Abstract
Purpose
Urodynamic studies are commonly performed as part of the preoperative work-up of patients undergoing surgery for stress urinary incontinence (SUI). We aimed to assess the extent to which these urodynamic parameters influence patient selection and postoperative outcomes.
Materials and Methods
Patients presenting with SUI were randomly assigned to two groups: one undergoing office evaluation only and the other with a preoperative urodynamic work-up. Patients with unfavorable urodynamic parameters (detrusor overactivity [DO] and/or Valsalva leak point pressure [VLPP]<60 cm H2O and/or maximum urethral closure pressure [MUCP]<20 cm H2O) were excluded from the urodynamic testing group. All patients in both groups underwent the transobturator midurethral sling procedure. Evaluation for treatment success (reductions in urogenital distress inventory and incontinence impact questionnaire scoring along with absent positive stress test) was done at 6 months and 1 year postoperatively.
Results
A total of 72 patients were evaluated. After 12 patients with any one or more of the abnormal urodynamic parameters were excluded, 30 patients were finally recruited in each of the "urodynamic testing" and "office evaluation only" groups. At both the 6- and the 12-month follow-ups, treatment outcomes (reduction in scores and positive provocative stress test) were significantly better in the urodynamic testing group than in the office evaluation only group (p-values significant for all outcomes).
Conclusions
Our findings showed statistically significantly better treatment outcomes in the urodynamic group (after excluding those with poor prognostic indicators such as DO, low VLPP, and MUCP) than in the office evaluation only group. We recommend exploiting the prognostic value of these urodynamic parameters for patient counseling and treatment decisions.
Changes in the pelvic floor alongside the urethral anatomy occur with aging, which can result in stress urinary incontinence (SUI). This has a socially debilitating impact and affects health care systems economically. SUI affects 4% to 35% of women [1,2,3], and up to 15% of women require further treatment for persistent or recurrent SUI after one surgical procedure [4]. Urodynamic testing is frequently utilized in the assessment of women with SUI, and urodynamic findings can predict disease severity (influence treatment recommendations) or postoperative outcome. The extent to which a complete urodynamic evaluation impacts outcomes after treatment of SUI is controversial, however [5]. Symptoms are an unreliable indicator of urodynamic findings [6], and therefore some have argued that performing urodynamic studies might improve outcome following surgery. This is achieved by both urodynamically confirming the diagnosis and by establishing the presence of other concomitant diagnoses (such as detrusor overactivity [DO], intrinsic sphincter deficiency [ISD], or detrusor dysfunction) that might affect treatment outcome [7]. For example, DO is a risk factor for failure of midurethral sling (MUS) procedures [8,9,10]. Currently, the diagnosis of ISD is unclear and there are conflicting data in the literature concerning whether a diagnosis of ISD influences the outcomes or the type of surgical treatment. Despite this lack of consensus, a maximum urethral closure pressure (MUCP) of less than 20 cm H2O and a Valsalva leak point pressure (VLPP) of less than 60 cm H2O have been the urodynamic criteria for diagnosis of ISD. MUCP correlates with passive urethral tone, whereas VLPP signifies active resistance during an episode of stress. A recently published prospective study showed that women with a low (<20 cm H2O) MUCP benefit from a retropubic tension-free vaginal tape (TVT) procedure [11]. Therefore, urodynamics can be used to select the proper MUS procedure.
Very few randomized trials on urodynamics in SUI have been carried out until now [12]. There is no conclusive evidence showing that preoperative urodynamic studies improve treatment outcome regardless of the surgical treatment chosen [13]. A Cochrane review focused on this very topic found only two studies that met the criteria for inclusion [9]. More studies are required to know the benefits of conducting urodynamics over other noninvasive office-based testing in SUI patients undergoing surgery. This is very important because urodynamics can add unnecessary expense and morbidity by introducing urinary tract infections if not indicated in the first place.
In this prospective randomized study, we aimed to assess the value of urodynamics before treatment in women with uncomplicated SUI by comparing outcomes with those of patients who underwent office evaluation only and no urodynamics.
