Abstract
Purpose
To report the outcome of laparoscopic pyelo- and ureterolithotomies with the aid of flexible nephroscopy.
Materials and Methods
A retrospective analysis was performed in 71 patients with complex renal stones or large and impacted proximal ureteral stones. Patients underwent laparoscopic pyelo- or ureterolithotomies with or without the removal of small residual stones by use of flexible nephroscopy between July 2005 and July 2010. Operative success was defined as no residual stones in the intravenous pyelogram at 12 weeks postoperatively. Perioperative results and surgical outcomes were analyzed.
Results
The patients' mean age was 54.7±13.7 years, and 53 males (74.6%) and 18 females (25.4%) were included. The mean maximal stone size was 19.4±9.4 mm. A total of 47 cases were complex renal stones and 24 cases were impacted ureteral stones. Mean operative time was 139.0±63.7 minutes. Stones were completely removed in 61 cases (85.9%), and no further ancillary treatment was needed for clinically insignificant residual fragments in 7 cases (9.9%). For complex renal stones, the complete stone-free rate and clinically significant stone-free rate were 80.9% and 93.6%, respectively. Multivariate analysis showed that the use of flexible nephroscopy for complex renal stones can reduce the risk of residual stones. A major complication occurred in one case, in which open conversion was performed.
Recently, patients with urinary stones have mostly undergone extracorporeal shock-wave lithotripsy (ESWL), ureterorenoscopic lithotomy, or percutaneous nephrolithotomy (PNL). The stone clearance rate of ESWL monotherapy or PNL ranges from 50% to 80%, which is considered to be relatively low [1,2]. Determining treatment methods becomes even more difficult in patients with complex renal stones because of the anatomic complexity of the renal pelvis and calyces. This difficulty increases the risk of residual stones. Therefore, open stone surgery, despite its invasiveness [3,4], remains a viable option in patients with complex renal stones for maximizing stone clearance rates [5]. However, PNL is preferred because of the extensive scar tissue formation that results from open surgery.
Laparoscopic surgery is currently not a preferred procedure among urologists, and the role of laparoscopic surgery has not been well established [6]. However, laparoscopic stone surgery is still considered to be a safer option than open surgery in cases of failed endourologic management, complex renal calculi, or large and impacted proximal ureteral stones [7]. In such complex cases, even laparoscopic-assisted PNL has been discussed to achieve maximum stone clearance rates [8]. Some studies have also demonstrated that stone clearance rates with the use of flexible equipment in laparoscopic stone surgery vary from 71% to 100% [6,7,8]. The present study attempted to report the surgical outcome of laparoscopic pyelo- and ureterolithotomies with or without the aid of flexible nephroscopy.
A retrospective analysis was performed in 71 patients with complex renal stones or large and impacted proximal ureteral stones who underwent laparoscopic surgery between July 2005 and July 2010. We defined complex stones as a primary renal pelvis stone accompanied by multiple stones scattered in multiple calyces. Approval for this study was granted by the Institutional Review Board of SMG-SNU Boramae Medical Center. All patients underwent laparoscopic pyelo- or ureterolithotomies with or without residual stone removal by use of flexible nephroscopy. Preoperative evaluation included taking a medical history, a physical examination, serum creatinine and hemoglobin measurement, urine analysis and culture, and intravenous pyelogram or computed tomography scan. We reviewed operative and perioperative outcomes according to the use of flexible nephroscopy. The postoperative presence of residual stones and complications were also evaluated. Postoperative serum creatinine was checked 2 weeks after surgery, and operative success was defined as no residual stones in the intravenous pyelogram at 12 weeks postoperatively.
