Abstract
Purpose
Infertile couples interested in nonspouse artificial insemination by donor (AID) not only require a thorough understanding of the medical procedure but also must scrutinize the effects it will have on family relationships, including those on the infant to be born. We conducted a series of surveys in couples with male infertility to collect information necessary for AID counseling.
Materials and Methods
A total of 384 cases with noncurable male infertility were enrolled in this inquiry survey. The questionnaire consisted of 18 items that assessed demographic characteristics, background information concerning the choice to use AID, subjective experiences, long-term effects, and an overall evaluation.
Results
A total of 126 surveys were returned (32.8%). AID was first suggested by the husband in about half of the cases. The major reason for considering the procedure was to form a complete family. Two-thirds of the couples were anxious about the procedure, most often about possible congenital or acquired deformities in the infant. After the birth of the child, most couples were positive about their decision to have used AID. About half of the couples felt that the child was their own and expected not to tell the child about AID. Overall, about 50% of the couples were satisfied with the procedure.
Conclusions
Those who underwent AID experienced various psychological effects, including anxiety about the child to be born. To overcome these problems, sufficient medical information and consultation about the process of selecting the donor and about AID procedures should be provided before the procedure is used.
Artificial insemination by donor (AID) is a reproductive medical procedure for infertile couples that entails insertion of a fine catheter directly into the uterus to deposit a sperm sample from a donor with the aim of achieving pregnancy. AID is used primarily in male spouses with incurable nonobstructive azoospermia or other related problems [1].
AID was initially introduced in the United States in the 1960s. However, its introduction in Korea in 1993 has raised social and medical concerns related to the use of fresh sperm in AID. Subsequently, the Korean Society of Obstetrics and Gynecology Ethical Outlines and Operation Procedures for AID were amended in the fifth revised edition, and the "Declaration of Artificial Conception Ethics" was also announced, which reiterated that the procedures and guidelines are ethically, medically, and administratively acceptable [2]. Recently, The Ministry of Health and Welfare preannounced "legislation on bio-ethics and safety" to strengthen national authority on reproductive diagnoses and research on the ethics and safety of such procedures.
We established the first public sperm bank in Korea in April 1997, which at that point considered only self-produced sperm from spouses and nonspouses based on the Declaration of Artificial Conception Ethics and Guidelines for Gamete and Embryo Donation by the American Society for Reproductive Medicine [3].
The implementation of AID was followed by a rise in psychological anxiety and conflict in infertile couples because the sperm from a nonspouse is used. Significant distress is likely to follow for the husband because of his own impaired reproductive health, the use of a stranger's sperm, and concern about genetic differences between him and his future child. The wife may also feel depressed about the potential for problems in the relationship with her husband or with other family members as a result of becoming pregnant via AID. Thus, a more careful consideration of the timing and frequency of the procedure and of the effect that it will have on the family relationship is warranted to minimize these problems.
We conducted a series of surveys in couples with male infertility to collect information necessary for AID counseling. AID had been recommended to these couples, or they had already undergone the procedure, and we investigated how the decision to use AID was made and how the infertile husband felt about the situation.
In total, 126 inquiry surveys (32.8%) were completed from among 384 distributed to couples with male infertility who lived in the Busan and Gyoungnam Provinces and who had visited the fertility clinic at Pusan National University Hospital to receive or explore AID from November 1997 to November 2012.
All questionnaires were submitted during a hospital visit or through the mail. The questionnaire used in the study was developed for the purposes of this study and consisted of 18 questions in five different topic areas: (1) demographic characteristics (average age of the couple, marriage duration, number of children, and sex ratio), (2) background concerning the choice to use AID (route of choice, person who recommended and discussed AID, reasons for the decision), (3) subjective experiences related to using AID (expected degree of surgical procedure, presence of anxiety and its causes, and desire for an infant), (4) long-term effects of AID (effects of both success and failure of the pregnancy on psychological status, feelings after the pregnancy, changes in views of life, feelings about children growing up, and whether or not the child will be notified of AID), and (5) overall evaluation of AID (satisfaction, need for the medical procedure, preference for another procedure) (Supplementary questionnaire).
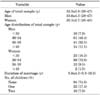
The average ages of the husbands and wives were 33.6±4.3 and 30.1±2.7 years, respectively (Table 1). Sixty-one males (48.4%) and 91 females (72.2%) were 30-34 years old. The average length of marriage was 5 years, 8 months. In addition, 52 participants (41.2%) had 69 children who were born through AID, and the boy:girl ratio was 2.28:1.
