Abstract
Purpose
The homeobox (Hox) genes a and d controlling limb and genital development influence the digit ratio and the fetal production of testicular androgen, which may result in testicular descent in boys. To assess whether the digit ratio reflects disease status, we investigated the second and fourth finger lengths in children with cryptorchidism, in children with hydrocele as a disease control, and in healthy controls (boys and girls).
Materials and Methods
One hundred ninety-six children (46 with cryptorchidism, 50 with hydrocele, 50 healthy boys, and 50 healthy girls) who were 6 to 23 months of age were prospectively enrolled. Digit lengths were measured by 2 investigators, and the mean value was recorded.
Results
The second-to-fourth digit ratios (2D:4Ds) of the left hand in the cryptorchidism group, hydrocele group, healthy boys, and healthy girls were 0.958, 0.956, 0.950, and 0.956, respectively. The 2D:4D values of the right hand were 0.946, 0.945, 0.952, and 0.969, respectively. The right and left 2D:4D ratios were not significantly different among groups. The 2D:4D of both hands was not related to age, weight, or height.
The second-to-fourth digit ratio (2D:4D), especially on the right hand, differs between boys and girls. Manning et al. [1] suggested that the mean right 2D:4D is lower in boys than in girls and that the difference is negatively related to prenatal and adult testosterone levels. They observed no change in the 2D:4D with age (0-28 years) in a cross-sectional study and suggested that this ratio is determined in utero or in the first 2 years of life. Trivers et al. [2] proposed that the 2D:4D ratio increases with age and its difference between genders decreases with age. The difference was more marked in the left hand, whereas the ratio of the right hand was stable in school aged children (7-11 years). In addition, a meta-analysis showed that the 2D:4D is not associated with adult sex hormone levels [3]. The longitudinal stability of the digit ratio suggests that the sexual dimorphism is fixed early in development [4,5].
Testicular descent is completed through an interplay among regression of müllerian structure by müllerian inhibitory factor, abdominal pressure, a patent processus vaginalis, and gubernacular regression. Androgens predominantly control the inguinoscrotal phase to descend from the inguinal ring into the scrotum. In this process, the development of the gubernaculum dilating inguinal ring and androgen-induced gubernacular regression are important to testicular descent [6]. Prenatal exposure to androgens also has an important role in the development of cryptorchidism.
The homeobox (Hox) genes a and d control limb and genital development. These may influence the digit ratio and the fetal production of testicular androgen, which may result in testicular descent in boys [4,5,7]. On the basis of this evidence and pathophysiology, we hypothesized that the digit ratio would differ in cryptorchidism and reflect the disease condition. Thus, we investigated and compared the digit length in children with cryptorchidism, in children with hydrocele as a disease control, and in healthy controls (boys and girls).
We prospectively enrolled 196 children aged 6 to 23 months. The subjects were divided into 4 groups (46 boys with cryptorchidism, 50 boys with hydrocele or indirect inguinal hernia, 50 healthy boys, and 50 healthy girls). We recruited healthy controls from among children who visited the pediatric ward of Eulji University Hospital for upper respiratory infections or enteritis. The cryptorchidism and hydrocele groups included children who underwent an operation for their disease in the Urology Department. Children who had any endocrine or developmental disorder or other urogenital disease were excluded. The parents of each subject provided informed consent before participation in this trial, and the institutional review board of our center approved the study.
We measured all children's height, weight, and finger lengths. The second and fourth digit lengths of both hands were measured from the ventral crease to the tip of the finger by using digital Vernier calipers accurate to 0.01 mm. To minimize error, the measurements were performed by 2 investigators for each child and the mean value was adopted. This measurement has been accepted in earlier studies as providing a high degree of repeatability [8].
All statistical analyses were performed by using R ver. 3.0.2 (R Foundation for Statistical Computing, Vienna, Austria). The quantitative results are presented as mean±standard deviation (SD). Statistical analyses of the 2D:4D were performed by using analysis of variance for the differences among 4 groups and Pearson linear correlation for the relationships among 2D:4D ratio, age, height, and weight. Statistical significance was assigned at p-values <0.05.