In all patients, prophylactic antibiotic was administered on the day of surgery. Briefly, patients were placed in a modified lateral decubitus position after general anesthesia. Both the surgeon and an assistant were located in front of the patient's abdomen, into which Xcel bladeless trocars (Ethicon Inc., Somerville, NJ, USA) were inserted. Three or four ports were used with a 12-mm camera port at the level of the umbilicus just lateral to the border of the rectus abdominis muscle, as well as 12-mm and 5-mm working ports at the anterior axillary line or subcostal area just next to the border of the rectus abdominis muscle. If necessary, an additional 5-mm port was placed for liver traction while performing stone surgery in the right kidney (Fig. 1). The open Hasson's technique was preferred to the Veress needle technique for the placement of the camera port. In most of the operations, the transperitoneal approach was used to increase the accessibility of the lower-anterior calyx. After pneumoperitoneum was achieved, the white line of Toldt was incised and the colon was reflected medially. Then perirenal dissection was performed to identify the renal pelvis, ureter, and renal pedicle. A pyelotomy or ureterotomy incision was then made with a blade. This incision was extended to a length sufficient for stones to be picked up by a laparoscopic grasper (Fig. 2A). An additional lithoclast was used in one case to fragment a relatively large stone that could not be retracted. After the main stone was removed, flexible nephroscopy was used with a trocar and pyelotomy to look for and pick up stones scattered in multiple calyces if these were suspected on the basis of the preoperative imaging study (Fig. 2B). If a residual stone was detected, a stone basket was used via flexible nephroscopy. Stones were removed by using a specimen retrieval bag and were extracted from the body through the 12-mm working port. After removal of the stone fragments, a decision was made to place a ureteral stent. The incision site was repaired by use of 4-0 absorbable sutures. A drain was placed in all patients. The Foley catheter, surgical drain, and ureteral stent were removed 1 to 3 days, 2 to 4 days, and 2 to 4 weeks after surgery, respectively.
Data were expressed as means±standard deviations. Surgical outcomes according to the use of flexible nephroscopy were analyzed by use of chi-square tests. Logistic regression analysis was performed to find the clinically significant predictors in determining operative success. Values were considered to be statistically significant when p<0.05. All statistical analyses were performed by using commercially available PASW Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA).
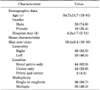
Table 1 shows the patient demographics and stone characteristics. The main stones in 47 cases were complex renal stones and the main stones in 24 cases were ureteral stones. In total, stone clearance was successful in 61 cases (85.9%), and no further ancillary treatment was needed to remove residual stones in 7 cases (9.9%) because the stones were too small to be removed (Table 2). A single case of a residual stone occurred after surgery for ureteral stones, and the other 9 cases occurred after surgery for complex renal stones. When we assessed the operative success rates according to the location of the stones, the risk of residual stones was higher after surgery for complex renal stones than after surgery for ureteral stones with borderline significance (odds ratio [OR], 5.4; 95% confidence interval [CI], 0.65-45.83; p=0.086). In 47 patients with complex renal stones, there were residual stones in one case (4.8%) with and in eight cases (30.8%) without the use of flexible nephroscopy, respectively (OR, 0.113; 95% CI, 0.01-0.99; p=0.03). One case of venous injury occurred during our early experiences, and in that case open conversion was performed immediately to repair the injury. In one of two bleeding cases, blood transfusion was performed. All other complications were minor.
According to a univariate analysis, location of stones (complex renal stones vs. ureteral stones), maximal size of stones, and no use of flexible nephroscopy were significant predictors of residual stones (Table 3). Multivariate analysis showed that stones in the renal pelvis and calyces had a 10-fold higher risk of residual stones than did ureteral stones and that the use of flexible nephroscopy during laparoscopic surgery for complex renal stones can reduce the risk of residual stones by 10-fold. However, age, gender, stone laterality, maximal size of stones, and multiplicity of stones were not significant predictors in the multivariate analysis.
The management of urinary stones has changed during the last 30 years. Laparoscopy has gained a place and has mostly replaced open stone surgery. Laparoscopic ureterolithotomy is technically feasible with fewer postoperative complications than open ureterolithotomy and with the highest level of evidence (IIa). Laparoscopic ureterolithotomy is especially recommended for large impacted stones in cases of failed endourologic management (grade B) [7]. In the largest series of laparoscopic ureterolithotomy to date, Simforoosh et al. [9] reported that laparoscopic ureterolithotomy for 123 patients with ureteral stones resulted in a stone-free rate of 96.7%. Ko et al. [10] reported that laparoscopic ureterolithotomy could be a preferred primary treatment modality for large proximal ureteral stones with ureteral stenosis or kinking rather than ureteroscopic removal. The present study showed a high stone clearance rate (23/24, or 95.8%) by laparoscopic ureterolithotomy.
In the present era, however, laparoscopic pyelolithotomy is rarely indicated despite its feasibility (III/B) [7]. PNL was recommended to be the first-line management for staghorn stones by the American Urological Association [11]. However, we performed laparoscopic pyelolithotomy because it can be a viable treatment option in some cases. It can be an effective option for renal stones with concomitant ureteropelvic junction obstruction [12]. Gaur et al. [13] performed laparoscopic pyelolithotomy successfully for complex staghorn calculi. The laparoscopic approach results in neither significant bleeding nor any parenchymal damage. In contrast, PNL for patients with multiple or large stones in several calices might require multiple punctures, which leads to an added risk of hemorrhage [14]. Such cases may also require more than one session to achieve complete stone extraction for complex stones.
