorecurrent prostate cancer. Eur Urol. 2009; 55:640–647.
23. Nguyen PL, D'Amico AV, Lee AK, Suh WW. Patient selection, cancer control, and complications after salvage local therapy for postradiation prostate-specific antigen failure: a systematic review of the literature. Cancer. 2007; 110:1417–1428.
24. Kimura M, Mouraviev V, Tsivian M, Mayes JM, Satoh T, Polascik TJ. Current salvage methods for recurrent prostate cancer after failure of primary radiotherapy. BJU Int. 2010; 105:191–201.
25. Touma NJ, Izawa JI, Chin JL. Current status of local salvage therapies following radiation failure for prostate cancer. J Urol. 2005; 173:373–379.
26. Gelet A, Chapelon JY, Poissonnier L, Bouvier R, Rouviere O, Curiel L, et al. Local recurrence of prostate cancer after external beam radiotherapy: early experience of salvage therapy using high-intensity focused ultrasonography. Urology. 2004; 63:625–629.
27. Sung HH, Jeong BC, Seo SI, Jeon SS, Choi HY, Lee HM. Seven years of experience with high-intensity focused ultrasound for prostate cancer: advantages and limitations. Prostate. 2012; 72:1399–1406.
28. Ganzer R, Robertson CN, Ward JF, Brown SC, Conti GN, Murat FJ, et al. Correlation of prostate-specific antigen nadir and biochemical failure after high-intensity focused ultrasound of localized prostate cancer based on the Stuttgart failure criteria-analysis from the @-Registry. BJU Int. 2011; 108(8 Pt 2):E196–E201.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download