Abstract
Purpose
It has been reported that varicocele is found less frequently in obese men. Accordingly, we evaluated varicocele patients and statistically analyzed the correlation between varicocele and somatometric parameters.
Materials and Methods
A total of 211 patients underwent surgery for varicoceles. All patients underwent history taking, physical examination, and scrotal ultrasound to determine the presence and severity of varicocele. An age-matched control group consisted of 102 patients who were found not to have varicocele according to physical examinations and scrotal ultrasound. The age, weight, height, and body mass index (BMI) of the two groups were compared. The statistical analyses were performed by use of PASW Statistics ver. 18.0. A p-value of less than 0.05 was used for statistical significance.
Results
In the varicocele group, the mean age, height, weight, and BMI were 29.42±14.01 years, 168.53±9.97 cm, 62.14±13.17 kg, and 21.66±3.21 kg/m2, respectively. The distribution of varicocele grade was as follows: 103 (48.8%) grade III, 72 (34.1%) grade II, and 36 (17.1%) grade I. In the control group, the mean age, height, weight, and BMI were 30.83±17.31 years, 161.93±19.83 cm, 64.69±17.86 kg, and 24.04±3.64 kg/m2, respectively. Analyzing these data specifically in adolescents, they showed significant differences in age, height, and BMI (p=0.000, p=0.000, and p=0.004, respectively) between two groups. There were no significant differences in somatometric parameters between patients with different grades of varicocele.
Varicocele is an abnormal tortuous dilatation of the pampiniform plexus in the scrotal portion of spermatic veins that drains blood from the testis. This abnormal venous dilatation is suspected to cause male infertility. The prevalence of varicocele is 30%-40% and 15%-20% in infertile men and in the general population, respectively [1]. Recently, varicocele was reported to be found less frequently in obese men and more frequently in tall and lean men [2]. Handel et al. [3] suggested that this is due to a decreased nutcracker effect to the left testicular vein with increasing body mass index (BMI). However, Delaney et al. [4] insisted that patients with varicoceles were heavier with no difference in BMI, even though patients with varicoceles were taller. To investigate this concept further, we evaluated 211 varicocele patients and statistically analyzed the correlation between varicocele and somatometric parameters.
A total of 211 consecutive patients underwent surgery for varicoceles at our department from January 2003 to December 2012. This retrospective study was approved by the Institutional Review Board of Daegu Catholic University Medical Center, which waived the requirement for written informed consent.
All patients underwent history taking, physical examination, and scrotal ultrasound to determine the presence and severity of varicocele. Among them, 23 patients (11%) had bilateral varicocele and were assigned a higher grade.
The control group consisted of 102 patients who visited who visited urology department in Daegu Catholic University Medical Center for scrotal discomfort during the same period but were found to not have varicocele on physical examinations and scrotal ultrasound. Somatometric parameters including age, weight, height, and BMI were measured in both groups and compared. To compare the data in more homogeneous groups, we divided both groups into adolescents (age≤20 years) and adults (age>20 years) and compared the somatometric data between these subgroups. BMI was calculated from height and weight data according to the formula of BMI=weight (kg)/height (m)2. The statistical analyses were performed by use of PASW Statistics ver. 18.0 (IBM Co., Armonk, NY, USA). Data were presented as means plus or minus standard deviations. One-way analysis of variance was used to analyze differences in somatometric measurements among the varicocele grades. Two sample t-test analysis was used to compare the somatometric parameters between the groups. A p-value of less than 0.05 was used as a threshold for statistical significance.
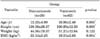
In the varicocele group, the mean age, height, weight, and BMI were 29.42±14.01 years, 168.53±9.97 cm, 62.14±13.17 kg, and 21.66±3.21 kg/m2, respectively. The distribution of varicocele grade was as follows: 103 (48.8%) grade III, 72 (34.1%) grade II, and 36 (17.1%) grade I. In the control group, the mean age, height, weight, and BMI were 30.83±17.31 years, 161.93±19.83 cm, 64.69±17.86 kg, and 24.04±3.64 kg/m2, respectively. Differences in somatometric parameters between the varicocele and control group are shown in Table 1. There were no significant differences in age or weight (p=0.227 and p=0.203, respectively), but significant differences were found in height and BMI (p=0.002 and p=0.000, respectively) between the two groups (Table 1).
To compare the data in more homogeneous groups, the data for 63 adolescents and 148 adults in the varicocele group were compared with the data for 28 adolescents and 73 adults in the control group. In adolescents, significant differences were found between the two groups in age, height, and BMI (p=0.000, p=0.000, and p=0.004, respectively) (Tables 2, 3). In adults, there were no significant differences in height, weight, or BMI (p=0.061, p=0.175, and p=0.481, respectively) (Table 4). Somatometric parameters with different grades of varicocele in adolescents are shown in Table 5. There were no significant differences in age, height, weight, or BMI (p=0.109, p=0.098, p=0.109, and p=0.142, respectively) according to varicocele grade.