Women presenting with predominantly SUI (defined as involuntary leakage during physical activity, coughing, or sneezing) underwent a standardized basic office evaluation and were eligible for the study if they had a history of symptoms of uncomplicated SUI for at least 3 months and failure to respond to standard medical treatment and pelvic floor exercises, a postvoid residual urine (PVRU) volume of less than 150 mL, a negative urine culture to exclude urinary tract infection, a desire for surgery for SUI, and a positive provocative stress test (defined as an observed transurethral loss of urine that was simultaneous with a cough or Valsalva maneuver). A random 150-mL cutoff for PVRU was chosen to exclude most patients with voiding dysfunction or neurogenic bladder. The provocative stress test, which had to be positive for inclusion in the study, was performed at the time of cystoscopic confirmation for SUI at a volume of approximately 300 mL along with a Bonney test. A clinical assessment of urethral mobility (defined as a straining angle of 30 degrees or greater relative to the horizontal on the Q-tip test) was also conducted at the same time.
Exclusion criteria were previous surgery for incontinence, a history of pelvic irradiation, pelvic surgery within the previous 3 months, and anterior or apical pelvic-organ prolapse beyond 1-cm proximal to the hymen (stage II and higher of the pelvic organ prolapse quantification system).
The study was conducted between September 2011 and August 2013, during which time a total of 72 women underwent randomization. Patients were randomly assigned to an "office evaluation only" group or a "urodynamic testing" group (those undergoing management based on a work-up with urodynamics). A simple 1:1 allocation was done (except if a patient was excluded from study owing to unfavorable urodynamic findings, in which case the next patient was assigned to the urodynamic group again). Written informed consent was obtained from each enrolled patient prior to their induction into the study, and ethical committee approval was obtained.
Standardized urodynamic testing included noninvasive uroflowmetry, filling cystometry with VLPP, urodynamic stress testing, pressure flow studies, and urethral pressure profilometry. These were performed on the urodynamic group prior to surgery by use of a Multichannel Urodynamics System (Dorado KT, Laborie, Toronto, Canada). The International Continence Society recommended Good Urodynamic Practice Guidelines [14] were adhered to in the research. Conventional filling cystometry was performed with the patients in the supine position by using a 6-Fr double lumen catheter. The bladder was filled at a constant rate of 20 mL per minute by using normal saline solution at room temperature for standard urodynamic study. Simultaneous abdominal pressure monitoring was obtained through a fluid-filled rectal balloon catheter. Pressures were measured by using external pressure transducers that were zeroed to atmospheric pressure by using the level of the symphysis pubis as the reference height. The presence of involuntary detrusor contractions with or without incontinence was documented, and VLPP was obtained at a bladder volume of 200 mL. With the patient having a full bladder, the resting urethral pressure profile was obtained by using a 6-Fr catheter, catheter withdrawal, and water perfusion. The mean MUCP value of three successive withdrawals was used for statistical analysis. Pressure flow study was subsequently performed with maximum cystometric capacity.
Wherever urodynamic findings indicated possible unfavorable outcomes with the transobturator tape (TOT) procedure, such as patients with DO (involuntary detrusor contractions during the filling phase with or without symptoms of urgency) or a possibility of ISD (abdominal leak point pressure<60 cm H2O or MUCP<20 cm H2O), the patients were excluded from the study and were advised to consider medical management with anticholinergics plus selective serotonin-reuptake inhibitors (in cases of DO) or another form of surgical procedure (in cases of ISD). Twelve patients who had undergone urodynamics opted for other forms of treatment (autologous pubovaginal sling with or without anticholinergics) owing to any one or more of the abnormal parameters being present as mentioned above. Finally, 30 patients in each group, i.e., preoperative urodynamic testing and office evaluation only, were included in the study.
All women in the study group underwent TOT surgery. All TOT operations done in this study were performed by a single senior surgeon, thereby ensuring the same expertise across all cases. The operating surgeon was blind to the study group to which the patient belonged, thereby removing any operator bias. Urodynamic findings such as detrusor pressures during the voiding phase did not influence tape tension during MUS surgery, because the operating surgeon was blind to the group to which the patient belonged. All patients were briefed on the possibility of voiding dysfunction postoperatively and the need for clean intermittent self-catheterization.
