Abstract
Purpose
Prostate cancer is rare in men younger than 50 years. Digital rectal examination (DRE) and measurement of prostate-specific antigen (PSA) concentrations are standard screening methods for detecting prostate cancer. We retrospectively investigated the risks and benefits of repeated transrectal ultrasonography-guided prostate needle biopsies in relation to the follow-up status of men younger than 50 years with a consistently high PSA concentration (>3.0 ng/mL).
Materials and Methods
During the period from January 2000 through February 2013, we reviewed patient's ages, dates of procedures, DRE results, frequencies of biopsies, results of the biopsies, periods of follow-up, PSA concentrations, and prostate volumes in Chonbuk National University Hospital records. We conducted telephone interviews in patients who did not undergo regular follow-up.
Results
The mean age of the patients was 44.7 years, and the mean PSA concentration was 8.59 ng/mL (range, 3.04-131 ng/mL) before biopsy. The PSA concentration was significantly different (p<0.001) between the patients with prostate cancer and those with benign prostatic hyperplasia (BPH). Nineteen patients underwent repeated prostate biopsy; however, in only one patient did the pathologic findings indicate a change from BPH to prostate cancer. We identified several complications after transrectal biopsy through an evaluation of follow-up data.
Conclusions
All patients with benign prostatic disease based on their first biopsy were shown to have benign disease based on all repeated biopsies (15.83%), except for one patient; however, several complications were noted after biopsy. Therefore, the risks and benefits of repeated biopsy in young patients should be considered because of the low rate of change from benign to malignant disease despite continuously high PSA concentrations (>3.0 ng/mL).
Although controversial, prostate-specific antigen (PSA) screening is generally considered to be essential for detecting prostate cancer and is commonly used as a screening method to detect prostate cancer [1]. However, the specificity of this method is limited because an elevated serum PSA concentration can be significantly elevated in association with benign prostatic conditions, such as benign prostatic hyperplasia (BPH), prostatitis, and urinary tract manipulations (e.g,. prostatic massage, transrectal prostate needle biopsy, transurethral resection of the prostate, digital rectal examination (DRE), transrectal ultrasonography, cystoscopy, and ejaculation) [2].
Ku et al. [3] reported that the median serum PSA concentration (5th-95th percentile range) is 0.90 ng/mL (range, 0.33-2.25 ng/mL) for men 20-29 years old, 0.89 ng/mL (range, 0.30-2.35 ng/mL) for men 30-39 years old, and 0.89 ng/mL (range, 0.30-2.36 ng/mL) for men 40-49 years old. The concentration of PSA in patients younger than 50 years was significantly lower than that in older patients. In another study, Sun et al. [4] reported that the frequency of prostate cancer is 4.4% in patients younger than 50 years and is 14.2% in patients older than 50 years. Even though much research has been conducted on prostate cancer detection rates and PSA concentration cutoffs in biopsy samples, little research on the efficacy of repeated biopsy in patients with benign results on initial biopsy has been conducted.
Thus, the objective of this study was to retrospectively investigate the efficacy of repeated transrectal ultrasonography-guided prostate needle biopsy based on the biopsy results and follow-up status of men younger than 50 years with a consistently high PSA concentration (>3.0 ng/mL).
This retrospective study was conducted at the Department of Urology in Chonbuk National University Hospital between January 2000 and February 2013. The study population consisted of 120 patients younger than 50 years who underwent transrectal prostate needle biopsy because of an elevated PSA concentration (>3.0 ng/mL). The ages of the patients, dates of procedures, numbers of biopsies, DRE results, periods of repeated biopsy, pathologic findings, periods of follow-up, concentrations of PSA, and prostate volumes were reviewed. We basically checked the PSA concentrations of patient who had less serious urinary symptoms.
All transrectal prostate biopsies were guided by ultrasonography (Type 2202, BK medical, Herlev, Denmark; in two-dimensional planes [sagittal and axial]). Twelve or 17 cores were obtained, and the pathologic findings were divided into four categories: BPH, prostatitis, atypical prostatic glands, and prostate cancer. The atypical prostatic glands included high-grade prostate intraepithelial neoplasia, atypical small acinar proliferation, and other benign reactive changes.
In patients with a benign result, we measured PSA concentrations at 1, 3, and 6 months and then every 6 months or 1 year. We performed a repeated transrectal prostate biopsy in patients with a PSA concentration >3.0 ng/mL or a biopsy finding of atypical prostatic gland.
