Abstract
Purpose
To evaluate the efficacy of subureteral injection types in patients with middle- to high-grade vesicoureteral reflux (VUR).
Materials and Methods
Between June 1999 and September 2010, subureteral dextranomer was applied at our clinic to 149 patients (214 refluxing ureters) with grades II, III, and IV VUR. Group 1 consisted of 54 patients (80 ureters), and group 2 consisted of 95 patients (134 ureters). The standard subureteric transurethral injection (STING) procedure was applied to group 1, and the modified STING procedure was applied to group 2. A second and if needed a third injection was applied to unsuccessfully treated patients. The mean follow-up period was 2 years. Patients were evaluated by cystography and ultrasonography in the third month of follow-up.
Results
VUR was resolved completely after a single injection in 54/80 ureters (67.5%) in group 1 and in 94/134 ureters (70.1%) in group 2. Overall successes after a second or a third injection were 61/80 (76.2%) and 111/134 (82.8%), respectively. There was a statistically significant difference between the groups only for grade IV reflux following multiple injections (p<0.05).
Correction of vesicoureteral reflux (VUR) with endoscopic injections was first described by Matouschek [1] and has been widely accepted since the pioneering work of O'Donnell and Puri [2]. This treatment has become the preferred therapy at selected centers because it is simple, generally obviates the need for long-term antibiotic prophylaxis, and often eliminates open surgery in selected children, especially in cases of intermediate and high-grade VUR [3]. Success rates of endoscopic therapy may be affected by factors such as anatomic variations, dysfunctional voiding, nephropathy, and ureteral dilatation grade as well as by appropriate application of the surgery technique [4,5,6,7]. In the endoscopic correction of VUR, polytetrafluoroethylene and then bovine collagen and Macroplastique bulking agents have been used as injection materials but have been replaced by dextranomer hyaluronic acid (DxHa) because of complications with their use.
New modifications of the subureteric transurethral injection (STING) method have been made to increase the success rate of this method [8]. The modified STING procedure (hydrodistention technique, HIT) applied by Kirsch et al. [9] is one of the most widely accepted and frequently used modifications of the STING method. In the present study, we aimed to compare our results with the endoscopic treatment of reflux by use of the standard STING and HIT. We began to use HIT at our hospital to increase success rates in the treatment of VUR in children.
Between June 1999 and September 2010, 149 patients with 214 refluxing ureters of grades II, III, and IV were treated endoscopically at our hospital. We conducted the study retrospectively including those patients. Ethics Committee approval was obtained from our hospital's Ethics Committee. We considered grades II and III reflux as middle-grade reflux and grade IV as high-grade reflux. We used a standard technique with other injection materials from 1994 until 1999, the results of which were excluded from this study. In the present study, we included the cases since 1999 for which we used DxHa as an injection material. We used the standard STING procedure described by O'Donnell and Puri [2] between 1999 and 2005 and have been using Kirsch's HIT since 2005. The results of both techniques were evaluated retrospectively in two groups. Group 1 included the patients who underwent the standard STING procedure, and group 2 included the patients who were treated with the HIT.
VUR was determined in the patients included in the study by use of voiding cystourethrogram (VCUG). VUR was graded according to the International Reflux Study Group classification. Renal scarring was evaluated with renal ultrasonography and dimercaptosuccinic acid scan preoperatively. Surgical indications were febrile urinary infection despite antibiotic prophylaxis, recurrent pyelonephritis, renal scar development, high-grade reflux, and persistent reflux despite antibiotic therapy.
We included in our study patients with grades II, III, and IV reflux. Grade I patients were not included because of the possibility of spontaneous resolution, and grade V patients were excluded because of the probability of significant changes in anatomic structure. Also, the patients who had undergone previous endoscopic injection with different injection materials, had undergone previous surgery for VUR, had neurogenic bladder, or had anatomic abnormalities such as complete duplication were excluded. The evaluation was made only for the reflux grade and the results of the technique. Predictive factors affecting success, such as age, localization, and type of orifice, were not evaluated in this study. We did not include the patients admitted to our clinic after 2010 because of the insufficient follow-up period.