About 37.3% of the infertile couples (47 respondents) learned about AID from doctors, 34.1% (43 respondents) from books and magazines, 11.1% (14 respondents) through television and the Internet (news, blogs, Internet cafés, information boards, etc.), 7.1% (9 respondents) from people around them, 3.2% (4 respondents) through the newspaper, 1.7% (2 respondents) from people who had previously undergone AID, and 1.6% (2 respondents) through movies. Of these sources, mass media such as books, magazines, television, the Internet, movies, and newspapers were the source of information for 50% (63 respondents)-the highest proportion.
About 56% of the respondents (n=71) answered that the husband recommended AID, about 32.5% (n=41) that the wife recommended AID, and about 11.1% (n=14) that both the husband and wife recommended AID.
With regard to other people with whom AID was discussed, the highest proportion, about 65% of respondents (n=82), answered that they discussed AID with their wives. About 19% of respondents (n=24) had discussed it with their parents, 8.7% (n=11) with their families, 5.5% (n=7) with their wives and friends, and 1.5% (n=2) with their wives, brothers, and sisters. The wife was regarded as the most important person when deciding whether to undergo AID.
About 86% (n=109) of respondents answered that they wanted to undergo AID to form a perfect family, followed by 53.1% (n=67) who simply wanted children. Keeping the marriage, maintaining a normal life, not interested in adoption, and preparation for later years were mentioned by 41.2% (52 respondents), 37.3% (47 respondents), 27.7% (35 respondents), and 22.2% (28 respondents).
Approximately 46% of respondents (n=58) answered that they strongly wanted AID, and 23.0% (n=29) answered that they were uncertain. A strong recommendation from the wife and no preference accounted for 20.6% (26 respondents) and 10.3% (13 respondents) of the answers (n=126).
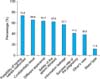
About 70% of respondents (n=88) were anxious when AID was being implemented. The reasons for the anxiety were the possibility of delivering a malformed infant in 73.8% of respondents (n=93), issues of confidentiality in 65.8% (n=83), difference in appearance between the father and child in 64.2% (n=81), the safety of the donated sperm in 62.6% (n=79), information leakage in 57.1% (n=72), success rate of the pregnancy in 41.2% (n=52), public judgment in 38.8% (n=49), and incompatible blood type in 11.9% (n=46) (Fig. 2).
About 61% of respondents (n=77) answered that they very much wanted to participate in AID, followed by 36.5% (46 respondents) with a moderate interest in doing so. Only 2.3% (3 respondents) had a low interest in AID as an option. However, respondents generally wanted to have children.
When AID was successful (n=57), 45.6% of respondents (n=26) reported both good and bad feelings, whereas 8.7% (n=5) felt good and had a generally positive reaction about the pregnancy.
When AID failed (n=37), 51.3% (19 respondents) wanted to forget the result, 29.7% (11 respondents) answered that they blamed their doctors, and 24.3% (9 respondents) reported regret, acceptance, or no thought at all about AID. This outcome represented failure of the pregnancy, which frustrated patients.
In terms of their initial feelings upon holding the infant after birth (n=47), 68.0% of respondents (n=32) answered that they felt very good, 23.4% (11 respondents) that they had both good feelings and anxiety, and 8.5% (n=4) that they felt good.
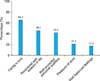
About 71% of 52 respondents (n=37) reported that AID positively changed their view of life, whereas 28.8% (n=15) had both positive and negative reactions. Positive aspects of the experience were expressed in terms of family love by 65.3% (34 respondents), recovered self-esteem by 46.1% (24 respondents), being viewed as an acceptable person by 42.3% (22 respondents), being pleased with their work in 21.1% (11 respondents), and well-balanced feelings in 17.3% (9 respondents) (Fig. 3).
With regard to negative responses (n=15), 60.0% of respondents (n=9) were self-conscious about others' reactions, 40.0% (n=6) felt a sense of alienation, and 13.3% (n=2) felt anxious about the growth of their child. About 63% of respondents (n=31) accepted infants born through AID as their own children, and 26.5% (n=13) expressed a positive reaction when similarities to them were found. About 20% of respondents (n=10) felt uncomfortable with others' views, 14.2% (n=7) reported that the child looked different from them, and 6.1% (n=3) mentioned a difference in personality.
In regard to telling their children about AID (n=77), 41.5% of respondents (n=32) strongly disagreed with telling the truth to their child, 29.8% (n=23) wanted to hide the truth, 19.4% (n=15) reported that they had not thought about this, and only 9.0% (n=7) wanted to decide depending on the situation (Fig. 4).
Nearly 75.0% of respondents (n=66) were satisfied with AID, 15.0% (n=12) were strongly satisfied, and 2.5% (n=2) expressed intense satisfaction. Additionally, all 91 respondents agreed with the importance of AID as an option in cases of male infertility.
About 54% of respondents (n=34) answered that they would consider undergoing AID again to have another child, 26.9% (n=17) disagreed with undergoing AID again, 12.6% (n=8) agreed with participating in AID again, and 6.3% (n=4) never wanted to undergo AID again.
