Abstract
Purpose
We investigated the efficacy of transurethral injection of Macroplastique bulking agent (Uroplasty) for male stress urinary incontinence (SUI) after prostate surgery.
Materials and Methods
This retrospective review included men with SUI treated by transurethral injection for symptoms resulting from prostate surgery. Patients were evaluated at 1 month and 6 months after injection by determining the number of pads used per day and changes in incontinence symptoms. Treatment success was defined as use of 1 pad or fewer per day combined with subjective symptom improvement.
Results
The study population comprised 30 men with a mean age of 66.1±5.3 years. Of the 30 patients, 24 (80.0%) underwent prostate cancer surgery and the remaining 6 (20.0%) underwent surgery for benign prostatic hyperplasia. The preinjection pad number was 2.9±1.9 pads per day. After injection treatment, the mean follow-up period was 9.3±12.7 months and the success rate was 43% (13/30) at 1 month and 32% (6/19) at 6 months. Injection was more likely to result in a successful outcome in patients with no preinjection radiation treatment history and higher abdominal leak point pressure (ALPP) than in those with a previous history of radiation treatment and lower ALPP, although this result was not statistically significant. Acute urinary retention occurred in 5 patients (17%).
In recent years, the incidence of prostate cancer has increased rapidly, and prostate cancer is now the fifth most common type of malignancy among Korean men [1]. Increased screening for prostate-specific antigen during health check-ups has contributed to increased detection of early prostate cancer, and the number of radical prostatectomies has increased correspondingly. In the case of benign prostatic hyperplasia (BPH), patients with lower urinary tract symptoms often report that their symptoms reduce quality of life. Thus, the number of BPH surgeries is also on the rise.
Male stress urinary incontinence (SUI) is one of the complications of prostate surgery. The first treatment approach for this condition is conservative management, which involves behavioral modifications, pelvic floor muscle training, and biofeedback. If conservative treatment fails, surgical treatment, including injection, male sling surgery, or creation of an artificial urinary sphincter (AUS) can be considered. Compared with other types of surgery, bulking agent injection therapy is less invasive, requires no skin incision, and can be converted to another type of incontinence surgery if necessary [2].
In this study, we describe our surgical experience with transurethral injection treatment of Macroplastique bulking agent (Uroplasty, Minnetonka, MN, USA) for male SUI after prostate surgery. We investigated the efficacy of transurethral Macroplastique injection for male SUI after prostate surgery, and we determined the factors that affected outcomes.
This retrospective review included men with SUI treated by transurethral injection of Macroplastique bulking agent from March 2006 to November 2012 at Samsung Medical Center. All SUI symptoms had occurred as complications of surgery for prostate disease. A urodynamic study was performed in all patients before injection treatment, and all procedures were performed by a single experienced surgeon (K.S.L.). A retrospective medical record review and telephone interview were performed to obtain the following clinical data: age at injection treatment, type of previous prostate surgery, preinjection radiation treatment history, time interval between prostate surgery and injection treatment, number of preinjection pads per day, abdominal leak point pressure (ALPP), detrusor overactivity (DO) on preinjection urodynamic study, and injected volume. Treatment outcomes after injection were evaluated at postoperative 1 month and 6 months. We analyzed factors affecting treatment success. Complications associated with injection treatment were also recorded.
Injection procedures were performed in the lithotomy position by using intraurethral lidocaine jelly injection. A 0-degree 24-Fr urethroscope was used. A syringe containing 2.5 mL of Macroplastique was attached to a 5-Fr injection catheter with a 20-gauge needle. The bulking agent was delivered to the 3, 6, 9, and 12 o'clock points of the urethra in the proximal position of the remnant urethral sphincter, creating a bleb under the urethral mucosa that protruded into the urethral lumen. Special care was taken to not inject the material into the external urethral sphincter because this can produce pudendal nerve irritation, resulting in sphincter spasm and discomfort. After injection, the urethral lumen was confirmed to be coaptated (Fig. 1). When proper coaptation was achieved, residual urine was evacuated with a thin urethral catheter to avoid displacement of the implant. Patients were discharged after successful voiding without significant residual urine (≤100 mL).
Patients were evaluated at 1 month and at 6 months after injection treatment by determining the number of pads used per day (objective parameter) and improvement in incontinence symptoms from before to after injection according to the Sandvik severity index (SSI) [3] and the benefit, satisfaction, and willingness to continue questionnaire [4] (subjective parameters). Dryness was defined as no wetting. Improvement was defined as use of one or fewer postinjection pads per day. Success was defined as dryness or subjective symptom improvement.
