Abstract
Purpose
There is some debate over the necessity of ureteral stenting after laparoscopic ureterolithotomy. We evaluated the need for ureteral stenting after retroperitoneal laparoscopic ureterolithotomy (RLU).
Materials and Methods
Between January 2009 and January 2013, 41 patients underwent RLU to remove upper ureteral stones. The retroperitoneal approach was used in all patients by a single surgeon. A double J (D-J) stent was placed in the first 17 patients after the procedure but not in any of the next 24 patients.
Results
The mean patient age, serum creatinine levels, and stone size were not significantly different between the two groups. The stone-free rate was 100%. The mean operative time was significantly shorter in the stentless group than in the stent group (59.48 minutes vs. 77.88 minutes, p<0.001). Parenteral analgesic use and anticholinergic medication use were observed in the stent group only. The blood loss, drain removal day, and hospital stay were not significantly different between the two groups. No other significant complications occurred during or after the operation in any patients.
Conclusions
RLU is a safe and effective treatment modality for large impacted ureteral stones. In this study, D-J stent placement was not necessary after RLU. In the future, large-scale studies of RLU without D-J stenting, especially on the frequency of the development of complications according to the surgical technique, may be needed.
Retroperitoneal laparoscopic ureterolithotomy (RLU) is recognized as a method that can replace open ureterolithotomy as a first-line treatment for large impacted upper or midureteral calculi and as a salvage treatment for use when ureteroscopic removal of stone (URS) or extracorporal shock wave lithotripsy (ESWL) has failed [1,2,3]. When RLU is used to treat stones larger than 1 cm, the stone-free rate reaches 100%, which confirms RLU as an effective minimally invasive treatment modality [4,5,6,7,8]. The operation-related complications include mainly prolonged urine leakage and postoperative ureteral stenosis. Some authors support the idea of deploying a double J (D-J) stent after the stone is removed to prevent urine leakage and ureteral stricture [9,10,11], but others do not agree because D-J stenting has shown no correlation with the complication rate and increases the number of inconveniences to the patient, such as lower urinary tract symptoms, pain, and cost of cystoscopic removal of the D-J stent [4,12]. Because of this controversy, in the present study, we assessed the need for ureteral stents after RLU.
Between June 2010 and January 2013, RLU was performed by one surgeon in Chonbuk National University Hospital on 41 patients who had impacted upper ureteral stones larger than 1 cm and who had experienced unsuccessful ESWL or URS. The retroperitoneal approach was used in all patients. All data were retrospectively collected by medical records review. Exclusion criteria included a positive urine culture, which is a conventional contraindication to surgery.
Before the operation, the age, gender, and body mass index of the patients and the results of their physical examinations and laboratory tests (urinalysis, urine culture, and renal function test) were obtained, as were their non-contrast computed tomography (CT) images. The kidney, ureter, and bladder x-ray, the postoperative laboratory test results, and the physical examination results 1 week and 3 months after discharge were reviewed, and additional imaging studies were performed when needed.
Of the total 41 patients, the first 17 patients received D-J stents and the next 24 patients did not. Thus, the stent group consisted of patients in whom a D-J stent was placed and the stentless group consisted of patients treated without a D-J stent.