We reviewed the medical records of all patients who underwent continuous follow-up at our hospital and conducted a short telephone interview in those patients who did not undergo regular follow-up for more than 6 months. A structured telephone interview was conducted in each patient regardless of whether they underwent regular follow-up for their prostatic disease. The patients were asked whether they underwent clinical follow-up for their prostatic disease, whether they had their PSA concentration checked regularly, and whether they received a repeated biopsy. Patients who did not undergo regular follow-up for their prostatic disease were provided four answers to choose from to explain why. The answers to these questions were provided by the patient or one of their family members.
The statistical analysis was performed by using IBM SPSS ver. 20.0 (IBM Co., Armonk, NY, USA). Chi-square tests were used to compare biopsy results and follow-up status. Patients with a biopsy finding of atypical prostatic gland were added to the malignancy group. Logistic regression analysis was used to check the relation between initial PSA values and follow-up status. Statistical significance was set at p<0.05.
A total of 120 patients were enrolled in our study. The mean follow-up period for 120 patients was 1,027.89 days (range, 7-4,563 days), the mean age was 44.7 years (range, 29-50 years), and the mean PSA concentration was 9.23 ng/mL (range, 3.12-131 ng/mL) at baseline (Table 1). The average number of biopsies was 1.23 (range, 1-7), the mean number of repeated biopsies was 2.47, and 19 men underwent repeated biopsy (14 patients underwent 2 biopsies, 4 underwent 3 biopsies, and 1 underwent 7 biopsies). In only one patient did the pathologic finding by repeated biopsy (third repeated biopsy in 2006) indicate a change from BPH to prostate cancer; this patient did not undergone regular follow-up, which was confirmed by telephone interview.
The result was that 88 of 120 men (73.3%) had benign prostatic tissue, 11 men (9.2%) had prostatitis, 7 men (5.8%) had atypical prostatic gland, 1 man (0.8%) had sclerosing adenosis, and 13 men (10.8%) had prostate cancer. The repeated biopsy results were nearly the same in the BPH and prostatitis groups, but four patients with BPH were reclassified with atypical prostatic gland.
Before the prostatic biopsy, the mean (±standard deviation) PSA concentrations in patients with BPH, prostatitis, atypical prostatic gland, and prostate cancer were 7.48±7.70, 10.32±7.01, 6.81±2.25, and 24.77±34.12 ng/mL, respectively. A comparison of PSA concentrations between the cancer and noncancer groups showed a significant differences (p<0.001), but no statistically significant difference was found between the prostatitis and prostate (p=0.76) cancer groups.
Abnormalities in DRE and biopsy results were closely correlated with the detection of prostate cancer. Five men (5%) had BPH, 0 had prostatitis, 1 (14%) had atypical prostatic glands, and 6 (46%) had prostate cancer. Thus, we confirmed a close relation between abnormalities in DRE results and prostate cancer.
We identified follow-up status in 45 of 120 patients by telephone interview and in 40 patients by review of medical records, but the follow-up status of the remaining 35 patients could not be confirmed because their addresses or phone numbers had changed. When we questioned the patients about their follow-up status by telephone interview, we found that 39 of 64 patients (60.9%) with BPH, 3 of 6 patients (50%) with prostatitis, 4 of 4 patients (100%) with atypical prostatic gland, and 10 of 10 patients (100%) with prostate cancer had undergone regular follow-up. We identified the follow-up status of 17 of 19 patients who received repeated biopsies.
All patients who underwent regular follow-up (confirmed by telephone interview or from medical records) had their PSA concentrations measured regularly at a local clinic, but we were unable to clearly identify the timing of these measurements. Furthermore, none of the repeated biopsies were done at other hospitals; therefore, we believe that these patients probably did not have high PSA concentrations. The remaining patients who underwent regular follow-up had a diagnosis of sclerosing adenosis. When we divided the patients into a benign group and a malignancy group, the rate of follow-up loss was higher in the former than in the latter group (p<0.001) (Table 2).
We found various reasons for follow-up loss. Of the 30 patients lost to follow-up, 3 (10%) did not receive follow-up because of side effects such as persistent hemospermia, severe pain, or discomfort after transrectal prostate needle biopsy. Fifteen (12.5%) who visited the hospital regularly experienced complications, 7 of whom were treated at a local clinic or at our hospital and 1 of whom received special therapy in the Department of Anesthesiology because of severe pain.