The data collected at the first visit for each patient were age, weight, height, body mass index, parity, duration of incontinence, menopausal status, history of smoking, history of hysterectomy or lower segment cesarian section, urethral mobility, PVRU on ultrasonography, full bladder and supine empty bladder stress test, and three-day voiding diary to measure incontinence severity. Self-reported measures included the urogenital distress inventory (UDI) and the incontinence impact questionnaire (IIQ), which were assessed preoperatively and at the 6- and 12-month follow-up visits. The UDI and IIQ were translated for Indian culture and were linguistically validated in Indian so that patients could read and write in their local language. A positive provocative test was also repeated at 12 months after surgery to assess treatment outcomes.
The two quality of life and incontinence assessment tools, the UDI-6 and the IIQ-7, are shortened versions of the original UDI and IIQ, respectively [15,16]. They have shown promise in the assessment of health-related quality of life and symptom distress and in distinguishing among different types of established urinary incontinence in the clinical setting. For scoring, item responses were assigned values of 0 for "not at all," 1 for "slightly," 2 for "moderately," and 3 for "greatly." The average score of items responded to was calculated. The average, which ranged from 0 to 3, was multiplied by 33 1/3 to put scores on a scale of 0 to 100.
Evaluation for treatment success was done at 6 months and 1 year postoperatively. The primary outcome for treatment success was clinical reduction of complaints as measured with the UDI and the IIQ (i.e., a score reduction of 70% or more) and a negative standard-volume stress test at 12 months after the onset of treatment. Treatment outcomes were compared between the urodynamic testing and office evaluation only group. Preoperative VLPP and MUCP (urodynamic testing group) were also stratified as 60-90 or >90 cm H2O and 20-40 or >40 cm H2O, respectively, and were correlated separately with outcome variables.
The statistical analysis was done by using the statistical software SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA). Chi-square test was used for nonparametric variables. Student t-test was used for comparing two groups, and one-way analysis of variance was used for multiple group comparisons. A p-value of <0.05 was stated as statistically significant.
Twelve patients who were excluded because of unfavorable urodynamic findings were lost to follow-up, and treatment outcomes were not assessed in that group. Primary outcome data were finally available for 30 women in the urodynamic testing group and 30 women in the evaluation only group. All of these 60 patients came for regular follow-up visits at both 6 and 12 months.
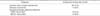
The demographic and clinical characteristics at baseline for the women in both groups are shown in Table 1. Demographic and clinical characteristics at baseline for women with primary outcome data available were generally similar between the two groups, although the data differed modestly with respect to two parameters. Specifically, women assigned to the urodynamic testing group had greater urethral mobility and were more likely to smoke.
The symptom severity of SUI before undergoing surgery in both the urodynamic testing and the office evaluation group is important because this can affect surgical outcomes. It is important to note that incontinence severity as denoted by UDI-6 and IIQ-7 scores was comparable between the groups (p=0.22 and p=0.66, respectively).
Table 2 shows the urodynamic characteristics for the 42 women who underwent urodynamic testing. Thirty women (71.4%) in this group had genuine stress incontinence confirmed by urodynamic testing. Seven women (16.7%) had DO, 9 (21.4%) had VLPP<60 cm H2O, and 8 (19.0%) had MUCP<20 cm H2O. In total, 12 women (28.6%) had to be excluded after counseling owing to unfavorable urodynamic findings. Thirty women with genuine stress incontinence underwent the TOT procedure and outcome data were evaluated in this group.
Table 3 compares the outcome success rate between the office evaluation only and urodynamic testing groups by evaluating the success criteria of 70% reduction in UDI and IIQ scores; mean change in these scores at 6 and 12 months, and provocative stress test at 12 months.
At 6 months, a 70% reduction in UDI and IIQ scores was significant in the urodynamic testing group at 86.7% and 73.3%, respectively, compared with only 60.0% and 46.7%, respectively, in the office evaluation only group (p=0.001 and p=0.001). Similarly, change in UDI and IIQ scores was -49.9 and -23.8, respectively, in the urodynamic testing group compared with -38.9 and -19.1, respectively, in the office evaluation only group (p=0.001 and p=0.002).
At the 12-month follow-up, there were mild changes in all outcome variables and p-values were similarly significant for all treatment outcomes in the two evaluation groups. At 1 year, the urodynamic testing group had a 3.3% rate of positive provocative stress test compared with 13.3% in the office evaluation only group (p<0.001).
