Abstract
Purpose
Since the 1990s, it has been well known that orchiopexies should be performed by no later than 2 years of age. Nevertheless, studies from other countries report a substantial number of delayed orchiopexies. On the basis of an analysis of a tertiary care hospital database, we aimed to investigate the incidence of delayed orchiopexies performed in patients after 5 years of age and to understand the causes of such delays and the possible consequences.
Materials and Methods
We retrospectively analyzed the surgical database of Seoul National University Hospital between 2004 and 2012 and detected patients who underwent orchiopexy later than 5 years of age. Reasons for delayed orchiopexies were studied and the possible consequences of delayed orchiopexies were assessed with respect to surgical difficulty and testicular volume.
Results
We found 160 cases of delayed orchiopexies, which accounted for about 15% of all orchiopexies performed. Two major reasons for delay were related to the parents of the child: parental delay and parental request for the treatment of persistent retractile testis. Acquired cryptorchidism was found in 21 cases (13.1%), mainly associated with hypospadias. Surgical difficulty, especially owing to a short testicular cord, was encountered in 48 cases (30.2%), and a comparison with age-matched normative values showed substantially smaller testicular volume.
Conclusions
Despite well-established guidelines for the optimal age of surgery, 15% of orchiopexies were not performed at a proper time. Improved propagation of an optimal age limit is necessary to reduce the rate of delayed orchiopexies considering increases in surgical difficulty and potential testicular growth retardation.
Cryptorchidism is the most common genital anomaly identified in males at birth with a prevalence of about 1% at 1 year of age [1,2]. After the first year of life, spontaneous testicular descent is unlikely to occur, and it has been postulated that testicular position at that time might be final, or that in some cases, testicular ascent may occur [3]. Because cryptorchidism is associated with infertility, malignancy, and cosmetic concerns, orchiopexy has been proven necessary to prevent such conditions.
Although various guidelines may differ regarding the age at which an orchiopexy should be performed, it is agreed that it should be performed at least before 18 months of age [4-6]. These recommendations are based on medical and psychological postulations such as a higher risk of malignancy and infertility in the undescended testes (UDT) [4]. The Nordic consensus on the treatment of UDT advocates treatment at 6 to 12 months of age [5]. However, reports from several countries have indicated that these theoretical advantages or guidelines for early orchiopexy have not been applied in clinical practice [7-10]. Data from many surgical divisions in different countries show that orchiopexies are still being performed late in childhood despite several national and international recommendations. Iatrogenic trapping by previous surgery, parental delay, and delay in referral have been speculated, but the data are sparse and researchers could not elucidate possible causes.
Another interesting explanation for delayed orchiopexy is the presence of acquired cryptorchidism (AC). Although a testis can be found in the scrotum during a previous examination, it can ascend as the child grows older. According to Hack et al. [11], the prevalence of AC can reach 73.4% and the median age of orchiopexy can be postponed until 8.4 years of age. Thus, this could be another explanation for late orchiopexy, although its presence has not been verified in Korean published data.
Retractile testis (RT) is regarded as a normal variant of UDT and does not require orchiopexy, because the testis will descend spontaneously. However, the distinction between RT and AC is not clear, which may explain the wide range of prevalence of testicular ascent among patients who were followed up for RT [12-14]. Furthermore, the usefulness and feasibility of annual follow-up until puberty, when both AC and RT are likely to spontaneously descend, has not been established.
In tertiary care hospitals, children with serious medical conditions often miss the optimal surgical timing for orchiopexy. As a result of the more urgent need for treatment of coexisting medical conditions, which affect more vital organs, the presence of UDT is often forgotten. Only after the more serious illnesses have been treated does undergoing delayed orchiopexy finally become the main focus. This may be a plausible scenario, but relevant statistics supporting such a hypothesis have not yet been reported.
To provide additional information for our current database, we analyzed the data for delayed orchiopexies performed at our institution. Because there has been only one report in the setting of a tertiary referral hospital, our data may be valuable to classify and understand the possible reasons for delayed orchiopexies. Another objective of our study was to evaluate the effects of delayed orchiopexies. By use of our surgical data, we tried to study the potential effects of delayed orchiopexies on surgical difficulty and testicular volume. We assumed that a delay in surgery might be associated with shortness of cord length, leading to difficulty in surgery. Moreover, it could result in retarded testicular growth compared with the mean normative value of age-matched Korean boys [15].
We retrospectively analyzed the records of all orchiopexies for UDT performed in patients older than 5 years from January 2004 through June 2012. We reviewed medical records and analyzed data concerning the age at operation, reasons for delayed surgery, laterality, testis size measured during operation, and difficulty in cord lengthening.