Loeb et al. [5] reported that the median PSA concentration in the general male population ranged from 0.4 to 0.7 ng/mL in men in their 40s and from 0.7 to 1.0 ng/mL in men in their 50s. The baseline PSA concentration at a young age is an important predictor of a later prostate cancer diagnosis and disease-specific outcomes. Thus, baseline PSA measurement can be used for risk stratification and to guide screening protocols.
We can detect prostate cancer early by the reviewing a young man's PSA concentration and biopsy results. Reducing the mortality rate associated with prostate cancer is dependent on early detection and prevention, because metastatic prostate cancer is difficult to treat. The most effective treatment strategy in prostate cancer is early detection.
Smith and Catalona [6] showed that most tumors detected through PSA screening are clinically important. Clinically important prostate cancer suggests that the treatment of these tumors will directly affect either the quality or length of the patient's life. Sun et al. [4] suggested three main reasons why the screening cutoff for PSA should be lower in men aged <50 years. First, the incidence of BPH is lower in younger men than in older men [7]. Second, prostate cancer that is detected early in younger men is more curable, as mentioned earlier for clinically localized cancer. Finally, younger men rarely have important medical comorbidities and can opt for definitive treatments such as surgery [8].
However, there is no clear protocol for PSA screening by age in Korea. The American Cancer Society recommends performing a prostate needle biopsy and PSA screening, on the basis of risks and benefits, at age 50 years in those with an average risk and at 40 years in those with a high risk (African Americans or those with a family history). The American Cancer Society's standard recommended PSA concentration cutoffs, from prostate biopsy, are 0.6 ng/mL at <40 years of age and 2.5 ng/mL at <60 years of age [9]. The National Comprehensive Cancer Network guidelines recommended beginning the risk-benefit discussion and offer baseline DRE and PSA screening at 40 years of age [10]. We comply with these foreign standards in our clinics.
Ku et al. [3] reported that, in healthy Korean men, the median serum PSA concentration (5th-95th percentile) is 0.90 ng/mL (range, 0.33-2.25 ng/mL) for men 20-29 years of age, 0.89 ng/mL (range, 0.30-2.35 ng/mL) for men 30-39 years of age, and 0.89 ng/mL (range, 0.30-2.36 ng/mL) for men 40 to 49 years of age. PSA concentrations in Korean men younger than 50 years were higher but those for men 50 years of age or older were lower than in other races.
In line with previously proposed guidelines for the evaluation of prostate cancer risk in young men, Oesterling et al. [11] considered the risk of prostate cancer relative to race. They suggested age-specific PSA thresholds for men in their 40s of 2.5 ng/mL for whites and 2.0 ng/mL for African Americans, and the recommended reference range for age-specific serum PSA (95th percentile) for men aged 40-49 years is 0-2.5 ng/mL.
As previously mentioned, early detection of prostate cancer is important. However, studies of PSA concentrations in young men in Korea and Asia are rare, and there is no reference range for age-specific serum PSA concentrations and no guidelines for transrectal prostate needle biopsy in young men. Clear guidelines for PSA values relative to prostate cancer risk do not exist for patients younger than 50 years in Asian countries, including Korea. Studies are needed to confirm risk factors for young Korean men in relation to biopsy findings and elevations in PSA, as in western countries. We currently recommend a PSA cutoff of >3.0 ng/mL (biopsy) for men younger than 50 years, because PSA level increase as patients age.
Other factors associated with elevations in PSA at a young age are high body mass index (BMI) and obesity. A higher BMI is positively associated with a diagnosis of prostate cancer. Also, in men with cancer, a higher BMI increases the odds of high-grade disease [12]. In addition, obesity is related to prostate cancer because prostate cancer is hormonally based [13].
Our research indicates a correlation between abnormal DRE results and risk of prostate cancer at a young age. We identified 5 patients (>50%) with abnormal DRE results who had cancer. This finding contrasts with the results of Ruska et al. [14], who studied 87 men younger than 40 years of age who underwent prostate needle biopsy. The most common indications for biopsy were abnormal DRE results (n=61), elevated PSA concentrations (n=14), and inflammatory symptoms (n=12); 23 cases of cancer were detected. However, an abnormal DRE result was not predictive of cancer.