AID has been widely used for infertile couples with aspermia, incurable male infertility, or a high incidence of severe hereditary diseases passed through the sperm. In the United States, the annual rate of pregnancy by AID was about 30,000, and >170,000 females were treated with AID in 1987 [4]. AID has also been used as a major treatment for male infertility in Korea, and the ethics and legality of the procedures have been emphasized.
The Declaration of Artificial Conception Ethics indicates that AID should be used only for couples who are legally married and infertile. Participation of the husband in AID should be voluntary. Sperm from the same donor can be used for pregnancy no more than 10 times, and all information about the donor is kept confidential. Furthermore, the result of the procedure is not be revealed to the donor [2].
In fact, the actual conditions and statistics regarding AID are incomplete, because many patients directly involved in AID prefer to hide that they are undergoing AID. Therefore, appropriate counseling should be given to couples who want AID, and the psychological effect of AID on the couple should be studied. This survey was conducted in infertile male patients, who planned to have AID, to identify how they felt about the procedure.
About 13% of the survey results (41/321) were collected by mail, which was lower than that (79.6%, 121/152) for a prospective survey at a fertility clinic. Klock and Maier [5] reported that a mail survey can possibly threaten the confidentiality of couples and that this issue would affect the participation rate in a retrospective survey. Most couples who participated in the current survey were aged 30-34 years, as older couples were less inclined to participate. According to Nachtigall et al. [1], respondents among patients undergoing AID were younger than ones not having undergone AID. Additionally, 109 of 126 women (86.5%) who underwent AID and became pregnant gave birth at other hospitals. This may be because of the convenience of another hospital's location and a desire to keep their status confidential.
Karow Jr [6] reported that confidentiality was so important to infertile couples undergoing AID that they often gave birth in a hospital where their children would not be recognized as AID-born children. This attitude was attributed to the fact that infertile women in Western countries are generally supported by their family and friends, whereas infertile men may encounter negative responses, such as ridicule.
Until now, reports of the sex ratio of children conceived through AID have been conflicting. Our study indicated that more boys than girls (2.28 times) were born through AID; however, the actual statistics are unclear. For example, some studies have shown a higher ratio of boys to girls [7,8], and others have shown the reverse [9-11]. To explain this difference, some researchers have shown that the lower basal body temperature of women is more likely to lead to the birth of a boy [12,13]. Others have suggested that the use of ovulation-induction treatments involving mixed ovulation increases the chance of a girl being born [14,15]. From the point of view of the sample size of all reported studies, it remains difficult to form a conclusion about sex ratio of children conceived through AID.
The psychological effect of deciding to undergo AID, and the procedure itself, is not negligible. Nachtigall et al. [1] stated that the male patients with infertility are more likely to develop psychological distress and lose self-respect than are infertile females. According to Klock et al. [16], this is demonstrated by the observation that fertility and intercourse are more important to males than females; thus, infertility in males is likely to have a greater negative impact on self-respect.
We found that when AID was recommended to husbands, and for about two-thirds of them, discussions with their wives on the matter dealt only with keeping the procedure a secret. Wright et al. [17] found similar differences in attitudes and responses from males and females towards AID.
As reducing anxiety due to AID is a priority, approximately two-thirds of respondents in the survey should have received active counseling. and Klock et al. [16] emphasized the expected effects of counseling on reducing anxiety and also suggested that medical advice from mental-health professionals is necessary before couples undergo AID, because the safety of the donor's genetic and medical history is not fully guaranteed. We found that the possibility of having a child with a disability was 60% greater than with typical births. Verp et al. [18] showed that broader screening for genetic abnormalities is not needed, because the frequency of malformations (2.3%) in typical-birth infants was similar to the frequency (1.7%) in infants resulting from AID. However, a higher age at pregnancy negatively affects the success of AID (Virro and Shewchuk [13]). Thus, Klock et al. [16] suggested that physicians remind infertile couples of the availability of counseling. That study also stressed the importance of counseling for patients who have experienced pregnancy failure through AID and are unwilling to try again.
Most couples who have children through AID maintain a stable marriage, as evidenced by a lower than average rate of divorce in these families [19,20]: 2.2% [21] in Norway and 7.2% [22] in the United States [23]. The positive effect of AID on marriage was shown by Amuzu et al. [22] and Schover et al. [24], who reported that the mental status and self-respect of infertile couples are within the normal range. Our results suggest that about 70% of couples have an overall positive view of AID.
With regard to notifying children that they were born through AID, Nachtigall et al. [1] stated that 30% of couples told their children that they were conceived through AID, Klock et al. [16] reported a figure of 27%, and other studies reported a figure of 14% to 20% [5,22] However, in our study, only 7.6% of the respondents planned to notify their children. The success of pregnancy through AID has encouraged more couples to undergo AID [25,26] and, according to Curie-Cohen et al. [3], about 11% of infertile couples revisit the fertility clinic to have a second child via AID (12.6% prefer AID for having a second child).