Statistical analyses were performed with PASW ver. 18.0 (SPSS Inc., Chicago, IL, USA). Chi-square tests were used to compare pre- and postoperative changes in the SSI score and factors affecting the outcomes of transurethral injection treatment. A p-value of less than 0.05 was considered statistically significant.
The study population comprised 30 men with a mean age of 66.1±5.3 years (range, 55-79 years). Of the 30 patients, 24 (80.0%) had undergone previous prostate cancer surgery (12 laparoscopic robot-assisted radical prostatectomies, 8 radical retropubic prostatectomies, 3 radical perineal prostatectomies, and 1 high-intensity focused ultrasound treatment), whereas the remaining 6 (20.0%) had undergone previous BPH surgery (3 holmium laser enucleations of the prostate, 2 transurethral resections of the prostate [TURP], and 1 photoselective vaporization of the prostate) (Table 1). Four patients (13.4%) had a history of radiation therapy for prostate cancer treatment. The mean preinjection number of pads was 2.9±1.9 pads per day. On the basis of the urodynamic findings, the mean preinjection ALPP was 109.7±41.9 cm H2O. The ALPP was less than 80 cm H2O in eight patients (26.7%). DO was observed in eight patients (26.7%). The mean time interval between prostate surgery and injection treatment was 35.8±25.2 months (range, 9-108 months). The mean injection volume was 5.3±2.1 mL, and no intraoperative complications occurred.
The mean follow-up duration after injection treatment was 9.3±12.7 months (range, 1-63 months) and 19 patients had follow-up periods longer than 6 months. The mean pad number at follow-up was 1.7±1.7 pads per day. Thirteen patients (43%) were successfully treated at 1 month, consisting of 3 patients (10.0%) with dryness and 10 patients (33.3%) with improvement. Of them, five patients had follow-up times shorter than 6 months and two patients showed recurrence of incontinence symptoms. Six of 19 patients (32%) were successfully treated at 6 months, consisting of 1 patient (5.3%) with dryness and 5 patients (26.3%) with improvement.
Table 2 summarizes the changes in pre- and post-injection SSI score at the 1-month time point, which consists of four levels of severity. The number of patients who had a severe (8-9 points) or very severe (12 points) symptom score was 27 (90.0%) before injection and 14 (46.7%) after injection. However, this change was not statistically significant (p=0.361) (Table 2). Fifteen patients (50%) benefited from the treatment, whereas 13 patients (43%) reported some benefit. Fifteen patients (50%) were satisfied with the treatment and only five patients (17%) were "very dissatisfied" with the treatment (Fig. 2).
Univariate analysis of several factors at the 1-month time point revealed that patients who had no previous history of radiation treatment or a higher ALPP were more likely to experience successful injection treatment. However, this relationship was not statistically significant, nor was there any statistically significant relationship between success and any of the other factors evaluated (Table 3).
Acute urinary retention (AUR) occurred in five patients (17%) as a complication of surgery. Two patients with AUR were treated by suprapubic catheter insertion. One patient kept the catheter for 1 month and the other the others kept catheter for 2 days. The remaining three AUR patients were treated by clean intermittent catheterization (CIC). One patient underwent CIC for 1 day and two patients underwent CIC for 2 days. One of the patients who underwent CIC for 2 days had a persistent weak stream. Therefore, after 6 months, we performed a urethroscopic examination of this patient. No abnormal narrowing or strictures were found; this patient is being closely observed.
The incidence of SUI after radical prostatectomy has been reported to range from 8% to 47% [5,6], whereas the incidence of SUI after TURP has been reported to be 0.5% [7]. The mechanism for male SUI after prostate surgery appears to be internal sphincter deficiency. The probable mechanism for internal sphincter deficiency after prostate surgery includes rhabdo-sphincter injury during apical dissection, large and deep sutures during vesico-urethral anastomosis, or injury of the neurovascular bundles.