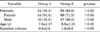
There were 44 girls and 10 boys (80 ureters) in group 1, and 68 girls and 27 boys (134 ureters) in group 2. Distribution of the reflux grades was 13, 49, and 18 ureters for grades II, III, and IV in group 1, and 16, 69, and 49 ureters for grades II, III, and IV in group 2, respectively. The mean patient age was 7.62 years (range, 18-144 months) in group 1 and 6 years (range, 2 months to 18 years) in group 2. Mean follow-up was 24 months (range, 18-36 months).
DxHa injection was applied to all patients. The mean injection material used was 0.9 mL (range, 0.5-2 mL) in group 1 and 1 mL (range, 0.5-1.6 mL) in group 2. Operations were performed by three surgeons with 10 to 20 years of experience in VUR (open or STING surgery). DxHa started to be used as the only implant material at our clinic in 2001.
The techniques used for the correction of VUR were the standard STING technique (between 1999 and 2005) and the modified STING technique (since 2005). In both techniques, endoscopic injection was performed with the patient under general anesthesia in the dorsal lithotomy position. Before the injection, prophylactic antibiotics were given. Only patients with sterile urine were injected. We used a 9.5-Fr pediatric cystoscope (Karl Storz, Tuttlingen,. Germany) and a 3.7-Fr needle. The standard technique was applied, as Puri and O'Donnell described, by injecting the material to the terminal submucosal ureter by introducing the needle from approximately 0.5 cm below the refluxing orifice at the 6 o'clock position. In the modified STING procedure, as Kirsch described, a pressured stream of irrigation fluid was directed into the refluxing ureter so that the ureter injection site could be defined. Then, the needle was introduced approximately 4 mm into the orifice at the 6 o'clock position. In both techniques, the procedure ended with the determination that the ureteral submucosa was raised up, a volcano-like mound was seen, and coaptation was sufficient.
Ultrasonography was performed in the first week after the operation to rule out any obstruction or progressive deterioration. A cystourethrogram was performed in the third month after the injection to evaluate the possibility of reflux recurrence. Patients with grade I reflux and higher were considered as partial or nonresponders. Among these patients, those with grade I reflux were taken to follow-up and patients with grade II reflux and higher were offered a second or third injection. Reinjection was performed in the same manner as for the previous injection. The patients not cured following injections were offered ureteral reimplantation. The patients with no reflux were followed up at 6, 12, and 24 months by VCUG. The first- and second-year follow-up results of the patients were also evaluated.
SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA) was used for the analysis. Categorical variables were compared by the chi-square test, and Student t-test was used for injected volume and age. Continuous variables were compared by using Student t-test. Statistical significance was considered at p≤0.05.
A total of 80 ureters for group 1 and 134 for group 2 were treated for VUR. Analysis of the patient's demographic information and volumes of injection material applied did not reveal a significant difference between the groups (Table 1). There was no statistically significant difference between the groups in terms of demographic information or reflux grade.
In the first injection, 54 ureters in group 1 and 94 in group 2 were treated. In group 1, reflux was cured after the first injection in all of the ureters with grade II reflux (13/13, 100%), in 32/49 ureters with grade III reflux (65.3%), and 9/18 ureters with grade IV reflux (50%). In group 2, reflux was cured after the first injection in all of the ureters with grade II reflux (16/16, 100%), in 51/69 ureters with grade III reflux (73.9%), and in 27/49 ureters with grade IV reflux (55.1%). There was no statistically significant difference in the success rates between the two groups for the first injection (not shown). Evaluation was performed on the basis of the three injection results through the overall success rate (Table 2).