In our study, all patients with benign prostatic disease based on the first biopsy were shown to have benign disease based on all repeated biopsies, except for one patient. This finding was similar to that of Yang et al. [15]. The median age of the 75 men in their study was 33 years (range, 26-40 years). The results of the primary biopsy were as follows: 1 case (1.3%) of prostate cancer, 70 cases (93%) of benign tissue, 2 cases (2.6%) of inflammation, and 1 case (1.3%) each of high-grade intraepithelial neoplasia and atypical small acinar proliferation. All of the 10 men who underwent a second biopsy, and three of the men who underwent a third biopsy, had benign results. The results of all repeated transrectal needle prostate biopsies in that study were benign; therefore, the usefulness of repeated biopsy in men younger than 40 years should be evaluated on the basis of risks and benefits (e.g., invasiveness, pain, and high cost).
In line with previous research on follow-up status and risk of prostate cancer, 3 men (10%) lost to follow-up in the current study experienced pain, hematuria, or hemospermia after biopsy, and complications were also experienced by some of the patients not lost to follow-up. These patients often required hospitalization and/or special therapy.
The mean PSA values differed between the prostatitis group and the prostate cancer group, but not significantly so; the standard deviation in the prostate cancer group may have been too wide. Kim et al. [16] showed that the mean PSA concentration decreased significantly after 4 weeks of treatment with antibiotics and nonsteroidal anti-inflammatory agents. A relatively high rate of cancer (13.5%, 5/37) was detected in patients with a PSA value that decreased to a normal value (<4 ng/mL) after treatment. Their results suggest a strong correlation between prostate inflammation and neoplastic transformation, although others refute this correlation [17, 18, 19, 20].
The main cause of follow-up loss was the lack of symptoms affecting quality of life. However, symptoms are rare in early-stage prostate cancer. The presence of symptoms usually suggests locally advanced or metastatic disease. Therefore, patients should undergo continuous follow-up even if they have no symptoms. The patients' attitudes about prostatic disease differed based on their biopsy results; most patients with a benign result tended to not think too seriously about the disease. Many patients were lost to follow-up after their first biopsy for this reason.
Our study had several limitations. First, there was a wide range of atypical prostatic gland types-not only high-grade intraepithelial neoplasia and atypical small acinar proliferation but benign reactive changes that could not be confirmed as either prostate cancer or BPH by pathologic review. Second, there is no definitive established follow-up protocol for when to perform a repeated biopsy. Third, the transrectal biopsies and ultrasonographies were not performed by one urologist. In addition, a larger sample size of patients would have resulted in more accurate results. The number of patients in our study (n=120) was too small to draw a definitive conclusion, and there was large deviation in the time periods for repeated biopsies. These limitations decreased the confidence of our data; however, the results are plausible given that the patients were younger than 50 years of age.
Our study was conducted to determine the efficacy of repeated biopsy at detecting prostate cancer in young patients (<50 years) with a high PSA concentration over a period of approximately10 years at a single hospital. Even though we conducted telephone interviews to determine the follow-up status of the patients, our data were insufficiently clear. It can bring a information or clue about patient who received repeated biopsy at young age.
The incidence of malignant disease being detected in patients with a previous benign biopsy result was very low in our study; only one case was detected in 19 of 120 patients who underwent repeated transrectal prostate needle biopsies. Thus, the risks and benefits of repeated biopsy in men younger than 50 years with high PSA concentrations should be considered carefully because of the possible complications associated with this procedure and because of the low malignancy change rate in this population. As this patient population ages, continuous follow-up is recommended, as is repeated transrectal prostate biopsy if warranted. Furthermore, the risk factors associated with elevated PSA concentrations in young men should be evaluated.
Figures and Tables
TABLE 1
Characteristic of patients younger than 50 years old with high prostate-specific antigen (PSA) concentrations (>3.0 ng/mL)
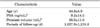
TABLE 2
Distribution of the repeated prostatic biopsies and observation in the patient population

The number of parenthesis represent the man's number of repeated biopsy.
TR-Bx, transrectal prostate needle biopsy; BPH, benign prostate hyperplasia.
a:Atypical prostatic gland includes high grade intraepithelial neoplasia, atypical small acinar proliferation and other reactive changes, excludes BPH, prostatitis and prostate cancer. b:Sclerosing adenosis. c:The patient of prostate cancer that he was BPH in previous prostate biopsy. d:Cannot connected by telephone.