The surgery was performed with the patient under general anesthesia. With the patient in the lateral position, a 1-cm skin incision was made at the umbilicus level on the midaxillary line, and blunt dissection was performed on the muscle and the dorsolumbar fascia by using straight kelly forceps. A retroperitoneal space was made by using a lubricated index finger, and additional space was secured by using an air balloon dilator. A 10-mm camera port was inserted and two 5-mm ports were inserted under direct vision. Using CO2 gas, pneumoperitoneum was maintained at a pressure of 11 to 13 mmHg. The surgery was performed in the following order: ureter identification, minimum dissection of ureter, confirmation of the stone location, longitudinal incision of the proximal ureteral area of the bulge caused by the stone by use of a cold knife (because it results in less inflammation of the tissue and less injury to the vasculature), stone extraction by use of a right-angled clamp, meticulous interrupted intracorporeal suture of the incised ureter by use of Vicryl 5-0, 5-mm camera insertion and stone removal through the 10-mm port, and placement of a drain via a 5-mm port.
Baseline characteristics, operation time, stone-free status, blood loss, drain removal, and postoperative complications of the two groups were analyzed. Statistical analysis was performed by using SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA). The data were analyzed by using the Mann-Whitney test and a p-value <0.05 was considered statistically significant.
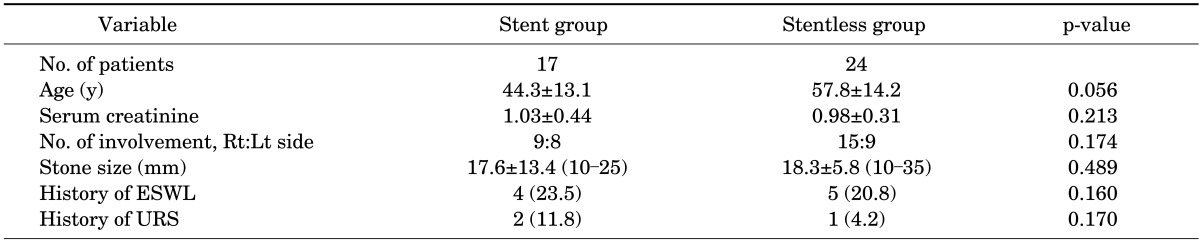
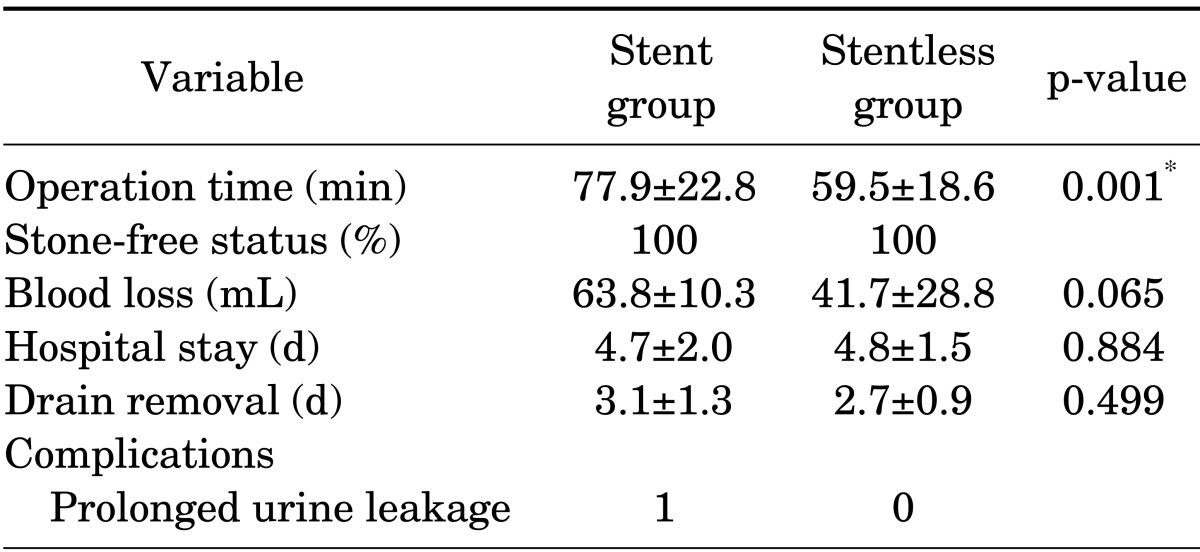
The mean age of the patients, serum creatinine level, and stone size (stent group, 17.64 mm; stentless group, 18.26 mm) were not significantly different between the two groups. Nine patients had a history of ESWL, and three had a history of URS. The demographic and clinical characteristics of the patients are shown in Table 1. The retroperitoneal approach was used in all patients by a single surgeon. Of the total 41 patients, the first 17 patients received a D-J stent and the next 24 patients did not. The mean operative time was significantly shorter in the stentless group than in the stent group (59.48 minutes vs. 77.88 minutes, p<0.001). Parenteral analgesic use and anticholinergic medication were observed in the stent group only (analgesics, 3 patients; anticholinergics, 2 patients). The mean blood loss, mean hospital stay, and mean drain removal day were not significantly different between the two groups. The stone-free rate was 100%, and no case was converted to open surgery. Prolonged urine leakage was reported in one patient in the stent group. The urine leak ceased without any intervention at 5 days postoperatively. No other complications, such as blood transfusion, febrile urinary tract infection, wound infection, or paralytic ileus, were reported.
The intra- and postoperative data of the subjects are shown in Table 2. At the 1-week and 3-month follow-up, eight patients complained of mild flank pain. The non-enhanced CT images of the eight patients showed no findings of hydroureteronephrosis or ureteral stricture. At the next follow-up, the patients' symptoms had spontaneously disappeared.
Less invasive laparoscopic ureterolithotomy (LU) has been recognized as the first-line treatment for 1.5-cm or larger upper or midimpacted ureteral stones [1,4,13,14,15] and as a salvage treatment for unsuccessful URS and ESWL [4,15,16]. When a skilled surgeon performs LU for a 1-cm or larger upper ureteral stone, the stone-free rate reaches 100%, as it did in this study [4,5,6,7,8]. Wickham [5] introduced laparoscopic retroperitoneoscopic ureterolithotomy in 1979, and Raboy et al. [9] performed laparoscopic transperitoneal ureterolithotomy for the first time in 1992. Compared with the transperitoneal approach, the retroperitoneal approach is reported to have better outcomes in terms of pain, ileus, port site hernia, and hospital stay [8,17,18,19]. Nevertheless, when the transperitoneal approach was used, a larger working space could be secured and the anatomical landmark could be easily confirmed, unlike in the retroperitoneal approach [20,21]. Upon consideration of the location of the ureteral stone and its anatomical relationship, the method of approach was determined before the surgery was performed. We believe that selection of the approach before the LU results in a shorter operative time and an enhanced success rate.