Varicocele is frequently found in adolescent males as a result of abnormal tortuous dilatation of the spermatic vein. There have been several reports that varicoceles are found less frequently in obese adolescents [2]. In 1957, Smith [5] reported that patients with varicoceles were taller and heavier. Thereafter, in 1980, Shafik and Bedeir [6] reported that a greater height was associated with an increased hydrostatic pressure of the spermatic vein, which may strain the valve mechanisms in the veins, resulting in the development of varicocele. In 1994, Braedel et al. [7] reported that this hypothesis was in accordance with the theory that describes malfunctioning venous valves as a potential cause of varicocele formation. It is also known that 75% to 90% of varicoceles are left-sided and may result from the more increased pressure in the left internal spermatic vein [8]. This may partly be due to the increased length of left-side venous drainage into the inferior vena cava [6]. In particular, increased pressure in the left spermatic vein may result from compression of the left renal vein between the aorta and the superior mesenteric artery, a phenomenon known as the nutcracker effect [9]. Tsao et al. [10] showed that the prevalence and severity of varicoceles were inversely correlated with obesity, which indicates that obesity may result in a decreased nutcracker effect. Handel et al. [3] reported that the prevalence of varicocele decreases with increasing BMI because of increased adipose tissue, which decreases compression of the left renal vein. However, Delaney et al. [4] reported that patients with varicoceles were taller, but contrary to the previous reports [11], they were heavier and BMI was not significantly different compared with respective growth charts for boys aged 2 to 20 years. They hypothesized that taller individuals were more susceptible to increased hydrostatic pressure owing to the increased length required for drainage of the spermatic vein. They also postulated that height is associated with a smaller angle of the superior mesenteric artery with the aorta, increasing the chance of the nutcracker effect on the left renal vein. They also explained that the differences with weight and BMI results in other reports might be due to the difference in study design. The mean age of 14.3 years (range, 11-19 years) may be associated with increased body musculature. Our data showed that even though varicocele in adults was not related with somatometric parameters, varicocele in adolescents was found more frequently in taller patients and less frequently in obese patients (higher BMI). This result is partly in contrast with the result of Delaney, but may reconfirm the studies of others. Our study has the strength that both the varicocele and the control groups were evaluated by scrotal ultrasound and thorough physical examination. However, the study also had a limitation due to the retrospective nature of the study design. A well-designed prospective study may be needed in the future.
Figures and Tables
TABLE 2
Comparison of somatometric parameters according to varicocele by two-sample t-test in adolescents
References
1. Jarow JP. Effects of varicocele on male fertility. Hum Reprod Update. 2001; 7:59–64.
2. Nielsen ME, Zderic S, Freedland SJ, Jarow JP. Insight on pathogenesis of varicoceles: relationship of varicocele and body mass index. Urology. 2006; 68:392–396.
3. Handel LN, Shetty R, Sigman M. The relationship between varicoceles and obesity. J Urol. 2006; 176:2138–2140.
4. Delaney DP, Carr MC, Kolon TF, Snyder HM 3rd, Zderic SA. The physical characteristics of young males with varicocele. BJU Int. 2004; 94:624–626.
5. Smith SM. Body size and weight in relation to varicocoele and hernia. Ann Hum Genet. 1957; 21:304–312.
6. Shafik A, Bedeir GA. Venous tension patterns in cord veins. I. In normal and varicocele individuals. J Urol. 1980; 123:383–385.
7. Braedel HU, Steffens J, Ziegler M, Polsky MS, Platt ML. A possible ontogenic etiology for idiopathic left varicocele. J Urol. 1994; 151:62–66.
8. Coolsaet BL. The varicocele syndrome: venography determining the optimal level for surgical management. J Urol. 1980; 124:833–839.
9. Nagler HM, Zippe CD. Varicocele: current concepts and treatment. In : Lipshultz LI, Howards SS, editors. Infertility in the male. 2nd ed. St. Louis: Mosby;1991. p. 313–336.
10. Tsao CW, Hsu CY, Chou YC, Wu ST, Sun GH, Yu DS, et al. The relationship between varicoceles and obesity in a young adult population. Int J Androl. 2009; 32:385–390.
11. Soylemez H, Atar M, Ali Sancaktutar A, Bozkurt Y, Penbegul N. Varicocele among healthy young men in Turkey; prevalence and relationship with body mass index. Int Braz J Urol. 2012; 38:116–121.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download