From the point of view of renal function, which modality is better is not yet established. Regarding renal function, debate remains on the damage and functional loss after PNL. Chatham et al. [15] reported no loss of renal function after PNL by mercaptoacetyl triglycine (MAG3) nuclear renography, and Moskovitz et al. [16] reported no significant change of renal function in the treated area, ipsilateral unaffected area, or contralateral kidney by use of Tc 99m-dimercaptosuccinic acid (DMSA) renal scintigraphy. Liou and Streem [17] reported that there were no significant differences between PNL and ESWL in terms of the estimated GFR after the procedure. Also, in patients with chronic kidney disease [18] or a solitary kidney [19], PNL showed preserved or long-term improvement of renal function. However, unlike laparoscopic pyelolithotomy, which does not invade the renal parenchymal tissue, PNL might cause glomerular damage in the postoperative short-term period, especially in patients with high preoperative serum creatinine concentrations, diabetes mellitus, or a long operative time [20]. Bayrak et al. [21] also showed decreased renal function in the early period after PNL, but renal function was not affected by the number of access sites. Even though Demirtas et al. [22] reported preserved renal function as assessed by DMSA after PNL, the study showed significantly decreased differential renal function on the treated side in the early and late postoperative periods and showed insignificant change on the nontreated side in the late postoperative period. In other reports, in which renal function after ESWL and PNL was evaluated with DMSA, there were no significant changes after ESWL but a significant change after PNL [23]. In contrast, laparoscopic stone surgery with a retroperitoneal approach for large proximal ureteral stones has an insignificant impact on renal function [24].
Moreover, laparoscopic surgery showed surgical outcomes comparable to PNL. Wang et al. [25] performed a meta-analysis for the comparison of laparoscopic pyelolithotomy and PNL for renal pelvic calculi greater than 2 cm in diameter. The study showed that laparoscopic pyelolithotomy was associated with lower blood loss and less postoperative fever, but with longer operative times and longer hospital stays, and that there were no significant differences regarding the procedural failure or conversion rate. The present study showed complete stone-free and clinically significant stone-free rates of 80.9% (38/47) and 93.6% (44/47), respectively, for which clinically significant stone-free was defined as stone-free status with clinically insignificant residual fragments of smaller than 4 mm without subjective symptoms for complex renal stones. Even though it is a concern that renal pelvic stricture could occur after surgery, stricture rarely occurs because of the dilated extrarenal pelvis as a result of the chronic obstruction by the stone. In the present study, there were no cases of ureteral or pelvic stricture after surgery. However, repair of the pyelotomy incision requires experienced skills. Laparoscopic pyelolithotomy could be considered as a feasible treatment option in case of complex renal anatomy, failure of endourologic management, and concomitant repair of ureteropelvic junction obstruction [7,25].
For complex renal stones, in the present study, the operative success rate was significantly higher in the group in which intraoperative flexible nephroscopy was used (95.2%) than in the group in which flexible nephroscopy was not used (69.2%). In terms of the clinically significant stone-free rate, the total operative success rate reached 95.8%. Because of the anatomic complexity of renal calyces, flexible nephroscopy has already been demonstrated to be necessary in some previous studies [6,26,27]. In contrast, because of the low rate of residual stones in cases of ureteral stones in which flexible nephroscopy was not used (7.1%, 1 of 14), it is hard to say whether the usefulness of flexible nephroscopy in ureteral stones is statistically significant.
Despite the advantages of the present study, the study had certain limitations. The procedure requires additional equipment such as a camera system. Although flexible nephroscopy did not cause any complications, the irrigation fluids and extensive manipulation may result in an edematous and friable renal pelvic wall.
The biggest drawback of laparoscopic surgery for urinary stone disease is the unique complications that do not occur in other endoscopic surgeries such as PNL or retrograde intrarenal surgery but only in laparoscopic surgery. Despite such concerns, for the present study, only a single case of open conversion occurred during the surgeon's learning curve period. Except for that complication, just three complications that were less than grade IIIa by the modified Clavien-Dindo classification occurred during the learning curve period. Also, there were no complications specific to laparoscopic surgery, for example, bowel injury. Therefore, laparoscopic pyelo- or ureterolithotomy can be performed safely. The retroperitoneal approach was often emphasized to avoid contaminating the peritoneal cavity with potentially infected urine during the surgery for stone removal [28]. However, because of some definite advantages [29], we mostly chose the transperitoneal approach without experiencing any adverse infectious events in any patients. All patients had appropriate antibiotics pre- and postoperatively, and contamination of the peritoneal cavity due to spillage was kept at a minimum during surgery. Hence, the transperitoneal approach could be considered to be as safe as the retroperitoneal approach for stone surgery.