The reasons for delayed surgery were as follows: (1) AC, (2) parental request for the treatment of persistent RT, (3) delay due to coexisting medical conditions (missed the surgical timing owing to treating other medical conditions), (4) reoperative orchiopexy (iatrogenic trapping following previous orchiopexies or herniorrhaphies), (5) parental delay (parents did not do anything despite the presence of overt cryptorchidism), and (6) delayed referral by the primary physician.
We defined AC when there had been a previous medical record confirming scrotal location of the testis. Parental delay included unintentional late detection (recent parental recognition of an empty scrotum without prior knowledge of the testicular position) and intentional negligence (parents knew that their son's testis was elevated but did not seek medical consultation).
Orchiopexy was performed by using the conventional technique of placing the testis in the subdartos space. Difficulty in lengthening was defined when the testis did not reach the midscrotum following the release of the processus vaginalis and cremasteric muscle during orchiopexy.
The effect of delayed orchiopexies was assessed by comparing the size of the operated testes with those of age-matched Korean boys [15]. Data were entered and expressed by using PASW ver. 18.0 (SPSS Inc., Chicago, IL, USA). The chi-square test was used to examine the differences in proportion. A p-value lower than 0.05 was considered significant.
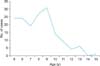
We analyzed data from 963 patients from our database who underwent 1,084 orchiopexies during the period of this study. A total of 125 patients (12.9%) underwent 160 (14.6%) delayed orchiopexies (81 right, 79 left-sided). Their median age at operation was 8.0 years (range, 5-15 years). The incidence of orchiopexies increased from the age of 5, peaked between 8 and 9 years of age, and then abruptly decreased after 10 years of age (Fig. 1).
The reasons for delayed orchiopexies in this population are described in Table 1. Parental delay and parental request for the treatment of persistent RT accounted for more than half of cases. Of the 54 cases of parental delay, 28 and 26 cases were attributed to unintentional late detection and intentional negligence despite prior recommendation by primary physician, respectively. AC was found in 21 cases (13.1%). Of these cases, 16 (76%) had comorbidities including hypospadias (11 patients), Prader-Willy syndrome (2 patients), and cerebral palsy (2 patients).
During operation, difficulty in cord lengthening was noted in 48 cases (30.2%, Table 2). Except for RT, for which only 1 case showed difficulty, the difficulty was nonspecifically distributed to each reason (p>0.05).
Data for testicular volume measurement were available in 116 cases. Fig. 2 shows the mean testicular volume in accordance with age. Compared with the mean Korean normative data, which are depicted for reference, significantly lower mean testicular volume was observed and the difference became larger with increasing age.
In this study, we reviewed our hospital's database to detect factors that can contribute to delayed orchiopexies. Such delays have been reported elsewhere, but the causes have not been well clarified, especially in a tertiary care setting. Because delays in orchiopexies can lead to testicular growth retardation, can be detrimental to future fertility, and may increase the risk of testicular cancer development, it is necessary to know why orchiopexies were not performed at a proper time. Understanding such causes could be helpful when implementing proper strategies to solve this problem.
We discovered that 160 orchiopexies were performed in a delayed fashion during the 8.5-year study period. This is not a small number, considering that orchiopexies account for about 15% of the surgeries performed in Seoul National University Hospital. An even larger number of delayed orchiopexies was reported in other studies. McCabe and Kenny [8] evaluated hospital statistics of all orchiopexies performed in England over a 9-year period and reported that only 20% of boys are operated on before the age of 24 months. Guven and Kogan [16] conducted a study similar to ours in a tertiary care center setting and reported that 33% were delayed surgeries between 1997 and 2006, although their age limit was lowered to 4 years. The above-mentioned studies indicate that, regarding the age limit of surgery, current guidelines for orchiopexy have not been well observed, even in tertiary care centers.
Considering that most textbooks or guidelines published after the 1980s recommend orchiopexy to be performed no later than 2 years of age, it is surprising that so many orchiopexies were conducted after 5 years. Reports from other countries have speculated that a possible reason may be delayed referral from primary physicians, differences in referral habits between pediatricians and primary physicians, cultural differences, parental delay, reoperative orchiopexy owing to iatrogenic trapping of testis, and the presence of AC [7-14]. Our data add new reasons to the current database, such as delay due to other medical conditions and parental request for persistent RT. These new reasons may be due to differences in the study setting or may reflect cultural differences, i.e., a study in a tertiary care hospital setting in Korea. These additional reasons could broaden our knowledge and aid us in understanding and solving the problem of delayed orchiopexy.