The mean±SD of age, height, and weight of the children and lengths of the second and fourth fingers are summarized in Table 1. Age, height, weight, and finger lengths did not differ significantly among groups. The cryptorchidism group consisted of 3 abdominal cases, 25 nonpalpable inguinal cases, and 18 palpable inguinal or prepubic type cases. Bilateral cryptorchidism occurred in 6 cases.
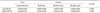
The left 2D:4D values in the cryptorchidism group, hydrocele group, healthy boys, and healthy girls were 0.958, 0.956, 0.950, and 0.956, respectively. The right 2D:4D values were 0.946, 0.945, 0.952, and 0.969, respectively (Table 2, Fig. 1). There were no significant differences among the groups in right or left 2D:4D (p=1.00 and 0.994 for cryptorchidism-hydrocele, p=0.904 and 0.984 for cryptorchidism-healthy boys, p=0.142 and 1.00 for cryptorchidism-healthy girls, p=0.885 and 1.00 for hydrocele-healthy boys, p=0.156 and 0.994 for hydrocele-healthy girls, and p=0.441 and 0.984 for healthy boys-healthy girls, respectively).
The lengths of the second and fourth fingers showed a significantly positive correlation with age, weight, and height, but the 2D:4D of either hand was not correlated with these variables (Table 3).
It has been reported that the difference in 2D:4D in children is related to variable medical conditions, such as endocrinologic diseases related to androgen secretion or sensitivity, psychopathologic disorder, and physical and mental developments. The difference in the digit ratio and the fetal production of testicular androgen may be controlled by Hox genes a and d, which may influence testicular descent in boys [4,5,7]. However, there are few studies of the relationship between urologic disease and digit ratio in children.
The principal objective of this study was to identify any difference in the digit ratio in children with cryptorchidism compared with a disease control group and a healthy control groups. However, we did not find any statistical difference in the 2D:4D of either hand between boys with cryptorchidism and boys with hydrocele or healthy controls (boys and girls). Furthermore, we did not find a gender difference between healthy boys and healthy girls. The lack of significant difference in the digit ratio between groups may indicate two possibilities: (1) differences in fetal exposure to androgens or the sensitivity of androgen receptor (AR) between groups may have been too small to result in a difference between the cryptorchidism and control groups, and (2) the infantile period is too early to recognize the difference in the digit ratio between the cryptorchidism and control groups. However, longitudinal and larger cohort studies are required to confirm our results.
It has been reported that the right 2D:4D differs between genders, with no evidence of a change with age (2-18 years) or in an ethnically diverse group of children (5-14 years) [1,9]. This evidence supports the hypothesis that the digit ratio is established in the prenatal period, is presented at least before 2 years of age, and is stable with growth in children. However, a longitudinal investigation of children aged 0-2 years showed that the right-hand 2D:4D was weakly correlated with prenatal/adult testosterone level, and the 2D:4D did not differ between genders at 12 or 24 months of age and was not stable over time [10,11]. In other longitudinal series, the left 2D:4D positively increased with age in children aged 5-17 years and the ratios in both hands slightly increased with age in preschool children aged 2-5 years [1,5,12]. Our cross-sectional investigation of 400 Korean children (0-9 years) showed that the gender difference presented at age over 3 years and was not evident at age 0-3 years (not published). As for these results, the difference in 2D:4D between boys cryptorchidism and controls may unfold with increasing age, although the 2D:4D in our series failed to show a difference according to disease condition in the infant period.
Activation of AR by prenatal testosterone is known to contribute to the development of boys' internal and external genitalia and reduces values of 2D:4D [12-14]. It has been well established that the sensitivity of AR to testosterone is influenced by allelic variation according to the numbers of CAG triplets, and the number of CAG repeats is negatively associated with the sensitivity to testosterone [15,16]. Manning et al. [17] demonstrated that men with a low number of CAG repeats in the AR gene had a lower value of the right 2D:4D than did men with high numbers of CAG triplets.