Urinary incontinence causes problems, such as poor hygiene and loss of self-confidence, that directly affect the quality of life of patients. When conservative treatment fails, surgical treatment should be considered. AUS is considered the gold standard treatment for male SUI, with a success rate ranging from 59% to 90% [8,9] and a patient satisfaction rate of 76% [8]. However, the revision rate for AUS is relatively high (20% to 29%) owing to infection, urethral erosion, and mechanical failure [8,9]. Compared with AUS, a male sling operation has several advantages, including the absence of mechanical problems, no need for device training, immediate efficacy, and an overall reduced revision rate. The success rate of a male sling operation ranges from 54% to 83% [10,11]. However, urinary retention, erosion, infection, system dislocation, and persistent pain are possible complications of a male sling operation, whereas technical difficulty is another problem in patients who have undergone radical pelvic surgery [12]. Compared with other surgical treatments, bulking agent injection is less invasive but has a lower success rate, and multiple injections are usually needed to maintain continence [2]. The therapeutic mechanism of bulking agent injection therapy in male SUI patients is urethral sphincter obstruction or the sealing effect afforded by the bulking agent. Histologically, the bladder neck and posterior urethra consist of four layers, namely the mucosa, lamina propria, muscle layer, and adventitia. Of the four layers, the lamina propria has the potential space for bulging. If the bulking agent is inserted into the lamina propria, dissecting and urethral bulging between the mucosa and muscle layer can occur and result in sealing [12].
A variety of bulking agents have been used to treat male SUI. Polytetrafluoroethylene (Teflon) was widely used in the past, but was shown to cause several problems, including urethral irritation and perineal discomfort; small particle migration to the regional lymph nodes, lungs, and brain; and in animal experiments, polytetrafluoroethylene sarcoma formation [13]. Therefore, polytetrafluoroethylene is not currently in use. One of the most commonly used materials is collagen, which does not migrate to other sites. However, collagen is rapidly resorbed, so repeated injections are needed to maintain continence. A hypersensitivity reaction can also occur during collagen use [14]. Similar to collagen, autologous fat shows rapid resorption and is associated with a relatively low success rate. An adequate blood supply is essential for the maintenance of autologous fat; thus, the success rate is low when periurethral vascular injury is present after prostate surgery [15]. The Macroplastique used in this study is composed of textured silicon particles (polydimethylsiloxane) in a liquid gel. These particles have a low migration rate because they are larger than 100 µm, the injection material is encapsulated by nearby tissue, and there is a quiescent foreign body reaction that is maintained for 9 months [16]. Compared with other bulking agents, Macroplastique has stable characteristics.
Studies that have investigated transurethral injection treatment for male SUI have reported widely different success rates [2,12,16-27] (Table 4). This wide variation in success has several possible explanations. First, there is no common definition of success across studies. Studies also differed in terms of patient characteristics, injected materials, number of injections, and length of the postoperative follow-up period. In general, the results of previous studies indicate that treatment with an injection agent has a lower success rate than does AUS or a male urethral sling. Several factors may affect the success rate of injection. During radical prostatectomy, extensive scarring owing to multiple anastomotic incisions and scarring of the mucosal layer after radiation therapy can cause tight adhesion of the mucosa and muscle layer, or a "rigid urethra." Rigid urethra interferes with bulging and causes extravasation of materials [12]. The long length of the male urethra compared with the female urethra and technical failure owing to bulking agent migration may also contribute to the lower success rate of injection treatment [18].
In our study, the success rate was 43% at 1 month and 32% at 6 months. Our success rate was slightly lower than that reported in previous studies, perhaps because our definition of success was stricter than that used in previous studies and because of the low injection volume of our study. We considered success if the pad count was less than one pad per day with subjective symptom improvement. We believe our definition of success is more appropriate than that of previous studies because social continence is generally accepted to be less than one pad per day. Compared with the injection volume of the other study (range, 7.1-11.9 mL), the injection volume of our study was 5.3 mL (Table 4). We could not exclude the possibility of a relationship between a low injection volume and a low success rate. In addition, our study included patients who received only a single injection and excluded patients who received repeated injections because this approach yields more practical information for clinical practice. When injection treatment fails, most patients want a different surgical treatment rather than a repeat injection. Thus, determining the success rate after a single injection provides more useful data than determining the success rate after multiple injections when planning further treatment.
When we assessed incontinence by using the four-level SSI score, we found that the number of patients with severe or very severe incontinence decreased after surgery (before, 90%; after, 46.7%), but this change was not statistically significant. We believe that this result demonstrates improvement in subjective symptoms after Macroplastique injection treatment, although further study is needed.