There is no definite answer to the question of whether a need exists to place a D-J stent after LU. A group of surgeons support the idea of placement of the D-J stent to prevent urine from leaking [8,9,10,11], but another group recommends that a stent not be used and instead that solely intracorporeal suturing be performed [4,12]. Karami et al. [22] compared the cases in which a D-J stent was used with those in which it was not used and reported that the use of the D-J stent significantly decreased the development of complications without extending the operative time. Accordingly, they supported the placement of a stent. However, Hammady et al. [6] compared a stent group with a stentless group and reported that the stentless group asked for a lower dose of analgesics and that their operative time was shorter and more economical without an increase in complications compared with the stent group. Accordingly, they supported the method without D-J stenting. Kijvikai and Patcharatrakul [23] suggested the use of the D-J stent only in cases of severe ureteral inflammation in which ureteral sutures cannot be performed. In 2011, we decided to start to perform RLU without D-J stenting according to the results of this study. However, we have not experienced a case in which suturing could not be performed because of severe ureteral inflammation.
Nouira et al. [2] recommended the use of a cold knife to make an incision on the ureter to prevent ureteral strictures. By contrast, other groups have suggested that an electric hook is easier to use in ureterotomy than a cold knife and does not cause any problems [6,7,22]. We thought that the use of the electric hook would not be absolutely free from the ischemic damage caused by capillary injury nor from direct tissue damage; thus, we used the cold knife for the longitudinal ureterotomy. Many surgeons have performed ureterotomy directly on the site of the bulge of the ureter [6,23,24], but we used a cold knife to make a longitudinal incision of the proximal ureteral bulge caused by the stone. In most cases in which the stone was impacted, the ureteral mucosa showed inflammation or ulceration. We thought that when the bulge was incised, suturing might be difficult, the possibility of recovery after the suturing might decrease, and the possibility of ureteral stricture due to adhesion at the suture site would increase. Thus, we incised the proximal ureter of the bulge. From our experience, the process of removing the stone by use of a right-angle clamp after incising the proximal ureter of the area of the bulge with a cold knife was not difficult. Comparative studies on the development of complications in cases that involved the use of a cold knife versus an electric hook, and of bulge site ureterotomy versus non-bulge-site ureterotomy, may be needed in the future.
The limitations of our study included the lack of an imaging study such as ultrasonography or CT scans to confirm ureteral strictures in all the subjects; these were only performed on the eight patients who complained of mild flank discomfort at the follow-up. None of the eight patients was confirmed to have had ureteral stricture or hydroureteronephrosis. Selective imaging studies were conducted because no patient had a significantly increased serum creatinine level after surgery and because of the high cost and the risk of radiation exposure of the imaging study. Another limitation was the short follow-up period; the shortest case was 5 months. Although the most extensive period of development of ureteral stricture after LU was not clearly investigated, the follow-up period in this study is considered short. In the future, long-term and large-scale studies may be needed.
Through this study, RLU was reconfirmed as a safe, effective, and minimally invasive treatment method for large stones or for cases of unsuccessful treatment with other methods. In this study, no complications such as urine leakage or ureteral stricture developed when the D-J stent was not used. We believe that laparoscopic ureteral stone surgery without D-J stenting is safe, economical, and less inconvenient for patients. In the future, large-scale studies that are focused on the development of complications, such as urine leakage and ureteral stricture, according to the surgical technique may be needed.
References
1. Wolf JS Jr. Treatment selection and outcomes: ureteral calculi. Urol Clin North Am. 2007; 34:421–430. PMID: 17678991.