Recent studies have shown an association between variation in AR CAG repeat length and cryptorchidism. A high number of CAG repeats has been associated with cryptorchidism, especially bilateral cases, and the combination of CGA/GGC repeat length is strongly associated with cryptorchidism [18-22]. Silva-Ramos et al. [20] reported that longer CAG repeats may be associated with slower testicular descent and incomplete closure of the processus vaginalis. However, there was no significant difference in CAG repeat length in unilateral cryptorchidism and in the patent processus vaginalis compared with controls [20]. Sasagawa et al. [23] did not find an association between CAG repeat length and cryptorchidism and suggested that the expansion of CAG repeats is unlikely to be a major cause of cryptorchidism in the Japanese population. It is known that CAG repeat length is longer and the incidence of cryptorchidism is higher in Asian populations than in Caucasians [24,25]. As well, the mean 2D:4D is higher in Asians (Oriental Han) than in Caucasians, Uygurs, and Afro-Caribbean Jamaicans [9]. Perhaps the ethnic variation of CAG repeat length could explain the ethnic difference in the digit ratio. Considering that our subjects were of the same ethnicity and 87% of the cryptorchidism was unilateral, the difference in the number of CAG repeats between the cryptorchidism and control groups may have been weak, which might have resulted in the lack of significant difference in values of 2D:4D among groups in our study.
This study had some limitations. This was a small sized study because we limited the disease group to children who underwent orchiopexy at the age of 0-2 years and selected control groups matched to the cryptorchidism group. For these reasons, statistical power was not strong (power=0.784 and 0.645 for left and right), rejecting completely that the 2D:4D ratio is different between boys with cryptorchidism and controls. Also, healthy boys and girls were recruited from the pediatric department among hospitalized children with upper respiratory infections or enteritis. Therefore, the controls do not represent a normal population. Another limitation is that we did not consider the influence of pre- and postnatal sex steroid exposure and the difference of digit ratio according to bilaterality and severity of cryptorchidism. Despite these limitations, the current study is the first report comparing the digit ratio between boys with cryptorchidism and controls and supports that the use of the digit ratio as a noninvasive retrospective biomarker reflecting disease condition is controversial.
In the current study, we did not find any statistical difference in the 2D:4D of either hand between the cryptorchidism group and the hydrocele group and healthy controls (boys and girls). We also did not find a gender difference between healthy boys and girls. The study suggests that the use of the digit ratio as a noninvasive retrospective biomarker reflecting disease condition during the infantile period is controversial. However, longitudinal and larger comprehensive cohort studies are required to confirm our results.
Figures and Tables
 | FIG. 1Median and standard errors for 2D:4D in the left (A) and the right (B) hands of the cryptorchidism group, hydrocele group, and healthy boys and girls. 2D:4D, second-to-fourth digit ratio. |
References
1. Manning JT, Scutt D, Wilson J, Lewis-Jones DI. The ratio of 2nd to 4th digit length: a predictor of sperm numbers and concentrations of testosterone, luteinizing hormone and oestrogen. Hum Reprod. 1998; 13:3000–3004.
2. Trivers R, Manning J, Jacobson A. A longitudinal study of digit ratio (2D:4D) and other finger ratios in Jamaican children. Horm Behav. 2006; 49:150–156.
3. Hönekopp J, Bartholdt L, Beier L, Liebert A. Second to fourth digit length ratio (2D:4D) and adult sex hormone levels: new data and a meta-analytic review. Psychoneuroendocrinology. 2007; 32:313–321.
4. Kondo T, Zakany J, Innis JW, Duboule D. Of fingers, toes and penises. Nature. 1997; 390:29.
5. Galis F, Ten Broek CM, Van Dongen S, Wijnaendts LC. Sexual dimorphism in the prenatal digit ratio (2D:4D). Arch Sex Behav. 2010; 39:57–62.
6. Hughes IA, Acerini CL. Factors controlling testis descent. Eur J Endocrinol. 2008; 159:Suppl 1. S75–S82.
7. Nagraj S, Seah GJ, Farmer PJ, Davies B, Southwell B, Lewis AG, et al. The development and anatomy of the gubernaculum in Hoxa11 knockout mice. J Pediatr Surg. 2011; 46:387–392.