Previous studies have identified several factors that influence the success of injection treatment. Increasing age is associated with problems such as low tissue quality, loss of ureter dexterity, and increased overactivity of the bladder [28]. Radiation therapy is associated with long-term consequences, such as obliteration of small vessels with subsequent endarteritis resulting in fibrosis, tissue ischemia, necrosis, and aberrant tissue repair [29]. Local anatomical distortion and tissue hypovascularity influence the results of surgery. Preoperative DO or low ALPP are also known to be negative risk factors for treatment success [30]. In the current study, patients who had a history of radiation therapy had a lower success rate (25%) than did those who did not (46.2%, p=0.427). Likewise, patients with an ALPP lower than 80 cm H2O had a lower success rate (25%) than did those whose ALPP was equal to or greater than 80 cm H2O (50%, p=0.222). However, these differences were not statistically significant, most likely owing to the small number of cases evaluated.
A potential limitation of this study was the retrospective cohort design. However, during the study period, our measurement and interpretation of clinical parameters such as pad number, SSI score, and urodynamic findings were consistent. Another limitation of this study was the small number of patients evaluated. Although our study period was longer than 6 years, only 30 patients who were treated during this period met the enrollment criteria.
Several studies have assessed the outcomes of bulking agent injection therapy with collagen, but few studies have examined outcomes after injection therapy with Macroplastique bulking agent for male SUI. To our knowledge, this is the first study to report outcomes of Macroplastique injection therapy to treat SUI in Korean men.
Injection therapy with Macroplastique bulking agent is a simple and relatively noninvasive surgical treatment for male SUI after prostate surgery with a short-term success rate of 43% and a longer-term success rate of 32%. There was a nonsignificant tendency for the treatment to be successful when patients had no preinjection radiation treatment history or when they had a higher ALPP. Our study provides useful information regarding the treatment options for male SUI after prostate surgery.
Figures and Tables
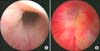 | FIG. 1Pre- and postinjection state of the urethral sphincter. (A) Preinjection state. The urethral lumen is wide open. (B) Postinjection state. The urethral lumen is coaptated. |
 | FIG. 2Benefit and satisfaction measurements for transurethral injection treatment. (A) Fifteen patients (50%) benefitted from the treatment and 13 patients (43%) reported much benefit. (B) Fifteen patients (50%) were also satisfied with the treatment, whereas only five patients (17%) were "very dissatisfied." |
References
1. Jung KW, Park S, Kong HJ, Won YJ, Lee JY, Seo HG, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2009. Cancer Res Treat. 2012; 44:11–24.
2. Westney OL, Bevan-Thomas R, Palmer JL, Cespedes RD, McGuire EJ. Transurethral collagen injections for male intrinsic sphincter deficiency: the University of Texas-Houston experience. J Urol. 2005; 174:994–997.
3. Sandvik H, Espuna M, Hunskaar S. Validity of the incontinence severity index: comparison with pad-weighing tests. Int Urogynecol J Pelvic Floor Dysfunct. 2006; 17:520–524.
4. Pleil AM, Coyne KS, Reese PR, Jumadilova Z, Rovner ES, Kelleher CJ. The validation of patient-rated global assessments of treatment benefit, satisfaction, and willingness to continue--the BSW. Value Health. 2005; 8:Suppl 1. S25–S34.
5. Catalona WJ, Carvalhal GF, Mager DE, Smith DS. Potency, continence and complication rates in 1,870 consecutive radical retropubic prostatectomies. J Urol. 1999; 162:433–438.
6. Fowler FJ Jr, Barry MJ, Lu-Yao G, Roman A, Wasson J, Wennberg JE. Patient-reported complications and follow-up treatment after radical prostatectomy. The National Medicare Experience: 1988-1990 (updated June 1993). Urology. 1993; 42:622–629.
7. Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Transurethral prostatectomy: immediate and postoperative complications: a cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol. 1989; 141:243–247.
8. Gousse AE, Madjar S, Lambert MM, Fishman IJ. Artificial urinary sphincter for post-radical prostatectomy urinary incontinence: long-term subjective results. J Urol. 2001; 166:1755–1758.
9. Trigo Rocha F, Gomes CM, Mitre AI, Arap S, Srougi M. A prospective study evaluating the efficacy of the artificial sphincter AMS 800 for the treatment of postradical prostatectomy urinary incontinence and the correlation between preoperative urodynamic and surgical outcomes. Urology. 2008; 71:85–89.