In our study, the rate of successful treatment at 6 and 12 months among women who underwent urodynamic testing was superior to the rate among those who underwent office evaluation only. Our findings suggest that for women with uncomplicated SUI, a basic office evaluation (i.e., a positive result on a provocative stress test, a normal postvoid residual volume, an assessment of urethral mobility, and confirmation of the absence of bladder infection) is not enough and urodynamic testing helps in better selection of patients, thereby translating into better treatment outcomes.
The reliability and the clinical impact of urodynamics are among the most debated issues in urogynecology. The most recent recommendations stated by the International Consultation on Incontinence and in some large research articles [17] showed the important role of preoperative urodynamic testing in women with SUI and concomitant relevant genital prolapse. In contrast, in the literature, the available data on the use of urodynamics in cases of uncomplicated and isolated SUI are conflicting and heterogeneous. Weber et al. [18] and Laurikainen and Kiilholma [19] showed that preoperative urodynamics did not improve the effectiveness of surgery in patients treated with MUS placements for SUI. However, in a recently published literature review, Patel and Chapple [20] concluded that the evidence, while not overwhelming, points to the utility of urodynamics in diagnosis, preoperative planning, severity assessment, and prognosis of surgery for SUI.
Urodynamics can help to exclude patients with DO or ISD. Missing a diagnosis of DO could result in worsening of the urge incontinence after MUS surgery [21,22,23]. Missing a low VLPP or MUCP would obviously lead to poorer outcomes in this subset of patients. Little evidence exists for the influence of other urodynamic parameters on treatment modus or outcome in uncomplicated women with an indication for surgical treatment of SUI [21]. Therefore, in this study, we used the premise that only women with DO or a low VLPP or MUCP might benefit from urodynamics.
The aim of this study was to investigate whether the findings of DO, a low VLPP, or a low MUCP in women with predominant SUI can influence treatment outcomes. In this group of women, urodynamic results could influence preoperative counseling and the choice of surgical procedure [8,9,10,11,24]. We considered that use of these urodynamic findings might result in a change from TOT to alternate therapy. To determine whether urodynamic studies might improve treatment outcomes and to avoid any bias about the form of treatment, we compared postoperative results only among the 30 women in each study group who underwent TOT implantation. It can be admitted that the 12 women excluded from the urodynamic group did receive the benefit of alternate forms of therapy on the basis of their poor prognostic urodynamic findings.
Our finding that preoperative urodynamic tests improve the rate of treatment success may be explained by several factors. Factors such as DO and ISD identified on preoperative urodynamic testing have traditionally been considered to increase the risk of a poor outcome after surgery for stress incontinence. O'Connor et al. [25] suggested that VLPP might provide prognostic information. In a series of 43 patients with SUI who underwent TVT obturator surgery, they observed, with a very short follow-up, that 77% of patients with a preoperative VLPP>60 cm H2O were cured compared with only 25% of patients with a VLPP<60 cm H2O. Romancik et al. [26] specifically investigated VLPP as an outcome-predicting factor in 65 patients who underwent TOT and found cure and success rates to be significantly higher in patients with VLPP>60 cm H2O (78% and 100%, respectively) compared with patients with VLPP<60 cm H2O (25% and 78%, p<0.005 and p<0.025, respectively).
Urodynamic findings cause physicians to not only change their clinical diagnosis (e.g., diagnoses of overactive bladder and ISD), but may also bring about changes in surgical management or surgical outcome. Schierlitz et al. [11] found that women with a low MUCP performed significantly better after a TVT procedure compared with TOT. Six months after surgery, 21% had urodynamic stress incontinence in the TVT group compared with 45% in the TOT group. Furthermore, nine women in the TOT group underwent repeat sling surgery compared with none in the TVT group. These findings were confirmed in other studies [27,28,29]. In a series of 658 patients, Abdel-Hady and Constantine [30] investigated the efficacy of TVT in 80 women with a low VLPP (<60 cm H2O) and reported an 86% cure rate (dry) and a 14% improved rate (wet but improved) at 6 months. They concluded that the high efficacy of TVT makes it the first choice of treatment for women with SUI, including those with low VLPP.