A second injection was applied to 26 patients in group 1 and 40 patients in group 2 who were considered as nonresponders and partial responders following the first injection. After the second injection, a third injection was applied to 21 uncured patients in group 1 and to 30 uncured patients in group 2. Ultimately, treatment was considered unsuccessful in 19 patients in group 1 and in 23 patients in group 2. The overall success rates increased to 36/49 (73.4%) and 12/18 (66.6%) for grades III and IV, respectively, in group 1, and to 58/69 (84.5%) and 37/49 (75.5%) for grades III and IV, respectively in group 2 (Table 2).
In the evaluation of the overall success neglecting the grades, no significant difference was found in the first- and second-year results between groups 1 and 2. In terms of successes by grades, in grade II reflux, no statistically significant difference was observed between the successes of the two groups. The modified STING method seemed to be more successful in ureters with grade III reflux, although this difference was not statistically significant. There was a statistically significant difference between the two groups in grade IV refluxed ureters (Table 3). Because the number of patients was small, however, this difference did not affect the overall success, and no statistically significant difference was observed between the groups in terms of overall success rates.
At the end of the first year, 13 cases of downgraded reflux and 8 cases of persistent reflux were observed in group 1, and 17 cases of downgraded reflux and 9 of persistent reflux were observed in group 2. In the second year of follow-up, 2 patients in group 1 and 3 patients in group 2 were recovered.
The overall cure rate after the second and third injections increased to 76.2% in group 1 and to 82.8% in group 2 (Table 3). In group 1, 11 refluxing units were downgraded to grade I (13.7%) and these patients were moved to follow-up. Eight patients in group 1 were directed to open surgery (10%) (Cohen ureteroneocystostomy). From the 23 patients in group 2, 14 were downgraded to grade I reflux (10.4%) and were moved to follow-up, and 9 persistent refluxing ureters were reimplanted (Cohen ureteroneocystostomy) (6.7%). Downgraded cases were moved to follow-up.
In the postoperative period, temporary dilatation developed in 4 patients in group 1 and in 7 patients in group 2. This temporary dilatation disappeared in the first week of weekly follow-ups. Contralateral grade I reflux was observed in 2 of the patients but resolved spontaneously during the follow-up period. Infection developed in 8 patients and their duration of hospitalization was extended for 5 more days, and 3 patients had transient hematuria resolving spontaneously. Flank pain developed in 7 patients, which was relieved by analgesics.
The management of VUR in children is controversial. The traditional therapy of VUR is either long-term antibiotic therapy or surgery. Since the first endoscopic injection with Polytef by Matouschek [1] in 1981, endoscopic therapy has been used as an alternative to open surgery.
Different methods have been tried to increase the success rates of endoscopic treatment of VUR. One of the techniques described to increase success rates is the HIT, which was defined by Kirsch et al. [9] in 2004 and which we discuss in this study. Kirsch et al. [9] reported an increase in the success rate in patients with reflux from 79% to 89% by use of the HIT. The caudal migration of the injected material in the standard STING procedure might result in inefficiency. This migration will occur along the tunnel with the modified STING procedure and will contribute to ureteral stabilization.
In the studies by Cerwinka et al. [10], Sung and Skoog [11], and Capozza and Caione [12], different operative techniques were described in which a better ureteral coaptation was reported, and the success rates were around 90%. Although there are differences in the success rates of different techniques and also new materials and methods that have contributed to success, it should be kept in mind that the experience of the surgeon also has a direct effect on the treatment of VUR [13]. The success rates could also increase with small combinations of different technical nuances such as gauge, volume of the injected material, and determination of best needle placement, which depend on the experience of the surgeon [14].