8. Scutt D, Manning JT. Symmetry and ovulation in women. Hum Reprod. 1996; 11:2477–2480.
9. Manning JT, Stewart A, Bundred PE, Trivers RL. Sex and ethnic differences in 2nd to 4th digit ratio of children. Early Hum Dev. 2004; 80:161–168.
10. Lutchmaya S, Baron-Cohen S, Raggatt P, Knickmeyer R, Manning JT. 2nd to 4th digit ratios, fetal testosterone and estradiol. Early Hum Dev. 2004; 77:23–28.
11. Knickmeyer RC, Woolson S, Hamer RM, Konneker T, Gilmore JH. 2D:4D ratios in the first 2 years of life: Stability and relation to testosterone exposure and sensitivity. Horm Behav. 2011; 60:256–263.
12. Brown WM, Hines M, Fane BA, Breedlove SM. Masculinized finger length patterns in human males and females with congenital adrenal hyperplasia. Horm Behav. 2002; 42:380–386.
13. Byne W. Developmental endocrine influences on gender identity: implications for management of disorders of sex development. Mt Sinai J Med. 2006; 73:950–959.
14. Buck JJ, Williams RM, Hughes IA, Acerini CL. In-utero androgen exposure and 2nd to 4th digit length ratio-comparisons between healthy controls and females with classical congenital adrenal hyperplasia. Hum Reprod. 2003; 18:976–979.
15. Chamberlain NL, Driver ED, Miesfeld RL. The length and location of CAG trinucleotide repeats in the androgen receptor N-terminal domain affect transactivation function. Nucleic Acids Res. 1994; 22:3181–3186.
16. Kazemi-Esfarjani P, Trifiro MA, Pinsky L. Evidence for a repressive function of the long polyglutamine tract in the human androgen receptor: possible pathogenetic relevance for the (CAG)n-expanded neuronopathies. Hum Mol Genet. 1995; 4:523–527.
17. Manning JT, Bundred PE, Newton DJ, Flanagan BF. The second to fourth digit ratio and variation in the androgen receptor gene. Evol Hum Behav. 2003; 24:399–405.
18. Aschim EL, Nordenskjold A, Giwercman A, Lundin KB, Ruhayel Y, Haugen TB, et al. Linkage between cryptorchidism, hypospadias, and GGN repeat length in the androgen receptor gene. J Clin Endocrinol Metab. 2004; 89:5105–5109.
19. Lim HN, Nixon RM, Chen H, Hughes IA, Hawkins JR. Evidence that longer androgen receptor polyglutamine repeats are a causal factor for genital abnormalities. J Clin Endocrinol Metab. 2001; 86:3207–3210.
20. Silva-Ramos M, Oliveira JM, Cabeda JM, Reis A, Soares J, Pimenta A. The CAG repeat within the androgen receptor gene and its relationship to cryptorchidism. Int Braz J Urol. 2006; 32:330–334.
21. Davis-Dao CA, Tuazon ED, Sokol RZ, Cortessis VK. Male infertility and variation in CAG repeat length in the androgen receptor gene: a meta-analysis. J Clin Endocrinol Metab. 2007; 92:4319–4326.
22. Radpour R, Rezaee M, Tavasoly A, Solati S, Saleki A. Association of long polyglycine tracts (GGN repeats) in exon 1 of the androgen receptor gene with cryptorchidism and penile hypospadias in Iranian patients. J Androl. 2007; 28:164–169.
23. Sasagawa I, Suzuki Y, Tateno T, Nakada T, Muroya K, Ogata T. CAG repeat length of the androgen receptor gene in Japanese males with cryptorchidism. Mol Hum Reprod. 2000; 6:973–975.
24. Hsing AW, Gao YT, Wu G, Wang X, Deng J, Chen YL, et al. Polymorphic CAG and GGN repeat lengths in the androgen receptor gene and prostate cancer risk: a population-based case-control study in China. Cancer Res. 2000; 60:5111–5116.
25. Berkowitz GS, Lapinski RH. Risk factors for cryptorchidism: a nested case-control study. Paediatr Perinat Epidemiol. 1996; 10:39–51.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download