Figures and Tables
ACKNOWLEDGMENTS
This study was supported by a clinical grant from Pusan National University Hospital (2012).
References
1. Nachtigall RD, Tschann JM, Quiroga SS, Pitcher L, Becker G. Stigma, disclosure, and family functioning among parents of children conceived through donor insemination. Fertil Steril. 1997; 68:83–89.
2. Korean Society of Obstetrics and Gynecology [Internet]. Seoul: Korean Society of Obstetrics and Gynecology;c2014. cited 2013 Sep 5. Available from: http://ksog.org.
3. Curie-Cohen M, Luttrell L, Shapiro S. Current practice of artificial insemination by donor in the United States. N Engl J Med. 1979; 300:585–590.
4. Critser JK. Current status of semen banking in the USA. Hum Reprod. 1998; 13:Suppl 2. 55–67.
5. Klock SC, Maier D. Psychological factors related to donor insemination. Fertil Steril. 1991; 56:489–495.
6. Karow AM Jr. Family secrets: who is to know about AID? N Engl J Med. 1982; 306:372.
7. Mochimaru F. Artificial insemination with frozen donor semen: its current status and follow-up studies. Keio J Med. 1979; 28:33–48.
8. Katzorke T, Propping D, Tauber PF. Results of donor artificial insemination (AID) in 415 couples. Int J Fertil. 1981; 26:260–266.
9. Aiman J. Factors affecting the success of donor insemination. Fertil Steril. 1982; 37:94–99.
10. Chong AP, Taymor ML. Sixteen years' experience with therapeutic donor insemination. Fertil Steril. 1975; 26:791–795.
11. Achanna S, Monga D. Outcome of forceps delivery versus vacuum extraction: a review of 200 cases. Singapore Med J. 1994; 35:605–608.
12. Harlap S. Gender of infants conceived on different days of the menstrual cycle. N Engl J Med. 1979; 300:1445–1448.
13. Virro MR, Shewchuk AB. Pregnancy outcome in 242 conceptions after artificial insemination with donor sperm and effects of maternal age on the prognosis for successful pregnancy. Am J Obstet Gynecol. 1984; 148:518–524.
14. Adashi EY, Rock JA, Sapp KC, Martin EJ, Wentz AC, Jones GS. Gestational outcome of clomiphene-related conceptions. Fertil Steril. 1979; 31:620–626.
15. James WH. Artificial insemination by donor: a review of 12 years' experience. J Biosoc Sci. 1984; 16:153–154.
16. Klock SC, Jacob MC, Maier D. A prospective study of donor insemination recipients: secrecy, privacy, and disclosure. Fertil Steril. 1994; 62:477–484.
17. Wright J, Duchesne C, Sabourin S, Bissonnette F, Benoit J, Girard Y. Psychosocial distress and infertility: men and women respond differently. Fertil Steril. 1991; 55:100–108.
18. Verp MS, Cohen MR, Simpson JL. Necessity of formal genetic screening in artificial insemination by donor. Obstet Gynecol. 1983; 62:474–479.
19. Clayton CE, Kovacs GT. A.I.D.: a pretreatment social assessment. Aust N Z J Obstet Gynaecol. 1980; 20:208–210.
20. Stewart CR, Daniels KR, Boulnois JD. The development of a psychosocial approach to artificial insemination of donor sperm. N Z Med J. 1982; 95:853–856.
21. Bendvold E, Moe N, Skjaeraasen J. Social conditions of children born after artificial insemination by donor. Scand J Soc Med. 1990; 18:203–206.
22. Amuzu B, Laxova R, Shapiro SS. Pregnancy outcome, health of children, and family adjustment after donor insemination. Obstet Gynecol. 1990; 75:899–905.
23. Lansac J, Royere D. Follow-up studies of children born after frozen sperm donation. Hum Reprod Update. 2001; 7:33–37.
24. Schover LR, Collins RL, Richards S. Psychological aspects of donor insemination: evaluation and follow-up of recipient couples. Fertil Steril. 1992; 57:583–590.
25. Farpis EJ, Garrison M Jr. Emotional impact of successful donor insemination; a report on 38 couples. Obstet Gynecol. 1954; 3:19–20.
26. David A, Avidan D. Artificial insemination donor: clinical and psychologic aspects. Fertil Steril. 1976; 27:528–532.
SUPPLEMENTARY MATERIALS
Supplementary questionnaire

Scan this QR code to see the supplementary questionnaire, or visit http://www.kjurology.org/src/sm/kju-55-134-s001.pdf.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download