On further comparison of treatment outcomes with stratified values for VLPP and MUCP (Tables 4, 5), we found no significant correlations except for a modest difference in 70% reduction in IIQ scores at both 6 and 12 months in the VLPP 60-90 and VLPP>90 cm H2O groups. These findings could be explained by VLPP<60 cm H2O and MUCP<20 cm H2O representing threshold values as far as influencing treatment outcomes. Further changes in VLPP and MUCP beyond these values may not have the same impact. However, the possibility of other threshold values does exist and can be the subject of further research.
A possible drawback of this model is women with voiding dysfunction. Voiding dysfunction can be present without symptoms and without a preexisting history. This group was not properly identified in the present study. However, because patients with known postvoiding bladder retention of more than 150 mL were excluded from this study, this group is likely to have been very small. A randomized clinical trial of the Burch colposuspension versus the autologous fascial sling showed that typical urodynamic measures did not predict the risk of postoperative voiding dysfunction [13].
Unlike many prior studies in which cure of stress incontinence was used as the primary outcome measure, we chose a broader measure of lower urinary tract function in terms of quality of life to determine any potential benefit of urodynamic testing. The UDI-6 determines the risk of postoperative adverse effects such as urinary urgency, urinary frequency, urgency incontinence, or voiding dysfunction. The IIQ-7 assesses the patient for activities, relationships, and feelings being affected by urine leakage.
We found urodynamic predictors to be important for treatment outcomes after TOT implantation. Our findings showed statistically significantly better treatment outcomes in the urodynamic group (after excluding those with poor prognostic indicators such as DO, low VLPP, and low MUCP) than in the office evaluation only group. Taking into consideration all of the above, we recommend exploiting the prognostic value of these urodynamic parameters for patient counseling and treatment decisions. Larger validated studies are needed, however, to derive any definite conclusions.
Figures and Tables
References
1. Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010; 29:4–20.
2. Luber KM. The definition, prevalence, and risk factors for stress urinary incontinence. Rev Urol. 2004; 6:Suppl 3. S3–S9.
3. Kane AR, Nager CW. Midurethral slings for stress urinary incontinence. Clin Obstet Gynecol. 2008; 51:124–135.
4. Jonsson Funk M, Siddiqui NY, Kawasaki A, Wu JM. Long-term outcomes after stress urinary incontinence surgery. Obstet Gynecol. 2012; 120:83–90.
5. Lemack GE. Use of urodynamics prior to surgery for urinary incontinence: how helpful is preoperative testing? Indian J Urol. 2007; 23:142–147.
6. Cundiff GW, Harris RL, Coates KW, Bump RC. Clinical predictors of urinary incontinence in women. Am J Obstet Gynecol. 1997; 177:262–266.
7. Handa VL, Jensen JK, Ostergard DR. Federal guidelines for the management of urinary incontinence in the United States: which patients should undergo urodynamic testing? Int Urogynecol J. 1995; 6:198–203.
8. Houwert RM, Venema PL, Aquarius AE, Bruinse HW, Kil PJ, Vervest HA. Predictive value of urodynamics on outcome after midurethral sling surgery for female stress urinary incontinence. Am J Obstet Gynecol. 2009; 200:649.e1–649.e12.
9. Glazener CM, Lapitan MC. Urodynamic investigations for management of urinary incontinence in adults. Cochrane Database Syst Rev. 2002; (3):CD003195.
10. Kuo HC. Effect of detrusor function on the therapeutic outcome of a suburethral sling procedure using a polypropylene sling for stress urinary incontinence in women. Scand J Urol Nephrol. 2007; 41:138–143.
11. Schierlitz L, Dwyer PL, Rosamilia A, Murray C, Thomas E, De Souza A, et al. Effectiveness of tension-free vaginal tape compared with transobturator tape in women with stress urinary incontinence and intrinsic sphincter deficiency: a randomized controlled trial. Obstet Gynecol. 2008; 112:1253–1261.
12. Nager CW, Brubaker L, Litman HJ, Zyczynski HM, Varner RE, Amundsen C, et al. A randomized trial of urodynamic testing before stress-incontinence surgery. N Engl J Med. 2012; 366:1987–1997.
13. Lemack GE, Krauss S, Litman H, FitzGerald MP, Chai T, Nager C, et al. Normal preoperative urodynamic testing does not predict voiding dysfunction after Burch colposuspension versus pubovaginal sling. J Urol. 2008; 180:2076–2080.
