Abstract
Vesicoenteric fistula is a rare complication of bladder squamous cell carcinoma. We report the case of a 70-year-old male who complained of painless, total gross hematuria. Abdominopelvic computed tomography (CT) revealed an approximately 2.7-cm lobulated and contoured enhancing mass in the bladder dome. We performed partial cystectomy of the bladder dome after transurethral resection of the bladder. The biopsy result was bladder squamous cell carcinoma, with infiltrating serosa histopathologically, but the resection margin was free. Postoperatively, follow-up CT was done after 3 months. Follow-up CT revealed an approximately 4.7-cm×4.0-cm lobulated, contoured, and heterogeneous mass in the bladder dome. A vesicoenteric fistula was visible by cystography. Here we report this case of a vesicoenteric fistula due to bladder squamous cell carcinoma.
Vesicoenteric fistula is a rare disease, with an estimated 2 to 3 patients per 10,000 hospital admissions and with an annual incidence of 0.5 per 100,000 [1]. Vesicoenteric fistula is usually secondary to an inflammatory or malignant bowel etiology such as diverticulitis, colorectal carcinoma, or Crohn's disease [2]. Vesicoenteric fistula due to primary bladder squamous cell carcinoma is extremely rare. Here we report the case of patient with a vesicoenteric fistula secondary to bladder squamous cell carcinoma.
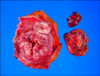
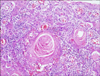
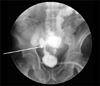
A 70-year-old male patient presented with painless, total gross hematuria. He had a history of urethral stricture due to a motor vehicle accident, and visual internal urethrotomy had been performed 9 years previously. He also had hypertension that was being treated medically. Abdominopelvic computed tomography (CT) showed an approximately 2.7-cm lobulated and contoured enhancing mass in the bladder dome within the diverticulum with no definite pelvic lymph node enlargement (Fig. 1). After transurethral resection of the bladder tumor, we performed a partial cystectomy at the bladder dome. Because the tumor was a small 2.7-cm mass, without pelvic lymph node enlargement, and limited to the bladder dome on CT, we performed partial cystectomy. The margins were negative in the frozen biopsy. Grossly, firm whitish gray masses were seen (Fig. 2). The pathology report was squamous cell carcinoma, infiltrating the serosa. Microscopically, the bladder tumor was composed of keratin-producing malignant cells (Fig. 3).
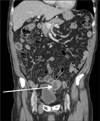
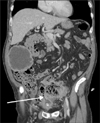
Three months postoperatively, frequency and nocturia occurred. Follow-up abdominopelvic CT showed a new approximately 4.7-cm×4.0-cm lobulate, heterogeneous mass in the dome of the bladder. CT also revealed another 2.9-cm×2.3-cm hypodense mass with peripheral rim enhancement in the right upper abdomen (Fig. 4). After we inserted a Foley catheter, bowel materials and feces were evacuated through the Foley catheter. Cystography showed that contrast media leaked to the ileum (Fig. 5). Abdominopelvic CT showed an enlarged mass at the dome of the bladder and noted communication with the sigmoid colon (Fig. 6). Ileostomy was done in the department of surgery. Eventually, bladder squamous cell carcinoma spread to multiple organs and the patient died of multiple organ failure 6 months later.
Vesicoenteric fistulas are usually secondary to an inflammation or malignancy of the bowel such as diverticulitis (52%), Crohn's disease (18%), carcinoma of the colon (11%), or other malignant pelvic conditions (9%) and uncommonly to infection, trauma, radiation, or iatrogenic surgical trauma [2]. Few cases of urological vesicoenteric fistulas have been described in the literature, and most of these were in the form of isolated case reports [3]. The peak incidence of vesicoenteric fistula is between 55 and 65 years of age.