The present study had some limitations because it was based on a retrospective analysis. More limitations are present concerning the definite criteria for the indication for laparoscopic surgery and for not using flexible nephroscopy, for example, size of the smallest calyceal stone. Flexible nephroscopy was used if concomitant calyceal stones had been found by preoperative imaging study. There were three exceptional ureteral stone cases in which flexible nephroscopy was not used. All three cases had clinically insignificant residual fragments and no further management was required during the follow-up period. However, laparoscopic surgery for complex renal or ureteral stones in the present study showed stone clearance rates comparable to those of standard treatment, such as PNL or ureteroscopy, without the addition of specific complications. Furthermore, the use of flexible nephroscopy is a predictor for operative success to remove multiple calyceal stones without any injury to the renal parenchyma. Regarding renal function, the present study evaluated pre- and postoperative renal function by using serum creatinine and estimated GFR. In future studies, however, radionuclide studies should be included to calculate differential renal function accurately and to compare exact pre- and postoperative renal function. Further randomized prospective study with the use of objective criteria to determine whether to use flexible nephroscopy, and comparison of laparoscopic surgery with a standard treatment such as PNL, can give us more information about the excellence or superiority of laparoscopic stone surgery.
Laparoscopic surgery for complex renal and ureteral stones demonstrated a high success rate that was comparable to standard treatment without any specific laparoscopic complications. With the aid of flexible nephroscopy, laparoscopic surgery can be performed effectively with less morbidity in selected complex renal stone cases in the era of endourologic management.
Figures and Tables
 | FIG. 1Placement of ports (A, B) for laparoscopic stone surgery in the right (C) and left (D) kidneys. |
 | FIG. 2Stone removal using laparoscopic graspers or right-angled clamps via an incision site (A) and the use of flexible nephroscopy to pick up residual stones (B). |
References
1. Lam HS, Lingeman JE, Mosbaugh PG, Steele RE, Knapp PM, Scott JW, et al. Evolution of the technique of combination therapy for staghorn calculi: a decreasing role for extracorporeal shock wave lithotripsy. J Urol. 1992; 148(3 Pt 2):1058–1062.
2. Lam HS, Lingeman JE, Barron M, Newman DM, Mosbaugh PG, Steele RE, et al. Staghorn calculi: analysis of treatment results between initial percutaneous nephrostolithotomy and extracorporeal shock wave lithotripsy monotherapy with reference to surface area. J Urol. 1992; 147:1219–1225.
3. Assimos DG, Boyce WH, Harrison LH, McCullough DL, Kroovand RL, Sweat KR. The role of open stone surgery since extracorporeal shock wave lithotripsy. J Urol. 1989; 142(2 Pt 1):263–267.
4. Paik ML, Wainstein MA, Spirnak JP, Hampel N, Resnick MI. Current indications for open stone surgery in the treatment of renal and ureteral calculi. J Urol. 1998; 159:374–378.
5. Marickar YM, Nair N, Varma G, Salim A. Retrieval methods for urinary stones. Urol Res. 2009; 37:369–376.
6. Salvado JA, Guzman S, Trucco CA, Parra CA. Laparoscopic pyelolithotomy: optimizing surgical technique. J Endourol. 2009; 23:575–578.
7. Skolarikos A, Papatsoris AG, Albanis S, Assimos D. Laparoscopic urinary stone surgery: an updated evidence-based review. Urol Res. 2010; 38:337–344.
8. Desai RA, Assimos DG. Role of laparoscopic stone surgery. Urology. 2008; 71:578–580.
9. Simforoosh N, Basiri A, Danesh AK, Ziaee SA, Sharifiaghdas F, Tabibi A, et al. Laparoscopic management of ureteral calculi: a report of 123 cases. Urol J. 2007; 4:138–141.
10. Ko YH, Kang SG, Park JY, Bae JH, Kang SH, Cho DY, et al. Laparoscopic ureterolithotomy as a primary modality for large proximal ureteral calculi: comparison to rigid ureteroscopic pneumatic lithotripsy. J Laparoendosc Adv Surg Tech A. 2011; 21:7–13.
11. Preminger GM, Assimos DG, Lingeman JE, Nakada SY, Pearle MS, Wolf JS Jr, et al. Chapter 1: AUA guideline on management of staghorn calculi: diagnosis and treatment recommendations. J Urol. 2005; 173:1991–2000.
