Abstract
Here we describe two cases of papillary urothelial neoplasm of low malignant potential in adolescent boys. One case was a 16-year-old boy with a polypoid mass beside the right ureteral orifice and the other case was a 13-year-old boy with a papillary mass beside the left ureteral orifice. The initial presentation was hematuria in both cases and the bladder mass was detected by ultrasonography. Complete resection of the bladder tumor was performed by using an 11-Fr pediatric resectoscope. Follow-up has been performed with urine analysis, urine cytology, and bladder ultrasonography or cystoscopy every 3 months with no evidence of recurrence.
Bladder transitional cell carcinoma (TCC) is typically a disease of older individuals and is rarely found in the first two decades of life. Before 2010, 125 cases of bladder urothelial tumors were reported in patients younger than 20 years [1]. Meta-analysis revealed a very favorable outcome for these patients with relatively low rates of recurrence (3.4%), progression (1.1%), and death (1.1%) [1,2]. However, just as in adult patients, close follow-up is necessary in pediatric patients with bladder urothelial tumors to identify tumor recurrence. Unfortunately, there is no consensus on follow-up methods in pediatric patients owing to the low incidence and scarcity of reports in the literature. Here we present two case studies aimed at expanding the number of pediatric cases reported and discuss follow-up methods with a review of the literature.
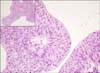
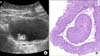
A 13-year-old boy presented with gross hematuria of 2 days' duration 4 months before surgery. The boy was otherwise healthy with no previous medical problems and thus the patient and his parents had ignored the symptom. The patient presented to the Emergency Department with right lower abdominal pain 5 days before surgery. Abdominal ultrasonography revealed acute appendicitis and a 2-cm-sized bladder mass (Fig. 1). He had no fever or loss of weight. The results of a complete blood count with differential were within normal limits. The results of an electrolyte battery, liver function, and renal function tests were within normal limits. The urine test revealed only hematuria, and urine cytology showed no evidence of malignancy. The patient's parents requested a computed tomography (CT) scan, which revealed a single bladder mass and no enlargement of the lymph nodes or metastasis to the abdomen or pelvis. Preoperative cystoscopy was not performed because the patient and his parents wished to schedule concomitant appendectomy and transurethral resection (TUR) of the bladder mass under general anesthesia. An 11-Fr pediatric resectoscope and TUR equipment (Karl Storz GmbH, Tuttlingen, Germany) were used for TUR of the bladder tumor. There was a 2-cm papillary mass with a stalk beside the left ureteral orifice (Fig. 2). Microscopic examination demonstrated round to oval shaped, uniformly enlarged nuclei; inconspicuous nucleoli; and rare mitosis (Fig. 3). The diagnosis was papillary urothelial neoplasm with low malignant potential (papillary TCC, TaG1 stage). Ultrasonography, urine analysis, and urine cytology were performed every 3 months after TUR of the bladder tumor. At present, 18 months after surgery, there has been no evidence of recurrence.
A 16-year-old boy presented with intermittent gross hematuria of 4 months' duration. The patient had stage 4 left neuroblastoma and had undergone left radical nephrectomy 7 years previously. He had also received adjuvant chemotherapy including cisplatin, etoposide, and cychlophosphamide. Five years prior, recurrence in the para-aortic lymph nodes was detected and radiation therapy was subsequently performed at the upper abdomen. At the time of presentation, there had been no evidence of tumor recurrence. The results of a complete blood count with differential were within normal limits. A urine test revealed only hematuria, and urine cytology showed no evidence of malignancy. Abdominal ultrasonography revealed a 1.2-cm bladder mass on the right posterior lateral wall (Fig. 4A). Abdominal CT revealed a single bladder mass and no lymph node enlargement or masses of other organs. Direct TUR of the bladder tumor was performed with the patient under general anesthesia. There was a 1.4-cm papillary mass with a stalk beside the right ureteral orifice. Microscopic examination demonstrated papillary urothelial neoplasm with low potential for malignancy (Fig. 4B). Urine analysis, cystoscopy with local anesthesia, and washed urine cytology were performed every 3 months after TUR of the bladder tumor. At present, 12 months after surgery, there has been no evidence of recurrence.
The most common symptom of bladder urothelial tumors in children is gross hematuria [3]. A urothelial tumor in the bladder is typically located in the trigone or ureteric orifices and the lateral bladder wall [1,4]. The vast majority of bladder urothelial tumors are solitary tumors (94%). In our case studies, the first symptom was also gross hematuria, and a solitary tumor was located beside the ureteral orifice. A delay in the diagnosis of bladder urothelial neoplasms seems to be common in younger patients, probably because of the relative rarity of this diagnosis and the predominance of benign causes of hematuria in this age group.
Bladder urothelial tumors in the first two decades of life are distinctly unusual, with most described in case reports and small series [5,6]. Recently, some review articles have described the clinicopathologic characteristics of pediatric bladder TCC [1,2]. In this age group, these tumors appear to exhibit unique clinicopathologic features, with preferentially low-grade morphology and decreased likelihood of recurrence and progression, although some debate exists regarding their biological behavior. Papillary urothelial neoplasm of low malignant potential (PUNLMP) was introduced in the World Health Organization/1998 International Society of Urologic Pathology grading system and is one of the most controversial aspects of this grading system [7]. PUNLMP is frequent among bladder urothelial tumors of young patients, particularly in the teenage years; it may have a low rate of progression to higher grade and stage and thus differs from papillary urothelial carcinoma [1]. The short follow-up period of our cases (12 and 18 months) might be a limitation in a discussion of the recurrence of adolescent bladder tumors. However, considering the high recurrence rate of adult bladder tumors, two of all our cases did not experience tumor recurrence during follow-up.
