Abstract
A 61-year-old man presented with a right renal mass with a vena caval thrombus on computed tomography that was consistent with renal cell carcinoma. The results of routine laboratory examinations and urinalysis were within normal limits. Preoperative planning was critical owing to the presence of the vena caval thrombus. A radical nephrectomy, vena caval thrombectomy, and regional lymphadenectomy were done. The pathologic report was consistent with a high-grade, invasive urothelial carcinoma, with sarcomatoid differentiation involving the renal vein and inferior vena cava (Stage IV, T4N0M0). Thus, this was a rare case of upper tract urothelial carcinoma. Adjuvant chemotherapy with the methotrexate, vinblastine, doxorubicin, cisplatinum regimen is scheduled. To our knowledge, this is the first report in Korea of upper tract urothelial carcinoma of the sarcomatoid type with a vena caval thrombus.
Renal masses are now most frequently diagnosed incidentally. Epithelial tumors of the kidney account for approximately 3% of all solid neoplasms, with adenocarcinoma or renal cell carcinoma (RCC) representing almost 85% [1]. RCC with a caval tumor thrombus occurs in 4% to 10% of patients and can present a formidable surgical challenge [2]. Herein, we report a rare case of upper tract urothelial carcinoma with a rare inferior vena cava (IVC) thrombus that mimicked RCC. Upper tract urothelial carcinoma and RCC are two different types of malignancy that are distinguished on the basis of tissue type and location. Differentiation of these malignancies is challenging but necessary because the management strategies and standard of treatment differs. To the best of our knowledge, our case is the first reported upper tract urothelial carcinoma of the sarcomatoid type with an IVC thrombus in Korea.
A 61-year-old man who had been diagnosed with hypertension and diabetes 15 years previously was referred to our outpatient clinic for an incidental finding on ultrasonography of a right renal mass. He had the nonspecific symptom of fatigue since 12 weeks previously. No palpable mass was detected on the physical examination. The results of routine laboratory examinations and urinalysis were within normal limits. A computed tomography (CT) scan revealed a 10-cm right renal mass with areas of necrosis and suspicious perirenal fat infiltration and invasion to the right adrenal gland. Some lymph nodes were enlarged in the aortocaval area. The tumor also infiltrated the right renal vein and the IVC as a typical advanced RCC (Fig. 1). A diagnosis of RCC with IVC thrombus (cT3bN1M0) was made and a radical nephrectomy with vena caval thrombectomy was planned.
Under general anesthesia, the patient was placed in the supine position with the right side elevated by 15 degrees. A midline abdominal incision was made and a Kocher maneuver was done to expose the right kidney. The liver was retracted to expose the right renal vein and IVC. The right kidney was mobilized and a venous cannulation was performed above and below the IVC mass, and arterial cannulation was performed on the left femoral artery. The incision on the IVC was made where the renal vein was ligated after cardiopulmonary bypass. Vena caval thrombectomy was done and reconstruction was accomplished by use of nonabsorbable sutures. En bloc resection of the right renal mass and regional lymphadenectomy were performed successfully. The pathological diagnosis was invasive urothelial carcinoma, of a high grade, with sarcomatoid differentiation, which invaded the renal cortex but was limited to the capsule (Figs. 2, 3). The IVC thrombus was composed of urothelial carcinoma of a high grade; the lymph nodes were free of carcinoma (pT4N0M0). The patient was discharged on the fourth postoperative day, and adjuvant chemotherapy with the methotrexate, vinblastine, doxorubicin, and cisplatinum regimen is scheduled.
Cases of upper tract urothelial carcinoma with extension to the vena cava are rare. A case of a renal pelvic carcinoma of the transitional histotype with vena caval invasion was reported previously with a focus on the challenges of IVC resection and replacement with a human cadaveric graft [3]. Upper tract urothelial carcinoma, including tumors of the ureter and renal pelvis, is an uncommon genitourinary malignancy that accounts for 5% of urothelial cancers and less than 10% of renal tumors. Owing to the infrequent presentation of this carcinoma, trends in disease incidence, associated demographic factors, and predictors of cancer-related and overall survival outcomes are limited [3]. Urothelial carcinomas of the renal pelvis also more often appear to be of a higher stage than their urinary bladder counterparts [4]. Invasion of the renal vein in the renal hilum or the IVC is considered to be a rare event and an uncommon late finding in urothelial carcinoma of the pelvocaliceal system [5]. Vena caval involvement by intraluminal extension of the tumor mass has been reported to occur in 4% to 10% of patients with renal neoplasm [6]. In a previous report on upper tract urothelial carcinoma with vena caval thrombi, of 18 cases, 6 cases underwent nephroureterectomy with vena caval reconstruction; 4 had nephroureterectomy with thrombectomy; 2 had nephrectomy and thrombectomy with chemotherapy; 3 had nephroureterectomy and thrombectomy; 1 had nephroureterectomy, thrombectomy, and radiation; 1 had nephroureterectomy, thrombectomy, and chemotherapy; and 1 underwent biopsy only [7]. Postoperative follow-up was done in 14 patients. Eight died of the disease within 6 months of surgery. In another review of cases done in 2005, 13 reported cases of renal pelvic sarcomatoid carcinoma had been documented since 1961, and all patients presented with metastatic disease or advanced renal parenchymal involvement, with a mean survival time of less than 9 months [8]. A normally thin renal pelvic musculature supports the extension of the tumor to contiguous structures like the renal parenchyma. As in this case, a shorter right renal vein compared with the left may have promoted intraluminal tumor extension to the IVC. Large infiltrative urothelial carcinoma with both pelvic and parenchymal involvement may simulate other entities such as lymphoma, metastasis, xanthogranulomatous pyelonephritis, or RCC with invasion to the renal pelvis [5]. Intrarenal urothelial carcinoma is a close radiologic mimic of other infiltrative renal masses, especially centrally located RCC [9]. Despite no effective treatments having previously been reported, systemic chemotherapy with a platinum-based regimen may be recommended for a renal pelvic tumor owing to its urothelial origin. In our case, the preoperative CT finding was typical RCC with an IVC thrombus showing a vena caval infiltration pattern. From this finding, a standard radical nephrectomy with thrombectomy and regional lymphadenectomy were performed. The prognosis of patients with a urothelial carcinoma accompanied by an IVC thrombus is poor compared with that of patients with RCC with a vena caval tumor thrombus [10]. Also, up to now, a radical procedure with thrombectomy for urothelial carcinoma with an IVC thrombus has been controversial.