Considering the preventable nature of complications related to cryptorchidism, it is frustrating that parental delay and delayed referral (by primary physician) contributes to more than 40% of delayed orchiopexies. Regarding parental delay, a similar proportion of unintentional or intentional delay was identified. Owing to the retrospective nature of this study, we could not identify the exact cause of these delays. However, we expect that improved education or propagation concerning the consequences of untreated cryptorchidism to parents will reduce the incidence of delayed surgery. Despite the fact that more than 20 years have passed since the controversy concerning the optimal age for orchiopexy was settled, our data showed that unexplained delayed referral by a physician was still responsible for delayed orchiopexies in about 8% of patients. This may be related to failure to determine the correct testicular position or misunderstanding of the optimal age for orchiopexy or the occurrence of AC. This portrays the clear need for primary physicians to be familiar with testicular palpation and to know the optimal age for orchiopexy.
Intriguingly, parental request to correct RT accounted for more than 20% of cases. Despite the fact that all RT will spontaneously descend, the distinction between RT and AC remains unclear. This explains the wide ranges in testicular ascent reported in those who were presumed to have RT [13,17]. In addition, the need to follow-up until puberty may instigate an impatient parent to consent to have an orchiopexy performed, because the duration of surveillance into puberty may seem too long for the parents to regularly evaluate the normal testicular position of their son.
AC, which is also referred to as ascending testis, is also a significant reason for delayed orchiopexy. This ascent was first noted in 1966 and data regarding similar cases were accumulated in subsequent studies. The risk of ascent was reported to increase in the presence of RT, cerebral palsy, and proximal hypospadias [18,19]. As far as we know, our data on AC are the first such report in Korea. Our data showed that AC significantly contributed to delayed orchiopexy, although the proportion was not as large as that reported in an American tertiary care center study [16]. Moreover, as previous reports have indicated, about half of AC patients in our study had a history of hypospadias.
Considering the fact that hypospadias is the result of low androgenic action and that androgen plays a critical role for proper signaling of the genitofemoral nerve via calcitonin gene related peptide (CGRP) and subsequent testicular ascent in animal study [20,21], it may be assumed that a low androgenic milieu could lead to disruption of innervations of CGRP-positive nerves and possibly testicular ascent afterwards. In Prader-Willy syndrome, a similarly low androgenic milieu may play a role. In the case of cerebral palsy, cremasteric muscle spasticity may be implicated. These results suggest that careful testicular palpation should be included in follow-up tests for patients who have a history of operation for proximal hypospadias, Prader-Willy syndrome, or cerebral palsy.
The most critical point of orchiopexy is cord lengthening by division of the processus vaginalis and dissection of the cremasteric muscle and fascia. We observed a rate of difficulty of approximately 30% in cord lengthening in delayed cases of orchiopexy. This is unusually high compared with the 3%-5% range of incidence of difficulty in lengthening in younger children [22,23]. Although difficult cord lengthening could be expected in iatrogenic cases, it is interesting that a similarly high rate of difficulty was noted in all other causes of delay but the cases of RT. As Hack et al. [24] assumed, failure of the spermatic cord to elongate in proportion to increasing body length may play a role in the case of delayed orchiopexy and this may be responsible for the difficulty in cord lengthening in some patients regardless of the reason.
The deleterious effect of delayed orchiopexy may be reflected in the comparison of testicular size. The mean testicular size of patients who underwent delayed orchiopexy was substantially lower than that of the age-matched normative patients. Moreover, the fact that such discrepancy was found in all age ranges supports the harmful effect of delayed orchiopexy. These findings underscore the proper timing of orchiopexy. Whether this effect can be applied to all causes could not be evaluated owing to the small number of cases for each reason.
This study had some limitations. Because it was performed in a retrospective manner, the determination of causes may not be discriminative and is liable to response bias. For example, what we described to be a case of delayed referral may actually have been a case of a parent trying to hide his or her mistake of postponement of surgery, despite appropriate referral. Additionally, the low incidence of AC may result from the fact that some cases might have been spuriously categorized as parental delay or delayed referral. The physical examination performed by parents and primary physicians was not as accurate as that performed by pediatric urologists, thus resulting in incorrect assessment for testicular positions. Furthermore, the age-matched normative volume of testis was measured by Prader orchidometry, whereas testicular volume in our study was measured directly by use of a ruler during the operation. This difference in measuring testicular volume may have affected the difference in testicular size.
A substantial number of patients with cryptorchidism missed the proper timing for orchiopexy and underwent delayed surgery. Several reasons were attributed to this delay, which underscore the necessity of improved propagation of the optimal age for orchiopexy. Similar to previous reports in other countries, AC played a significant role in the Korean cohort. The increased number of AC in cases of hypospadias suggests the need for vigilant follow-up, even after the completion of urethroplasty. The harmful effects of delayed orchiopexy were reflected in difficult cord lengthening and retarded testicular growth.