Although TUR is the treatment of choice for papillary urothelial tumors, the nature of recurrent disease and the best follow-up methods in these young patients after TUR procedures are under debate [8]. Surveillance methods for pediatric patients with bladder urothelial tumors have rarely been described in the literature. We performed ultrasonography and urine analysis and cytology tests every 3 months for the 13-year-old boy and cystoscopy and urine tests for the 16-year-old boy. The results of these tests have been within normal limits.
In a small contemporary series, ultrasonography was extremely effective in identifying bladder tumors, and the authors argued for its use in initial diagnosis and disease surveillance [3]. As the technology and image quality of ultrasonography has advanced, it has become more sensitive in identifying bladder urothelial tumors in pediatric patients. Ultrasonography is noninvasive and is not associated with a radiation hazard, thus providing benefits for the periodic surveillance of young patients after TUR. However, the accuracy of ultrasound concerning bladder tumor follow-up has not yet been proven. Intravenous urography was found to have a sensitivity of 44% in identifying a bladder mass in patients younger than 40 with urothelial carcinoma [9]. It is also more difficult to detect a small bladder mass by intravenous urography compared with ultrasonography. Whereas only cystoscopy allows for definitive diagnosis, the need for general anesthesia in young patients and the risks of urethral manipulation make its limited use preferable, especially in repeated periodic examinations. Routine cystoscopy might be changed to other diagnostic methods to screen for the recurrence of bladder tumors owing to the low recurrence and indolent features of bladder urothelial neoplasm in children. CT is an accurate imaging modality for the detection of bladder cancer in patients at risk for the disease. However, radiation exposure has to be balanced against the disease likelihood in younger patients. Urine cytology has not been a useful diagnostic tool in young patients mainly because of the predominance of low-grade lesions resulting in a low sensitivity rate. Thus, urine cytology alone is not recommended for diagnosis and follow-up [4].
There is no standard surveillance protocol for young patients with a urothelial tumor. Although rare, some recurrences and deaths have been reported [10]. Clinicians must remember that young patients should be periodically screened for recurrence of bladder urothelial tumors to ensure the timely identification of recurrence or metastasis. For follow-up methods, we suggest the combination of noninvasive diagnostic method such as ultrasonography, urinalysis, and cytology as diagnostic and surveillance tools for bladder urothelial tumors in younger children. If the pediatric patients can tolerate it, periodic cystoscopy may be recommended, as for adult patients, because of its standard use as a surveillance tool.
Figures and Tables
 | FIG. 1Ultrasonograph of case 1. Markers indicate the presence of a urothelial tumor on the posterior bladder wall. |
 | FIG. 2Endoscopic view of a urothelial tumor in a 13-year-old boy (case 1). Transurethral resection (A, C) was performed with an 11-Fr pediatric resctoscope and TUR equipment (Karl Storz GmbH, Tuttlingen, Germany). Deep biopsy was performed (B). Resected bladder tumor (D). |
References
1. Paner GP, Zehnder P, Amin AM, Husain AN, Desai MM. Urothelial neoplasms of the urinary bladder occurring in young adult and pediatric patients: a comprehensive review of literature with implications for patient management. Adv Anat Pathol. 2011; 18:79–89.
2. Williamson SR, Lopez-Beltran A, MacLennan GT, Montironi R, Cheng L. Unique clinicopathologic and molecular characteristics of urinary bladder tumors in children and young adults. Urol Oncol. 2013; 31:414–426.
3. Hoenig DM, McRae S, Chen SC, Diamond DA, Rabinowitz R, Caldamone AA. Transitional cell carcinoma of the bladder in the pediatric patient. J Urol. 1996; 156:203–205.
4. Lerena J, Krauel L, Garcia-Aparicio L, Vallasciani S, Sunol M, Rodo J. Transitional cell carcinoma of the bladder in children and adolescents: six-case series and review of the literature. J Pediatr Urol. 2010; 6:481–485.
5. McGuire EJ, Weiss RM, Baskin AM. Neoplasms of transitional cell origin in first twenty years of life. Urology. 1973; 1:57–59.
6. Patel R, Tery T, Ninan GK. Transitional cell carcinoma of the bladder in first decade of life. Pediatr Surg Int. 2008; 24:1265–1268.
7. Epstein JI, Amin MB, Reuter VR, Mostofi FK. Bladder Consensus Conference Committee. The World Health Organization/International Society of Urological Pathology consensus classification of urothelial (transitional cell) neoplasms of the urinary bladder. Am J Surg Pathol. 1998; 22:1435–1448.
8. Fine SW, Humphrey PA, Dehner LP, Amin MB, Epstein JI. Urothelial neoplasms in patients 20 years or younger: a clinicopathological analysis using the world health organization 2004 bladder consensus classification. J Urol. 2005; 174:1976–1980.
9. Kurz KR, Pitts WR, Vaughan ED Jr. The natural history of patients less than 40 years old with bladder tumors. J Urol. 1987; 137:395–397.
10. Madgar I, Goldwasser B, Nativ O, Hanani Y, Jonas P. Long-term followup of patients less than 30 years old with transitional cell carcinoma of bladder. J Urol. 1988; 139:933–934.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download