10. Cornel EB, Elzevier HW, Putter H. Can advance transobturator sling suspension cure male urinary postoperative stress incontinence? J Urol. 2010; 183:1459–1463.
11. Hübner WA, Gallistl H, Rutkowski M, Huber ER. Adjustable bulbourethral male sling: experience after 101 cases of moderate-to-severe male stress urinary incontinence. BJU Int. 2011; 107:777–782.
12. Elsergany R, Ghoniem GM. Collagen injection for intrinsic sphincteric deficiency in men: a reasonable option in selected patients. J Urol. 1998; 159:1504–1506.
13. Malizia AA Jr, Reiman HM, Myers RP, Sande JR, Barham SS, Benson RC Jr, et al. Migration and granulomatous reaction after periurethral injection of polytef (Teflon). JAMA. 1984; 251:3277–3281.
14. Stothers L, Goldenberg SL. Delayed hypersensitivity and systemic arthralgia following transurethral collagen injection for stress urinary incontinence. J Urol. 1998; 159:1507–1509.
15. Santarosa RP, Blaivas JG. Periurethral injection of autologous fat for the treatment of sphincteric incontinence. J Urol. 1994; 151:607–611.
16. Kylmälä T, Tainio H, Raitanen M, Tammela TL. Treatment of postoperative male urinary incontinence using transurethral macroplastique injections. J Endourol. 2003; 17:113–115.
17. Cummings JM, Boullier JA, Parra RO. Transurethral collagen injections in the therapy of post-radical prostatectomy stress incontinence. J Urol. 1996; 155:1011–1013.
18. Klutke JJ, Subir C, Andriole G, Klutke CG. Long-term results after antegrade collagen injection for stress urinary incontinence following radical retropubic prostatectomy. Urology. 1999; 53:974–977.
19. Martins FE, Bennett CJ, Dunn M, Filho D, Keller T, Lieskovsky G. Adverse prognostic features of collagen injection therapy for urinary incontinence following radical retropubic prostatectomy. J Urol. 1997; 158:1745–1749.
20. Colombo T, Augustin H, Breinl E, Schips L, Hubmer G. The use of polydimethylsiloxane in the treatment of incontinence after radical prostatectomy. Br J Urol. 1997; 80:923–926.
21. Griebling TL, Kreder KJ Jr, Williams RD. Transurethral collagen injection for treatment of postprostatectomy urinary incontinence in men. Urology. 1997; 49:907–912.
22. Faerber GJ, Richardson TD. Long-term results of transurethral collagen injection in men with intrinsic sphincter deficiency. J Endourol. 1997; 11:273–277.
23. Smith DN, Appell RA, Rackley RR, Winters JC. Collagen injection therapy for post-prostatectomy incontinence. J Urol. 1998; 160:364–367.
24. Tiguert R, Gheiler EL, Gudziak MR. Collagen injection in the management of post-radical prostatectomy intrinsic sphincteric deficiency. Neurourol Urodyn. 1999; 18:653–658.
25. Schneider T, Sperling H, Rossi R, Schmidt S, Rubben H. Do early injections of bulking agents following radical prostatectomy improve early continence? World J Urol. 2005; 23:338–342.
26. Imamoglu MA, Tuygun C, Bakirtas H, Yigitbasi O, Kiper A. The comparison of artificial urinary sphincter implantation and endourethral macroplastique injection for the treatment of post-prostatectomy incontinence. Eur Urol. 2005; 47:209–213.
27. Onur R, Singla A. Comparison of bone-anchored male sling and collagen implant for the treatment of male incontinence. Int J Urol. 2006; 13:1207–1211.
28. Costa P, Poinas G, Ben Naoum K, Bouzoubaa K, Wagner L, Soustelle L, et al. Long-term results of artificial urinary sphincter for women with type III stress urinary incontinence. Eur Urol. 2013; 63:753–758.
29. Raj GV, Peterson AC, Webster GD. Outcomes following erosions of the artificial urinary sphincter. J Urol. 2006; 175:2186–2190.
30. Kim SP, Sarmast Z, Daignault S, Faerber GJ, McGuire EJ, Latini JM. Long-term durability and functional outcomes among patients with artificial urinary sphincters: a 10-year retrospective review from the University of Michigan. J Urol. 2008; 179:1912–1916.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download