2. Nouira Y, Kallel Y, Binous MY, Dahmoul H, Horchani A. Laparoscopic retroperitoneal ureterolithotomy: initial experience and review of literature. J Endourol. 2004; 18:557–561. PMID: 15333221.

3. El-Moula MG, Abdallah A, El-Anany F, Abdelsalam Y, Abolyosr A, Abdelhameed D, et al. Laparoscopic ureterolithotomy: our experience with 74 cases. Int J Urol. 2008; 15:593–597. PMID: 18479354.

4. Gaur DD, Trivedi S, Prabhudesai MR, Madhusudhana HR, Gopichand M. Laparoscopic ureterolithotomy: technical considerations and long-term follow-up. BJU Int. 2002; 89:339–343. PMID: 11872020.

5. In : Wickham JE, editor. The surgical treatment of renal lithiasis. In : Wickham JE, editor. Urinary calculus disease. New York: Churchill Livingstone;1979. p. 145–198.
6. Hammady A, Gamal WM, Zaki M, Hussein M, Abuzeid A. Evaluation of ureteral stent placement after retroperitoneal laparoscopic ureterolithotomy for upper ureteral stone: randomized controlled study. J Endourol. 2011; 25:825–830. PMID: 21457084.

7. Harewood LM, Webb DR, Pope AJ. Laparoscopic ureterolithotomy: the results of an initial series, and an evaluation of its role in the management of ureteric calculi. Br J Urol. 1994; 74:170–176. PMID: 7921933.

8. Singh V, Sinha RJ, Gupta DK, Kumar M, Akhtar A. Transperitoneal versus retroperitoneal laparoscopic ureterolithotomy: a prospective randomized comparison study. J Urol. 2013; 189:940–945. PMID: 23023151.

9. Raboy A, Ferzli GS, Ioffreda R, Albert PS. Laparoscopic ureterolithotomy. Urology. 1992; 39:223–225. PMID: 1532102.

10. Skrepetis K, Doumas K, Siafakas I, Lykourinas M. Laparoscopic versus open ureterolithotomy. A comparative study. Eur Urol. 2001; 40:32–36. PMID: 11528174.
11. Kiyota H, Ikemoto I, Asano K, Madarame J, Miki K, Yoshino Y, et al. Retroperitoneoscopic ureterolithotomy for impacted ureteral stone. Int J Urol. 2001; 8:391–397. PMID: 11442662.

12. Demirci D, Gulmez I, Ekmekcioglu O, Karacagil M. Retroperitoneoscopic ureterolithotomy for the treatment of ureteral calculi. Urol Int. 2004; 73:234–237. PMID: 15539842.

13. Anagnostou T, Tolley D. Management of ureteric stones. Eur Urol. 2004; 45:714–721. PMID: 15149742.

14. Leonardo C, Simone G, Rocco P, Guaglianone S, Di Pierro G, Gallucci M. Laparoscopic ureterolithotomy: minimally invasive second line treatment. Int Urol Nephrol. 2011; 43:651–654. PMID: 21110095.

15. Knoll T, Alken P, Michel MS. Progress in management of ureteric stones. EAU Update Series. 2005; 3:44–50.

16. Gettman MT, Segura JW. Management of ureteric stones: issues and controversies. BJU Int. 2005; 95(Suppl 2):85–93. PMID: 15720341.

17. Farooq Qadri SJ, Khan N, Khan M. Retroperitoneal laparoscopic ureterolithotomy: a single centre 10 year experience. Int J Surg. 2011; 9:160–164. PMID: 21059419.
18. Sinha R, Sharma N. Retroperitoneal laparoscopic management of urolithiasis. J Laparoendosc Adv Surg Tech A. 1997; 7:95–98. PMID: 9459808.

19. Kumar M, Kumar R, Hemal AK, Gupta NP. Complications of retroperitoneoscopic surgery at one centre. BJU Int. 2001; 87:607–612. PMID: 11350398.

20. Al-Sayyad A. Laparoscopic transperitoneal ureterolithotomy for large ureteric stones. Urol Ann. 2012; 4:34–37. PMID: 22346099.

21. Henkel TO, Rassweiler J, Alken P. Ureteral laparoscopic surgery. Ann Urol (Paris). 1995; 29:61–72. PMID: 7646000.
22. Karami H, Javanmard B, Hasanzadeh-Hadah A, Mazloomfard MM, Lotfi B, Mohamadi R, et al. Is it necessary to place a Double J catheter after laparoscopic ureterolithotomy? A four-year experience. J Endourol. 2012; 26:1183–1186. PMID: 22540150.

23. Kijvikai K, Patcharatrakul S. Laparoscopic ureterolithotomy: its role and some controversial technical considerations. Int J Urol. 2006; 13:206–210. PMID: 16643610.

24. Modi P, Vyas J, Dholaria P, Sharma V. Retroperitoneoscopic ureterolithotomy. Indian J Urol. 2011; 27:420–421. PMID: 22022075.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download