14. Schäfer W, Abrams P, Liao L, Mattiasson A, Pesce F, Spangberg A, et al. Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn. 2002; 21:261–274.
15. Shumaker SA, Wyman JF, Uebersax JS, McClish D, Fantl JA. Health-related quality of life measures for women with urinary incontinence: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Continence Program in Women (CPW) Research Group. Qual Life Res. 1994; 3:291–306.
16. Uebersax JS, Wyman JF, Shumaker SA, McClish DK, Fantl JA. Short forms to assess life quality and symptom distress for urinary incontinence in women: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Continence Program for Women Research Group. Neurourol Urodyn. 1995; 14:131–139.
17. Serati M, Salvatore S, Siesto G, Cattoni E, Braga A, Sorice P, et al. Urinary symptoms and urodynamic findings in women with pelvic organ prolapse: is there a correlation? Results of an artificial neural network analysis? Eur Urol. 2011; 60:253–260.
18. Weber AM, Taylor RJ, Wei JT, Lemack G, Piedmonte MR, Walters MD. The cost-effectiveness of preoperative testing (basic office assessment vs. urodynamics) for stress urinary incontinence in women. BJU Int. 2002; 89:356–363.
19. Laurikainen E, Kiilholma P. The tension-free vaginal tape procedure for female urinary incontinence without preoperative urodynamic evaluation. J Am Coll Surg. 2003; 196:579–583.
20. Patel AK, Chapple CR. Urodynamics in the management of female stress incontinence: which test and when? Curr Opin Urol. 2008; 18:359–364.
21. Fletcher SG, Lemack GE. Clarifying the role of urodynamics in the preoperative evaluation of stress urinary incontinence. ScientificWorldJournal. 2008; 8:1259–1268.
22. Gamble TL, Botros SM, Beaumont JL, Goldberg RP, Miller JJ, Adeyanju O, et al. Predictors of persistent detrusor overactivity after transvaginal sling procedures. Am J Obstet Gynecol. 2008; 199:696.e1–696.e7.
23. Panayi DC, Duckett J, Digesu GA, Camarata M, Basu M, Khullar V. et al. Pre-operative opening detrusor pressure is predictive of detrusor overactivity following TVT in patients with pre-operative mixed urinary incontinence. Neurourol Urodyn. 2009; 28:82–85.
24. Houwert RM, Venema PL, Aquarius AE, Bruinse HW, Roovers JP, Vervest HA. Risk factors for failure of retropubic and transobturator midurethral slings. Am J Obstet Gynecol. 2009; 201:202.e1–202.e8.
25. O'Connor RC, Nanigian DK, Lyon MB, Ellison LM, Bales GT, Stone AR. Early outcomes of mid-urethral slings for female stress urinary incontinence stratified by valsalva leak point pressure. Neurourol Urodyn. 2006; 25:685–688.
26. Romancik M, Lutter I, Goncalves F, Pechan J, Obsitnik M, Weibl P, et al. Valsalva leak point pressure predicts outcome after transobturator suburethral tape implantation--fact or fiction? Bratisl Lek Listy. 2006; 107:426–429.
27. Miller JJ, Botros SM, Akl MN, Aschkenazi SO, Beaumont JL, Goldberg RP, et al. Is transobturator tape as effective as tension-free vaginal tape in patients with borderline maximum urethral closure pressure? Am J Obstet Gynecol. 2006; 195:1799–1804.
28. Jung HJ, Yim GW, Jeon MJ, Kim SK, Bai SW. Preoperative maximum urethral closure pressure and valsalva leak point pressure as predictive parameters for midurethral sling. J Reprod Med. 2009; 54:436–440.
29. Gungorduk K, Celebi I, Ark C, Celikkol O, Yildirim G. Which type of mid-urethral sling procedure should be chosen for treatment of stress urinary incontinance with intrinsic sphincter deficiency? Tension-free vaginal tape or transobturator tape. Acta Obstet Gynecol Scand. 2009; 88:920–926.
30. Abdel-Hady el-S, Constantine G. Outcome of the use of tension-free vaginal tape in women with mixed urinary incontinence, previous failed surgery, or low valsalva pressure. J Obstet Gynaecol Res. 2005; 31:38–42.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download