Use of the HIT after multiple injections contributed to the treatment of our patients (overall success, 76.2% to 82.8%), but the results were not statistically significant except for the patients with grade IV reflux. As in several other studies, we obtained the highest rates of success in lower grade reflux. The 100% success rate we obtained in grade II reflux gradually decreased in grades III and IV reflux. The differences observed in the overall success rates between groups 1 and 2 were not statistically significant. On the other hand, although the difference observed between the groups in grade III reflux was not statistically significant, there was a trend toward significance for the modified STING technique in group 2. This trend needs to be confirmed by studies in a larger series. We think that the statistical difference found to be significant between the groups in grade IV was because of the better ureteral stabilization with the HIT as mentioned in previous studies [9]. The trend towards success mentioned here is encouraging for future studies.
In the studies of Gupta and Snodgrass [15] and Routh and Reinberg [16] where two different injection techniques were compared, no significant statistical difference was found between the techniques. Routh et al. [13] stated that the success obtained in favor of the HIT did not produce a statistical difference, whereas there was a statistically significant difference between the experience of the surgeon and VUR grade. Our study differs from those studies because of the higher success rates obtained by use of the HIT in grade IV reflux following multiple injections.
By applying the HIT used by Kirsch et al. [9], our success rate increased from 76.2% to 82.8%. Our HIT results seem to be lower than the results reported in the study where Kirsch first described the technique. This could be explained by the greater number of patients with grades III and IV refluxed ureters in our group (118/134, 88.1%). As Routh and Reinberg [16] pointed out, lower rates of success are an expected result in higher grade reflux. For example, whereas the success rate was 81% in grade I reflux, it was only 62% in grade V reflux [17]. Lavelle et al. [18] reported similar results. They treated their patients who had grade I to IV VUR with the HIT and determined the overall success rates to be 81.8%, 83.8%, 77.7%, and 72.7% for grades I to IV, respectively. Thus, they also had lower success rates in higher grades. Our HIT results for grades III and IV were consistent with those of Lavelle et al. [18]. We believe that with more experience in the HIT and with a larger patient population, our success rates will increase.
The aim of the STING procedure has been to increase the success rate with a single injection. Application of second and third injections increases the success rates. However, every additional operation may cause an increase in complications (e.g., dilatation, infection, hematuria) and costs, as we encountered at our clinic. Holmdahl et al. [19] reported in their study in which they used standard or double HIT to correct VUR that VUR resolved completely or downgraded to grade I after the first injection in 71% of grade III and 52% of grade IV refluxing ureters. In our HIT group, with the first injection, VUR resolved completely in 73.9% of grade III and 55.1% of grade IV refluxing ureters. It may seem that our results are similar to those of Holmdahl et al. [19]. However, our results differ in that our group did not include patients downgraded to grade I.
It has been speculated that dilatation of the upper tract, which can occasionally be seen on the ultrasound following injections, is probably due to focal edema, because it always disappears spontaneously a few days later. In the presence of persistent dilatation, initially, a ureteral stent is placed and the patient is followed up. If the problem remains after the stent is removed, open surgery may be applied [20]. In our group, dilatation developed in 11 patients and was resolved in the first week. The reason for dilatation may be due to the higher volume of injection material. The reflux grade of 2 patients who developed contralateral reflux was grade I. In the follow-up, their refluxes disappeared spontaneously without any treatment. We did not encounter any other serious complications during the short- and long-term follow-up.
The modified STING procedure contributed to our success rates, but only the results for grade IV reflux were statistically significant. We preferred this method for its easy application, short learning curve, and effectiveness. We believe that the HIT could provide urologists with increased success rates as the patient population and surgeon experience increase. We also believe that there is a need to conduct studies with larger patient populations to evaluate the success rates of different techniques.
Figures and Tables
References
1. Matouschek E. Treatment of vesicorenal reflux by transurethral teflon-injection (author's transl). Urologe A. 1981; 20:263–264.
2. O'Donnell B, Puri P. Treatment of vesicoureteric reflux by endoscopic injection of Teflon. Br Med J (Clin Res Ed). 1984; 289:7–9.
3. Puri P, Kutasy B, Colhoun E, Hunziker M. Single center experience with endoscopic subureteral dextranomer/hyaluronic acid injection as first line treatment in 1,551 children with intermediate and high grade vesicoureteral reflux. J Urol. 2012; 188:4 Suppl. 1485–1489.