Figures and Tables
References
1. Berkowitz GS, Lapinski RH, Dolgin SE, Gazella JG, Bodian CA, Holzman IR. Prevalence and natural history of cryptorchidism. Pediatrics. 1993; 92:44–49.
2. Thong M, Lim C, Fatimah H. Undescended testes: incidence in 1,002 consecutive male infants and outcome at 1 year of age. Pediatr Surg Int. 1998; 13:37–41.
3. Barthold JS, Gonzalez R. The epidemiology of congenital cryptorchidism, testicular ascent and orchiopexy. J Urol. 2003; 170(6 Pt 1):2396–2401.
4. American Academy of Pediatrics. Timing of elective surgery on the genitalia of male children with particular reference to the risks, benefits, and psychological effects of surgery and anesthesia. Pediatrics. 1996; 97:590–594.
5. Ritzen EM, Bergh A, Bjerknes R, Christiansen P, Cortes D, Haugen SE, et al. Nordic consensus on treatment of undescended testes. Acta Paediatr. 2007; 96:638–643.
6. Tekgul S, Riedmiller H, Gerharz E, Hoebeke P, Kocvara R, Nijman R, et al. Guidelines on pediatric urology. Arnhem: European Society for Pediatric Urology;2009.
7. Springer A, Huber C, Reck CA, Fengler D, Horcher E. Delayed referral despite appropriate knowledge in cryptorchidism as a cause of delayed orchidopexies in Austria. Klin Padiatr. 2010; 222:248–251.
8. McCabe JE, Kenny SE. Orchidopexy for undescended testis in England: is it evidence based? J Pediatr Surg. 2008; 43:353–357.
9. Golabek T, Kiely E. Patterns of referral and treatment of undescended testis: a 12-year experience in a single centre. Ir J Med Sci. 2010; 179:511–514.
10. Kokorowski PJ, Routh JC, Graham DA, Nelson CP. Variations in timing of surgery among boys who underwent orchidopexy for cryptorchidism. Pediatrics. 2010; 126:e576–e582.
11. Hack WW, Meijer RW, van der Voort-Doedens LM, Bos SD, Haasnoot K. Natural course of acquired undescended testis in boys. Br J Surg. 2003; 90:728–731.
12. Atwell JD. Ascent of the testis: fact or fiction. Br J Urol. 1985; 57:474–477.
13. Stec AA, Thomas JC, DeMarco RT, Pope JC 4th, Brock JW 3rd, Adams MC. Incidence of testicular ascent in boys with retractile testes. J Urol. 2007; 178(4 Pt 2):1722–1724.
14. Hack WW, Meijer RW, Van Der Voort-Doedens LM, Bos SD, De Kok ME. Previous testicular position in boys referred for an undescended testis: further explanation of the late orchidopexy enigma? BJU Int. 2003; 92:293–296.
15. Song JE, Yi YY, Hwang IT, Lee HR, Lim JS, Yang S. Testicular volume in Korean boys. J Korean Soc Pediatr Endocrinol. 2010; 15:14–18.
16. Guven A, Kogan BA. Undescended testis in older boys: further evidence that ascending testes are common. J Pediatr Surg. 2008; 43:1700–1704.
17. Agarwal PK, Diaz M, Elder JS. Retractile testis: is it really a normal variant? J Urol. 2006; 175:1496–1499.
18. Tasian GE, Zaid H, Cabana MD, Baskin LS. Proximal hypospadias and risk of acquired cryptorchidism. J Urol. 2010; 184:715–720.
19. Itesako T, Nara K, Matsui F, Matsumoto F, Shimada K. Acquired undescended testes in boys with hypospadias. J Urol. 2011; 185:6 Suppl. 2440–2443.
20. Shono T, Zakaria O, Imajima T, Suita S. Does proximal genitofemoral nerve division induce testicular maldescent or ascent in the rat? BJU Int. 1999; 83:323–326.
21. Nazir Z, Masood R, Rehman R. Sensory innervation of normal and hypospadiac prepuce: possible implications in hypospadiology. Pediatr Surg Int. 2004; 20:623–627.
22. Kirsch AJ, Escala J, Duckett JW, Smith GH, Zderic SA, Canning DA, et al. Surgical management of the nonpalpable testis: the Children's Hospital of Philadelphia experience. J Urol. 1998; 159:1340–1343.
23. Banieghbal B, Davies M. Laparoscopic evaluation of testicular mobility as a guide to management of intra-abdominal testes. World J Urol. 2003; 20:343–345.
24. Hack WW, Goede J, van der Voort-Doedens LM, Meijer RW. Acquired undescended testis: putting the pieces together. Int J Androl. 2012; 35:41–45.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download