ACKNOWLEDGEMENT
This study was supported by grants from the Korea Healthcare Technology R&D Project, Ministry for Health, Welfare & Family Affairs, Republic of Korea (HI13C0104).
References
1. Barry MJ. Screening for prostate cancer: the controversy that refuses to die. N Engl J Med. 2009; 360:1351–1354.
2. Klein LT, Lowe FC. The effects of prostatic manipulation on prostate-specific antigen levels. Urol Clin North Am. 1997; 24:293–297.
3. Ku JH, Ahn JO, Lee CH, Lee NK, Park YH, Byun SS, et al. Distribution of serum prostate-specific antigen in healthy Korean men: influence of ethnicity. Urology. 2002; 60:475–479.
4. Sun L, Moul JW, Hotaling JM, Rampersaud E, Dahm P, Robertson C, et al. Prostate-specific antigen (PSA) and PSA velocity for prostate cancer detection in men aged <50 years. BJU Int. 2007; 99:753–757.
5. Loeb S, Carter HB, Catalona WJ, Moul JW, Schroder FH. Baseline prostate-specific antigen testing at a young age. Eur Urol. 2012; 61:1–7.
6. Smith DS, Catalona WJ. The nature of prostate cancer detected through prostate specific antigen based screening. J Urol. 1994; 152(5 Pt 2):1732–1736.
7. Denmeade SR, Isaacs JT. The role of prostate-specific antigen in the clinical evaluation of prostatic disease. BJU Int. 2004; 93:Suppl 1. 10–15.
8. Vickers AJ, Lilja H. Predicting prostate cancer many years before diagnosis: how and why? World J Urol. 2012; 30:131–135.
9. American Cancer Society. American Cancer Society recommendations for prostate cancer early detection [Internet]. Atlanta: American Cancer Society;2012. cited 2012 May 10. Available from: http://www.cancer.org/aboutus/howwehelpyou/contactus/index.
10. National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology (NCCN Guidelines): prostate cancer. ver. 3. 2012 [internet]. Fort Wathington: NCCN;c2012. cited 2012 Apr 25. Available from: http://www.nccn.org/professionals/physician_gls/pdf/prostate_detection.pdf.
11. Oesterling JE, Jacobsen SJ, Chute CG, Guess HA, Girman CJ, Panser LA, et al. Serum prostate-specific antigen in a community-based population of healthy men. Establishment of age-specific reference ranges. JAMA. 1993; 270:860–864.
12. Freedland SJ, Terris MK, Platz EA, Presti JC Jr. Body mass index as a predictor of prostate cancer: development versus detection on biopsy. Urology. 2005; 66:108–113.
13. Bray GA. The underlying basis for obesity: relationship to cancer. J Nutr. 2002; 132:11 Suppl. 3451S–3455S.
14. Ruska KM, Partin AW, Epstein JI, Kahane H. Adenocarcinoma of the prostate in men younger than 40 years of age: diagnosis and treatment with emphasis on radical prostatectomy findings. Urology. 1999; 53:1179–1183.
15. Yang JB, Jeong BC, Seo SI, Jeon SS, Choi HY, Lee HM. Outcome of prostate biopsy in men younger than 40 years of age with high prostate-specific antigen (PSA) levels. Korean J Urol. 2010; 51:21–24.
16. Kim YJ, Kim SO, Ryu KH, Hwang IS, Hwang EC, Oh KJ, et al. Prostate cancer can be detected even in patients with decreased PSA less than 2.5 ng/ml after treatment of chronic prostatitis. Korean J Urol. 2011; 52:457–460.
17. Nelson WG, De Marzo AM, Isaacs WB. Prostate cancer. N Engl J Med. 2003; 349:366–381.
18. Palapattu GS, Sutcliffe S, Bastian PJ, Platz EA, De Marzo AM, Isaacs WB, et al. Prostate carcinogenesis and inflammation: emerging insights. Carcinogenesis. 2005; 26:1170–1181.
19. Postma R, Schroder FH, van der Kwast TH. Atrophy in prostate needle biopsy cores and its relationship to prostate cancer incidence in screened men. Urology. 2005; 65:745–749.
20. Anton RC, Kattan MW, Chakraborty S, Wheeler TM. Postatrophic hyperplasia of the prostate: lack of association with prostate cancer. Am J Surg Pathol. 1999; 23:932–936.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download