Abstract
Purpose
Although transurethral resection of the prostate (TURP) is considered the standard surgical treatment for benign prostatic hyperplasia (BPH), Holmium laser enucleation of the prostate (HoLEP) is replacing TURP. We compared TURP with HoLEP with matching for prostate size.
Materials and Methods
We retrospectively reviewed the medical charts of patients who underwent TURP and HoLEP performed by one surgeon at our institute. All patients were categorized into 3 groups on the basis of prostate size (group 1, <40 g; group 2, 40-79 g; and group 3, >80 g), and 45 patients were selected for each method.
Results
No major intraoperative complications were encountered. The mean resected tissue weight was 6.3, 18.3, and 28.0 g for groups 1, 2, and 3, respectively, for TURP and 8.7, 25.0, and 39.8 g, respectively, for HoLEP. The mean operation time was 51.8, 89.3, and 101.9 minutes for TURP and 83.6, 122.8, and 131.2 minutes for HoLEP in groups 1, 2, and 3, respectively. HoLEP had better resection efficacy than TURP for any size prostate, but there was no statistical difference between the methods. Both methods resulted in an immediate and significant improvement of International Prostate Symptom Score, peak urinary flow rates, and postvoid residual urine volume.
The modern strategy for managing benign prostatic hyperplasia (BPH) has focused on medical treatment over radical treatment. Since its introduction, transurethral resection of the prostate (TURP) has been considered the gold standard for surgical treatment of symptomatic BPH. In the past, cases with relatively less prostate enlargement underwent TURP, whereas cases of larger prostate enlargement underwent open prostatectomy. Concerns over complications associated with invasive procedures remained, however, because cases with an overly enlarged prostate are technically more difficult to resect safely, and transurethral resection (TUR) syndrome can occur owing to the longer operating time [1].
Holmium laser enucleation of the prostate (HoLEP), which was first introduced by Gilling et al. [2] in 1995, replicates open prostatectomy in an endoscopic procedure that facilitates complete surgical removal of the prostate. It has become the gold standard for surgical treatment of BPH because of the low incidence of complications. HoLEP is well-known for its effectiveness on large prostates; however, recently it has been tried on prostates of various sizes [3]. Only a few studies have compared the results of TURP and HoLEP according to prostate size. We therefore compared clinical outcomes between TURP and HoLEP in cases matched for prostate size.
The study was conducted retrospectively on 266 patients (TURP, n=138; HoLEP, n=128) presenting with symptoms of BPH who were surgically treated by one surgeon in our hospital between 2006 and 2013. Almost all surgeries for BPH have been performed by use of a holmium laser since it became available in our center. Patients who had neurogenic bladder, urinary tract infection, prostate cancer, bladder cancer, or acute urinary retention were excluded from the study. The first 20 patients who underwent HoLEP were also excluded to accommodate the learning curve of the new procedure. This study was approved by our Institutional Review Board.
The TURP and HoLEP groups were further divided into three subgroups according to prostate volume (group 1, <40 g; group 2, 40-79 g, and group 3, >80 g). Fifteen patients who had a similar age, prostate size, and International Prostate Symptom Score (IPSS) were selected from each group.
Prostate-specific antigen (PSA), IPSS, uroflowmetry, and prostate volume through transrectal ultrasonography (TRUS) were determined before surgery. Duration of surgery, amount of tissue removed, decrease in hemoglobin after surgery, and duration of Foley catheterization were the factors included in the analysis. Improvement of symptoms and incidence of complications were retrospectively analyzed by checking uroflowmetry and IPSS at 4 to 6 weeks after surgery. If the PSA value was high before surgery, the surgery was performed after confirming the absence of prostate cancer through a prostate biopsy.
A 72-W OmniPulse (Trimedyne Inc., Irvine, CA, USA) was used for the HoLEP, which was performed by following the method reported by Gilling et al. [4]. The energy source consisted of a 72-W holmium: yttrium aluminium garnet laser with a 550-µm laser fiber. Enucleated prostatic tissue was removed by transurethral morcellation by use of a mechanical morcellator (Richard Wolf, Knittlingen, Germany) introduced through an offset rigid nephroscope. The bladder was kept distended during morcellation and the morcellator was facing the upside. The urethral catheter was removed once the urine became and remained clear.
Statistical analysis was performed by using SPSS ver. 14 (SPSS Inc., Chicago, IL, USA). Student t-test or the Mann-Whitney U-test was applied to compare the clinical parameters of each group. Chi-square test was used to compare the rate of complications between the groups. Values of p<0.05 were considered as statistically significant.
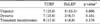
The mean age of the patients in the TURP group was 71.0 years and the mean age in the HoLEP group was 70.3 years (p=0.662). There was no significant difference in prostate size between the TURP and HoLEP groups (61.8 g vs. 61.8 g, p=0.984). There was also no significant difference between the two groups in terms of preoperative PSA (4.79 ng/mL vs. 4.15 ng/mL, p=0.487), IPSS, preoperative maximal urinary flow rate (7.3 mL/s vs. 6.7 mL/s, p=0.474), or residual urine after voiding (129.8 mL vs. 127.1 mL, p=0.922) (Table 1). Prostate volume was similar in both groups (Table 2).
