Abstract
Urinary catheterization is a common procedure, particularly among patients with neurogenic bladder secondary to spinal cord injury. Urethral catheterization is associated with the well-recognized complications of catheter-associated urinary tract infections and limited genitourinary trauma. Unintentional ureteral cannulation represents a rare complication of urethral catheterization and has been previously described in only eight cases within the literature. We describe two cases of aberrant ureteral cannulation involving two patients with quadriplegia. These cases along with prior reports identify the spastic, insensate bladder and altered pelvic sensorium found in upper motor neuron syndromes as major risk factors for ureteral cannulation with a urinary catheter.
Urinary catheterization is a common procedure, particularly among patients with neurogenic bladder secondary to spinal cord injury (SCI). The specific bladder dysfunction related to SCI depends on both the level of cord injury and the duration of time passed since the original injury. Patients with hyperactive and flaccid bladder secondary to SCI are often managed with long-term urethral or suprapubic catheterization. Urethral catheterization is associated with the well-recognized complications of catheter-associated urinary tract infections (UTIs) and limited genitourinary trauma [1]. Unintentional ureteral cannulation represents a rare complication of urethral catheterization and has been previously described in only eight cases within the literature [2,3,4,5,6,7,8,9]. We describe two cases of aberrant ureteral cannulation involving two patients with quadriplegia seen at our institution. These cases along with prior reports identify the spastic, insensate bladder and altered pelvic sensorium found in upper motor neuron syndromes as major risk factors for ureteral cannulation with a urinary catheter.
A 48-year-old quadriplegic female with a chronic indwelling Foley catheter secondary to neurogenic bladder from a C6 SCI presented to the Emergency Department (ED) with a 1-day history of acute right flank pain and visualized blood clots within her catheter bag. She reported having last changed her catheter earlier that afternoon.
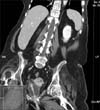
Upon presentation to the ED, the patient was found to be hypertensive (206/129 mmHg). Initial laboratory results revealed leukocytosis (12.9×109/L), and urinalysis was significant for >100 red blood cells (RBCs) and 4-10 white blood cells (WBCs). Urine gram stain and nitrates were negative. Electrolyte panel demonstrated normal renal function (creatinine level, 0.6 mg/dL; estimated glomerular filtration rate>60 mL/min/body surface area). A contrast computed tomography (CT) scan of her abdomen/pelvis revealed cannulation of the right distal ureter by the Foley catheter with the tubing extending 1 cm into the distal right ureter; mild right hydronephrosis was also visualized with diffuse enhancement of the right urinary collecting system consistent with inflammation and infection (Fig. 1). Careful review of the images showed the Foley catheter balloon completely filling this patient's small spastic bladder. The catheter was emergently removed and replaced with a new catheter device. After replacement of the Foley catheter, the patient's exaggerated autonomic response, pain, hematuria, and leukocytosis rapidly resolved.
A 68-year-old gentleman with a history of C4-5 quadriplegia complicated by neurogenic bladder and recurrent UTIs as well as known left-sided urolithiasis presented to the ED with a 1-day history of hematuria and abdominal pain. On presentation, the patient was afebrile (36.7℃) and normotensive (120/83 mmHg); initial labs demonstrated leukocytosis (12.9×109/L), and urine microscopy detailed >100 RBCs/high power field (HPF) as well as >100 WBCs/HPF. The urine gram stain was negative. Physical examination demonstrated the presence of multiple blood clots within the patient's undergarments. A three-way urinary catheter was placed to facilitate continuous bladder irrigation, which yielded further expression of numerous blood clots.
The following day, a CT urogram was performed that showed obstruction of the right distal ureter by the Foley catheter resulting in mild to moderate pyeloureterectasis (Fig. 2). The indwelling catheter was promptly readjusted and continuous bladder irrigation was stopped. Over the following 24 hours, manual irrigation of the catheter demonstrated marked improvement in the patient's hematuria.
Urinary catheterization is a common practice whose most frequent complications include catheter-associated infections and genitourinary trauma [1]. In patients in whom indwelling or intermittent catheterization represents a daily component of a health maintenance routine, the risk for catheter-associated complications increases. Within the hospital setting, others have reported that approximately 1.8% of total Foley catheter days are associated with possible UTI episodes, whereas 1.5% of Foley catheter days are associated with genitourinary trauma [1]. Urinary catheter-associated trauma is commonly inclusive for urethral damage resulting in hematuria, accidental removal of the catheter without sufficient balloon deflation, or false passage creation [1,10].
The two cases of ureteral cannulation we identified from our institution prompted us to review the literature for similar cases. Our review identified eight previous cases involving ureteral cannulation in the setting of urinary catheterization. The details of these cases are included in Table 1 [2,3,4,5,6,7,8,9]. These cases occurred between the ages of 26 and 77 years, with the majority occurring after the fifth decade of life. Including our two presented cases, 80% of complications entailed female patients, and 5 patients (50%) had known neurologic conditions (paraplegia [2,5], quadriplegia, or multiple sclerosis with autonomic dysreflexia [9]) traditionally associated with bladder dysfunction. An additional two cannulation cases occurred secondary to iatrogenic placement during surgical procedures [6,7]. Interestingly, four of the patients with underlying neurological conditions experienced cannulation of the right ureter while both iatrogenic placements during surgery occurred on the left. Additionally, all patients experiencing left-sided ureteral cannulation were female.