In conclusion, establishment of the correct diagnosis of an upper tract urothelial carcinoma with a tumor thrombus in the vena cava is important for accurate surgical planning [7]. Thus, if a urothelial carcinoma with thrombus dissimilar from our case is suspected, examination of a frozen section may provide a correct diagnosis. If the results reveal a urothelial carcinoma, a standard nephroureterectomy with cavotomy and thrombectomy and bladder cuff excision should be performed.
The fact that the incidence of urothelial carcinoma is low, and that urothelial carcinoma is diagnosed at a later stage when metastasis has ensued, contributes to limited documentation of disease behavior and response to different treatment modalities. Cystoscopy and ureterectomy were considered for this case. However, because of the aggressive nature of the disease and its metastatic potential, adjuvant chemotherapy was considered to be a better option. A second-look cystoscopy was performed months after the surgery, before adjuvant chemotherapy, to search for small tumors in the bladder. The vascular pattern of the bladder mucosa and the anatomic landmarks such as the trigone and both ureteral orifices were unremarkable.
Figures and Tables
FIG. 1
Computed tomography revealed an approximately 10-cm-sized renal mass with partial necrosis (A) and invasion to the right renal vein and inferior vena cava (B).
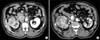
FIG. 2
Bisected kidney revealed an ill-defined, infiltrative, whitish soft mass (9.5 cm×7 cm), mainly involving the renal pelvis (A). The ureter was dilated owing to extension of the tumor (B).

FIG. 3
Urothelial carcinoma, of a high grade, invaded the renal cortex limited to the capsule (A: H&E, ×100; B: H&E, ×400). Area of urothelial carcinoma with sarcomatoid differentiation showing spindled tumor cells (C: H&E, ×100; D: H&E, ×400). Separately sent thrombus sample contained a tumor emboli (E: H&E, ×100). High-power view of the tumor emboli showed high-grade urothelial carcinoma (F: H&E, ×400).

ACKNOWLEDGMENTS
This study was supported by a grant from the Korea Healthcare technology R&D Project, Ministry for Health, Welfare & Family Affairs, Republic of Korea (A084120).
References
1. Uzzo RG, Cherullo E, Myles J, Novick AC. Renal cell carcinoma invading the urinary collecting system: implications for staging. J Urol. 2002; 167:2392–2396.
2. Hyams ES, Pierorazio PM, Shah A, Lum YW, Black J, Allaf ME. Graft reconstruction of inferior vena cava for renal cell carcinoma stage pT3b or greater. Urology. 2011; 78:838–843.
3. Nam JK, Moon KM, Park SW, Chung MK. Surgical treatment of inferior vena cava invasion in patients with renal pelvis transitional cell carcinoma by use of human cadaveric aorta. Korean J Urol. 2012; 53:285–287.
4. Raman JD, Messer J, Sielatycki JA, Hollenbeak CS. Incidence and survival of patients with carcinoma of the ureter and renal pelvis in the USA, 1973-2005. BJU Int. 2011; 107:1059–1064.
5. Perez-Montiel D, Wakely PE, Hes O, Michal M, Suster S. High-grade urothelial carcinoma of the renal pelvis: clinicopathologic study of 108 cases with emphasis on unusual morphologic variants. Mod Pathol. 2006; 19:494–503.
6. Prando A, Prando P, Prando D. Urothelial cancer of the renal pelvicaliceal system: unusual imaging manifestations. Radiographics. 2010; 30:1553–1566.
7. Kaplan S, Ekici S, Dogan R, Demircin M, Ozen H, Pasaoglu I. Surgical management of renal cell carcinoma with inferior vena cava tumor thrombus. Am J Surg. 2002; 183:292–299.
8. Miyazato M, Yonou H, Sugaya K, Koyama Y, Hatano T, Ogawa Y. Transitional cell carcinoma of the renal pelvis forming tumor thrombus in the vena cava. Int J Urol. 2001; 8:575–577.
9. Thiel DD, Igel TC, Wu KJ. Sarcomatoid carcinoma of transitional cell origin confined to renal pelvis. Urology. 2006; 67:622.e9–622.e11.
10. Tseng YS, Chen KH, Chiu B, Chen Y, Chung SD. Renal urothelial carcinoma with extended venous thrombus. South Med J. 2010; 103:813–814.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download