Duration of surgery was longer in the HoLEP group (80.7 minutes vs. 112.6 minutes, p<0.05), and the amount of tissue removed was also larger in the HoLEP group (17.3 g vs. 24.2 g, p<0.05). There was no significant difference in hemoglobin decrease during surgery between the two groups (p=0.950). The maintenance period for the Foley catheter was longer in the TURP group (3.7 days vs. 2.5 days, p<0.05). The maximal urinary flow rate after surgery was higher in the HoLEP group (6.0 mL/s vs. 8.6 mL/s, p<0.05), and improvement of voiding symptoms was better in the HoLEP group even though there was no statistically significant difference in IPSS between the two groups (6.5 vs. 8.1, p=0.194).
There were more grades I and II complications in the TURP group, but the difference was not statistically significant. There were no grade III or higher complications in either group. Complications that occurred in the TURP group were as follows: one case of keeping a urethral catheter owing to failure of self-voiding, two cases of fever, two cases of clot retention, and two cases of transient inability to self-void. Two cases of minimal urethral injury, two cases of transient inability to self-void, and one case of clot retention were seen in the HoLEP group (Table 3).
In group 1, the duration of surgery was longer in the HoLEP group (51.8 minutes vs. 83.6 minutes, p<0.05). The amount of tissue removed was larger in the HoLEP group but the difference was not statistically significant (6.3 g vs. 8.7 g, p=0.769). There was no significant difference in improvement of the IPSS. The maximal urinary flow rate was higher in the HoLEP group but was not significant. In group 2, the duration of surgery was longer (89.3 minutes vs. 122.8 minutes, p<0.05), and the amount of tissue removed was significantly larger in the HoLEP group (18.3 g vs. 25.0 g, p<0.05). In group 3, there was no significant difference in duration of surgery between the two groups (101.9 minutes vs. 131.2 minutes, p=0.091); however, the amount of tissue removed was larger in the HoLEP group (28.0 g vs. 39.8 g, p<0.05). There was no significant difference in terms of improvement of the IPSS between the two groups (Table 4).
There was no significant difference in the enucleation ratio (calculated by measuring the amount of removed tissue against the size of the transition zone; 0.636 vs. 0.685, p=0.603) and no significant difference in prostate volume between the two groups. The ratio of tissue removed in the HoLEP group was higher in group 3 but was not statistically significant (Table 5).
Transient dysuria occurred in 15.6% (n=7) of patients after TURP and in 6.7% (n=3) after HoLEP (p<0.05). The incidence of stress incontinence was 17.8% (n=8) in the TURP group and 8.9% (n=4) in the HoLEP group (p=0.178). Postsurgery urgency was seen in seven cases in the TURP group and in six cases in the HoLEP group (p=0.688). All cases improved after treatment (Table 6).
Since HoLEP was first introduced, it has rapidly replaced TURP as the gold standard for the surgical treatment of symptomatic BPH. Consequently, HoLEP is now the most rigorously studied surgical technique. HoLEP is stably being performed on various sizes of the prostate, and the result of treatment is excellent according to several recent studies.
As in previous studies, duration of surgery in our patients was longer and the amount of tissue removed was larger in the HoLEP group [5]. Improvements in IPSS after surgery were similar in the groups, but the increase in maximal urinary flow rate was higher in the HoLEP group because there was more tissue to be removed. HoLEP was more effective than TURP in the management of cases with a larger prostate volume in this study. For small prostates, HoLEP was comparable to TURP in terms of maximal urinary flow rate.
The most difficult issue with performing HoLEP is the steep learning curve. Although not shown in this study, 20 cases were required to achieve regular resection efficacy, which is similar to other reports [6,7]. TURP could allow for enough prostatic tissue to be removed in cases with a larger prostate because this procedure has been performed for a long time by a skilled surgeon. The relatively short learning period for HoLEP was expected owing to the surgeon's familiarity with transurethral prostate surgery.
In a previous report [8], the HoLEP group showed less blood loss and complications than in the TURP group. No patient needed transfusion in our study. In cases with a large prostate, the HoLEP group showed a lesser decrease in hemoglobin than in the TURP group (1.3 mg/dL vs. 0.3 mg/dL, p=0.014) during the operation.
It is difficult to accurately compare the occurrence of complications because of the small number of patients in this study. However, no statistically significant difference in the occurrence of severe complications was seen between the methods. Among the 128 patients who underwent HoLEP, two cases (1.6%) needed transfusion and one case (0.8%) required reoperation owing to persistent bleeding. However, these cases were excluded from the study cohort during patient selection. In previous studies investigating complications, no differences were reported in the incidence of urgency, dysuria, or stress incontinence between the two methods [9], which was similar to the results of our study. The ratio of incontinence, however, was high with both methods. This was considered an early follow-up result and all cases improved after the administration of anticholinergics.