12. Ramakumar S, Lancini V, Chan DY, Parsons JK, Kavoussi LR, Jarrett TW. Laparoscopic pyeloplasty with concomitant pyelolithotomy. J Urol. 2002; 167:1378–1380.
13. Gaur DD, Trivedi S, Prabhudesai MR, Gopichand M. Retroperitoneal laparoscopic pyelolithotomy for staghorn stones. J Laparoendosc Adv Surg Tech A. 2002; 12:299–303.
14. Sampaio FJ. Surgical anatomy of the kidney. In : Smith AD, Preminger G, Badlani G, Kavoussi L, editors. Smith's text book of endourology. St. Louis: Quality Medical;1996. p. 153–184.
15. Chatham JR, Dykes TE, Kennon WG, Schwartz BF. Effect of percutaneous nephrolithotomy on differential renal function as measured by mercaptoacetyl triglycine nuclear renography. Urology. 2002; 59:522–525.
16. Moskovitz B, Segev Y, Sopov V, Horev N, Groshar D, Nativ O. Does percutaneous nephrolithotripsy (PCNL) affect renal function: assessment with quantitative spect of Tc 99M-DMSA (QDMSA) renal scintigraphy. Harefuah. 2005; 144:626–629. 676677
17. Liou LS, Streem SB. Long-term renal functional effects of shock wave lithotripsy, percutaneous nephrolithotomy and combination therapy: a comparative study of patients with solitary kidney. J Urol. 2001; 166:36.
18. Kurien A, Baishya R, Mishra S, Ganpule A, Muthu V, Sabnis R, et al. The impact of percutaneous nephrolithotomy in patients with chronic kidney disease. J Endourol. 2009; 23:1403–1407.
19. El-Tabey NA, El-Nahas AR, Eraky I, Shoma AM, El-Assmy AM, Soliman SA, et al. Long-term functional outcome of percutaneous nephrolithotomy in solitary kidney. Urology. 2014; 83:1011–1015.
20. Sharifiaghdas F, Kashi AH, Eshratkhah R. Evaluating percutaneous nephrolithotomy-induced kidney damage by measuring urinary concentrations of β2-microglobulin. Urol J. 2011; 8:277–282.
21. Bayrak O, Seckiner I, Erturhan SM, Mizrak S, Erbagci A. Analysis of changes in the glomerular filtration rate as measured by the cockroft-gault formula in the early period after percutaneous nephrolithotomy. Korean J Urol. 2012; 53:552–555.
22. Demirtas A, Caniklioglu M, Kula M, Sofikerim M, Akınsal EC, Ergul MA, et al. Assessment of the effects of access count in percutaneous nephrolithotomy on renal functions by technetium-99m-dimercaptosuccinic Acid scintigraphy. ISRN Urol. 2013; 2013:827121.
23. Matsuura H, Hioki T, Sakurai M, Arima K, Yanagawa M, Sugimura Y, et al. Influence of extracorporeal shock wave lithotripsy (ESWL) on renal function assessed by 99mTc-DMSA scintigraphy: comparative analysis between ESWL and percutaneous nephroureterolithotripsy (PNL). Hinyokika Kiyo. 1994; 40:1061–1067.
24. Yasui T, Okada A, Hamamoto S, Taguchi K, Ando R, Mizuno K, et al. Efficacy of retroperitoneal laparoscopic ureterolithotomy for the treatment of large proximal ureteric stones and its impact on renal function. Springerplus. 2013; 2:600.
25. Wang X, Li S, Liu T, Guo Y, Yang Z. Laparoscopic pyelolithotomy compared to percutaneous nephrolithotomy as surgical management for large renal pelvic calculi: a meta-analysis. J Urol. 2013; 190:888–893.
26. Stein RJ, Turna B, Nguyen MM, Aron M, Hafron JM, Gill IS, et al. Laparoscopic pyeloplasty with concomitant pyelolithotomy: technique and outcomes. J Endourol. 2008; 22:1251–1255.
27. Nadu A, Schatloff O, Morag R, Ramon J, Winkler H. Laparoscopic surgery for renal stones: is it indicated in the modern endourology era? Int Braz J Urol. 2009; 35:9–17.
28. Gill IS, Grune MT, Munch LC. Access technique for retroperitoneoscopy. J Urol. 1996; 156:1120–1124.
29. Bove P, Micali S, Miano R, Mirabile G, De Stafani S, Botteri E, et al. Laparoscopic ureterolithotomy: a comparison between the transperitoneal and the retroperitoneal approach during the learning curve. J Endourol. 2009; 23:953–957.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download