Cord injuries above the conus medullaris contribute to an upper motor neuron syndrome and may lead to bladder hyperactivity resulting in bladder spasm, urgency, and incontinence. Over time, the reduction in bladder capacity as well as bladder and bladder sphincter hyperactivity may also lead to elevated bladder pressures, which results in increased vesicoureteral reflux. Spinal cord injuries involving the conus medullaris or caudae equina cause a lower motor neuron syndrome that can lead to bladder flaccidity and urinary retention. Others have proposed that the underlying mechanism of ureter cannulation may be attributed to insertion of the Foley catheter during bladder contraction [5,8]. The findings from this series and review of existing cases suggest that individuals with bladder dysfunction due to upper motor neuron disease are at the highest risk for this complication among patients undergoing urethral catheterization. We suggest that this population is particularly at risk because of their small spastic bladders and altered pain perception. Those patients identified as having experienced this complication through iatrogenic placement under surgical anesthesia [6,7] and with a history of fibrotic bladder [4] further implicate diminished pain perception as a major contributor to this adverse event.
Confirmation of urinary catheter placement typically constitutes the visualization of urine flow into the collection tubing as well as subjective resistance after inflation of the retaining balloon. However, these methods of confirmation remain error prone, particularly in the setting of frequent catheterization. In patients who experience the complication of ureteral cannulation shortly after catheter placement during a surgical procedure, aberrant ureteral placement during introduction is the most likely scenario. However, in many cases, particularly in patients with underlying neurologic conditions, it is unclear whether ureteral cannulation occurs during the initial introduction of the catheter device or after subsequent migration. Traditionally, patients are instructed that if they experience resistance to instillation, pain, or autonomic instability, catheter placement should be adjusted. However, patients with neurologic sequelae are often unable to rely upon these clues as a means of detecting a catheter-associated complication. Additionally, given the unclear role that catheter migration may play in the development of ureteral cannulation, patients should also be instructed to monitor for adequate urine flow not solely at the time of catheter placement, but on a continuing basis. Given the observed association between autonomic dysreflexia and ureteral cannulation, patients with upper motor neuron disease or altered pelvic sensorium and a history of indwelling or intermittent catheterization presenting with autonomic instability should prompt evaluation for irregular catheter placement.
As observed within the presented cases, complications of ureteral cannulation are inclusive for hydronephrosis and pyeloureterectasis in addition to various mechanisms of ureteral injury or possible ureteral rupture. These complications may subsequently contribute to infectious processes such as UTI, abscess formation, or even fistulous formation [9]. Following suspected or confirmed ureteral cannulation, manual removal of the catheter following deflation of the catheter bulb should be attempted, if possible, and further management decisions including surgical intervention should be based upon clinical correlation with consideration given to the timing of the resulting complication or injury [9].
Ureteral cannulation represents a rare complication of urinary catheterization. Review of known cases identifies patients with bladder dysfunction due to upper motor neuron syndromes as the population at highest risk for developing this complication, particularly among female patients. The contributing features of underlying neurological disease suggest that the elements of bladder contraction and altered sensorium significantly add to the increased danger appreciated within this high-risk population. Those patients at high risk should be educated at regular intervals regarding the importance of safe, aseptic placement and monitoring techniques at both initiation of and continuing Foley catheter use.
Figures and Tables
FIG. 1
Computed tomography of the abdomen and pelvis with intravenous contrast demonstrating cannulation of the right distal ureter with a Foley catheter extending 1 cm into the distal ureter.
References
1. Leuck AM, Wright D, Ellingson L, Kraemer L, Kuskowski MA, Johnson JR. Complications of Foley catheters: is infection the greatest risk? J Urol. 2012; 187:1662–1666.
2. Singh NP, Eardley I. An uncommon complication of urethral catheterization. Br J Urol. 1996; 77:316–317.
3. Ogan K, Berger RM. Aberrant Foley catheter placement into the proximal right ureter. BJU Int. 2001; 88:124.
4. Muneer A, Minhas S, Harrison SC. Aberrant Foley catheter placement into the proximal right ureter. BJU Int. 2002; 89:795.
5. Kim MK, Park K. Unusual complication of urethral catheterization: a case report. J Korean Med Sci. 2008; 23:161–162.
6. Papacharalabous E, Ford M, Butler-Manuel S, Tailor A. Inadvertent insertion of a Foley's catheter through the orifice of a duplex ureter during catheterisation for laparotomy. Gynecol Surg. 2011; 8:99–101.
7. Hara N, Koike H, Bilim V, Takahashi K. Placement of a urethral catheter into the ureter: An unexpected complication after retropubic suspension. Int J Urol. 2005; 12:217–219.
8. Kato H. Incorrect positioning of an indwelling urethral catheter in the ureter. Int J Urol. 1997; 4:417–418.
9. Baker KS, Dane B, Edelstein Y, Malhotra A, Gould E. Ureteral rupture from aberrant Foley catheter placement: a case report. J Radiol Case Rep. 2013; 7:33–40.
10. St Luce S, Ninan AC, Hall JA, Kimberl IJ, Petros JA, Issa MM. Role of transrectal ultrasonography in diagnosis and treatment of retained Foley catheter. Urology. 2005; 65:1001.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download