4. Routh JC, Kramer SA, Inman BA, Ashley RA, Wolpert JJ, Vandersteen DR, et al. Utility of dextranomer/hyaluronic acid injection in setting of bladder and ureteral anomalies. Urology. 2008; 71:435–438.
5. Capozza N, Lais A, Matarazzo E, Nappo S, Patricolo M, Caione P. Influence of voiding dysfunction on the outcome of endoscopic treatment for vesicoureteral reflux. J Urol. 2002; 168(4 Pt 2):1695–1698.
6. Karami H, Razi A, Mazloomfard MM, Javanmard B. Is there any role for urodynamic study in children with high-grade vesicoureteral reflux? Urology. 2012; 79:888–891.
7. Mendez R, Somoza I, Tellado MG, Liras J, Sanchez A, Pais E, et al. Predictive value of clinical factors for successful endoscopic correction of primary vesicoureteral reflux grades III-IV. J Pediatr Urol. 2006; 2:545–550.
8. Lackgren G, Kirsch AJ. Surgery illustrated - surgical atlas endoscopic treatment of vesicoureteral reflux. BJU Int. 2010; 105:1332–1347.
9. Kirsch AJ, Perez-Brayfield M, Smith EA, Scherz HC. The modified sting procedure to correct vesicoureteral reflux: improved results with submucosal implantation within the intramural ureter. J Urol. 2004; 171(6 Pt 1):2413–2416.
10. Cerwinka WH, Scherz HC, Kirsch AJ. Dynamic hydrodistention classification of the ureter and the double hit method to correct vesicoureteral reflux. Arch Esp Urol. 2008; 61:882–887.
11. Sung J, Skoog S. Surgical management of vesicoureteral reflux in children. Pediatr Nephrol. 2012; 27:551–561.
12. Capozza N, Caione P. Modification of the sting procedure for vesicoureteral reflux: ureteral repositioning and injection. Arch Esp Urol. 2008; 61:254–257.
13. Routh JC, Reinberg Y, Ashley RA, Inman BA, Wolpert JJ, Vandersteen DR, et al. Multivariate comparison of the efficacy of intraureteral versus subtrigonal techniques of dextranomer/hyaluronic acid injection. J Urol. 2007; 178(4 Pt 2):1702–1705.
14. Molitierno JA, Scherz HC, Kirsch AJ. Endoscopic treatment of vesicoureteral reflux using dextranomer hyaluronic acid copolymer. J Pediatr Urol. 2008; 4:221–228.
15. Gupta A, Snodgrass W. Intra-orifice versus hydrodistention implantation technique in dextranomer/hyaluronic acid injection for vesicoureteral reflux. J Urol. 2008; 180:4 Suppl. 1589–1592.
16. Routh JC, Reinberg Y. Predicting success in the endoscopic management of pediatric vesicoureteral reflux. Urology. 2010; 76:195–198.
17. Routh JC, Inman BA, Reinberg Y. Dextranomer/hyaluronic acid for pediatric vesicoureteral reflux: systematic review. Pediatrics. 2010; 125:1010–1019.
18. Lavelle MT, Conlin MJ, Skoog SJ. Subureteral injection of Deflux for correction of reflux: analysis of factors predicting success. Urology. 2005; 65:564–567.
19. Holmdahl G, Brandstrom P, Lackgren G, Sillen U, Stokland E, Jodal U, et al. The Swedish reflux trial in children: II. Vesicoureteral reflux outcome. J Urol. 2010; 184:280–285.
20. Nseyo U, Mancini JG, Wiener JS. Symptomatic bilateral delayed partial ureteral obstruction after bilateral endoscopic correction of vesicoureteral reflux with dextranomer/hyaluronic acid polymer. Urology. 2013; 81:184–187.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download