The enucleation ratio, as calculated from the amount of removed tissue in the transition zone as found by TRUS, was 0.685 in HoLEP. This was almost similar to the ratio for TURP; however, HoLEP removed more tissue in group 3. Although the transition zone should have been entirely removed by HoLEP, the actual amount of tissue removed was less than expected. Kuntz et al. [10] have suggested that tissue loss due to vaporization and morcellation may account for the above result. There may be loss of tissue from the collecting tool used in morcellation as well.
The overall efficiency of HoLEP for the entire study population was 0.34 g/min (group 1, 0.12±0.07 g/min; group 2, 0.30±0.10 g/min; group 3, 0.56±0.21 g/min). This value is rather low compared with previous clinical trials [11]. In our study, the duration of surgery was not divided into resection time and morcellation time. Also, the time to control bleeding, preparation of tools, and urethral catheterization time were included in the operation time. However, the overall resection efficacy was better than with TURP. HoLEP also showed better resection efficacy in group 1, although it was not statistically different.
The present study had several limitations. First, the number of study patients was small. We tried but it was difficult to find appropriate methods for a retrospective study with a limited number of patients that was designed by matching on prostate size. Also, because the data were collected retrospectively, this study could have had a selection bias. However, the results of our study can still be meaningful because of the similar preoperative factors between the groups. Second, research is lacking on other factors associated with urination, such as change in pressure/flow (i.e., urodynamics). Investigating pressure/flow may be important when determining whether a patient with BPH should undergo an operation. Not all patients had a pressure/ flow test done at our hospital. In its place, uroflowmetry and IPSS were considered when an operation was being decided upon. Almost all cases showed improvement of voiding symptoms after surgery. The last limitation was the result of the short postsurgery follow-up in this study.
This study analyzed early postsurgery follow-up data only. HoLEP was done regardless of prostate size. Improvements in micturition and symptom scores were immediate. Mean IPSS, peak urinary flow rate, and postvoid residual urine volumes returned to normal within 1 month after the operation in each group. Although there was no long-term follow-up in this study, other studies have shown more improvement in voiding symptoms with HoLEP [12].
Figures and Tables
References
1. Madersbacher S, Marberger M. Is transurethral resection of the prostate still justified? BJU Int. 1999; 83:227–237.
2. Gilling PJ, Cass CB, Malcolm AR, Fraundorfer MR. Combination holmium and Nd:YAG laser ablation of the prostate: initial clinical experience. J Endourol. 1995; 9:151–153.
3. Shah HN, Sodha HS, Kharodawala SJ, Khandkar AA, Hegde SS, Bansal MB. Influence of prostate size on the outcome of holmium laser enucleation of the prostate. BJU Int. 2008; 101:1536–1541.
4. Gilling PJ, Kennett K, Das AK, Thompson D, Fraundorfer MR. Holmium laser enucleation of the prostate (HoLEP) combined with transurethral tissue morcellation: an update on the early clinical experience. J Endourol. 1998; 12:457–459.
5. Yin L, Teng J, Huang CJ, Zhang X, Xu D. Holmium laser enucleation of the prostate versus transurethral resection of the prostate: a systematic review and meta-analysis of randomized controlled trials. J Endourol. 2013; 27:604–611.
6. El-Hakim A, Elhilali MM. Holmium laser enucleation of the prostate can be taught: the first learning experience. BJU Int. 2002; 90:863–869.
7. Bae J, Oh SJ, Paick JS. The learning curve for holmium laser enucleation of the prostate: a single-center experience. Korean J Urol. 2010; 51:688–693.
8. Montorsi F, Naspro R, Salonia A, Suardi N, Briganti A, Zanoni M, et al. Holmium laser enucleation versus transurethral resection of the prostate: results from a 2-center, prospective, randomized trial in patients with obstructive benign prostatic hyperplasia. J Urol. 2004; 172(5 Pt 1):1926–1929.
9. Ahyai SA, Gilling P, Kaplan SA, Kuntz RM, Madersbacher S, Montorsi F, et al. Meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic enlargement. Eur Urol. 2010; 58:384–397.
10. Kuntz RM, Ahyai S, Lehrich K, Fayad A. Transurethral holmium laser enucleation of the prostate versus transurethral electrocautery resection of the prostate: a randomized prospective trial in 200 patients. J Urol. 2004; 172:1012–1016.
11. Ahyai SA, Chun FK, Lehrich K, Dahlem R, Zacharias MS, Fisch MM, et al. Transurethral holmium laser enucleation versus transurethral resection of the prostate and simple open prostatectomy--which procedure is faster? J Urol. 2012; 187:1608–1613.
12. Elmansy HM, Kotb A, Elhilali MM. Holmium laser enucleation of the prostate: long-term durability of clinical outcomes and complication rates during 10 years of followup. J Urol. 2011; 186:1972–1976.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download