The most common clinical presentations of vesicoenteric fistulas are urinary tract infection (100%), pneumaturia (66%), fecaluria (50%), and hematuria (22.6%) [4], because the high bladder compliance and low intravesical pressure favor the unidirectional flow of bowel contents to the bladder. The classical presentation of vesicoenteric fistula is described as Gouverneur's syndrome and consists of suprapubic pain, urinary frequency, dysuria, and tenesmus [5]. Thus, in some case, if refractory to antibiotic therapy, urinary tract infection may suggest a vesicoenteric fistula. Vesicoenteric fistula can be diagnosed by use of tests such as cystoscopic examination, cystography, excretory urography, barium enema, and CT. Cystoscopic examination is the most sensitive investigation, with accuracy of 79% [6]. Sometimes, nonspecific and localized erythema and a papillary lesion make diagnosis difficult. Cystography, excretory urography, and barium enema with or without the small bowel have lower detection rates of 20% to 35% [6]. Cross-sectional imaging, especially CT scanning, has become the imaging modality of choice [5]. In CT findings, bladder wall thickening adjacent to the loop of thickened colon, bladder air, and colonic diverticula are suspicious of vesicoenteric fistula. Oral ingestion of activated charcoal will appear in the urine as black particles in cases of vesicoenteric fistulas [5]. Our case revealed bladder wall thickening adjacent to the loop of thickened bowel and bladder air in the CT.
Both single and multistage procedures have been advocated in the treatment of vesicoenteric fistulas, depending on the clinical circumstances. Some medical treatments, such as octreotide, are also available for malignant vesicoenteric fistula [7]. In surgical treatment, minimally invasive and organ-preserving surgery, such as laparoscopic bladder-preserving surgery, should be performed in the case of a vesicoenteric fistula caused by benign diseases [8]. In a malignant vesicoenteric fistula, Whiteley Jr and Grabstald [9] proposed that a one-stage en bloc resection of the colonic malignancy and involved bladder portion is a reasonable and safe procedure, thus avoiding a total cystectomy [3,4]. Vidal Sans et al. [10], however, reported that surgical morbidity and mortality is relatively high, especially in fistula resulting from malignancy.
Figures and Tables
FIG. 1
Computed tomography of the lower abdomen showing an approximately 2.7-cm lobulated and contoured enhancing mass in the bladder dome, within a diverticulum (arrow).
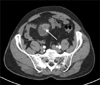
FIG. 2
An ulcerofungating friable mass measuring 5.5 cm×4.5 cm×1.5 cm. Upon sectioning, firm whitish gray masses were seen.
References
1. Karamchandani MC, West CF Jr. Vesicoenteric fistulas. Am J Surg. 1984; 147:681–683.
2. Kirsh GM, Hampel N, Shuck JM, Resnick MI. Diagnosis and management of vesicoenteric fistulas. Surg Gynecol Obstet. 1991; 173:91–97.
3. Dawam D, Patel S, Kouriefs C, Masood S, Khan O, Sheriff MK. A "urological" enterovesical fistula. J Urol. 2004; 172:943–944.
4. Larsen A, Bjerklund Johansen TE, Solheim BM, Urnes T. Diagnosis and treatment of enterovesical fistula. Eur Urol. 1996; 29:318–321.
5. Rovner ES. Urinary tract fistulae. In : Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 10th ed. Philadelphia: Saunders;2011. p. 2252–2254.
6. Carson CC, Malek RS, Remine WH. Urologic aspects of vesicoenteric fistulas. J Urol. 1978; 119:744–746.
7. Shinjo T, Kondo Y, Harada K, Yamazaki J, Okada M. Treatment of malignant enterovesical fistula with octreotide. J Palliat Med. 2009; 12:965–967.
8. Mizushima T, Ikeda M, Sekimoto M, Yamamoto H, Doki Y, Mori M. Laparoscopic bladder-preserving surgery for enterovesical fistula complicated with benign gastrointestinal disease. Case Rep Gastroenterol. 2012; 6:279–284.
9. Whiteley HW Jr, Grabstald H. Conservative management of distal large bowel cancer invading the urinary bladder. Clin Bull. 1975; 5:99–101.
10. Vidal Sans J, Pradell Teigell J, Palou Redorta J, Villagrasa Serrano M, Banus Gassol JM. Review of 31 vesicointestinal fistulas: diagnosis and management. Eur Urol. 1986; 12:21–27.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download