Abstract
Purpose
The purpose of this study was to identify the risk factors for recatheterization after holmium laser enucleation of the prostate (HoLEP).
Materials and Methods
A total of 166 consecutive patients treated with HoLEP by a single surgeon from January 2010 to June 2011 were enrolled in this study. We collected data on preoperative and intraoperative parameters, including intraoperative bladder distention volume. The patients were divided into two groups. Group 1 included patients who voided successfully after removal of the catheter, and group 2 included patients who required recatheterization. Analysis and comparison of the perioperative parameters of both groups was performed for identification of risk factors for recatheterization.
Results
Recatheterization was required in 9 of 166 (5.4%) patients. No significant differences in age or preoperative parameters, including prostate-specific antigen, prostate volume, International Prostate Symptom Score, peak flow rate, postvoid residual urine, maximal bladder capacity, and Abrahams Griffiths number, were observed between the two groups. Of the intraoperative parameters, intraoperative bladder distention volume was significantly smaller in group 1 than in group 2 (700.65 mL vs. 897.78 mL, p<0.001). In the multivariate logistic regression analysis, after adjustment for other variables, intraoperative bladder distention volume was found to be a statistically significant risk factor for postoperative recatheterization (hazard ratio, 1.006; confidence interval, 1.002 to 1.010; p=0.002).
Holmium laser enucleation of the prostate (HoLEP) is a safe and effective surgical procedure that significantly decreases perioperative morbidity, catheter time, and hospital stay. In addition, it provides overall functional results similar to those of transurethral resection of the prostate (TURP) and open prostatectomy [1-5]. It has recently been proposed as the new gold standard for the surgical treatment of benign prostatic hyperplasia (BPH) [3].
Recatheterization due to failure of voiding or acute urinary retention is a major complication after surgery for treatment of BPH. The incidence of recatheterization after TURP has been reported as 0.5% to 21% of patients [6-12], and that after HoLEP has been reported as 5% to 9% [12-17]. Because of increased patient discomfort, increased duration of hospitalization, and risk of secondary urinary tract infection [18] caused by the catheter, recatheterization is a complication that surgeons want to avoid.
The incidence of postoperative recatheterization could be the result of many factors. Some studies have reported an association of age, chronic urinary retention, retention volume, and maximal detrusor pressure with failure to void and recatheterization after TURP [10,19,20]. However, no study analyzing the risk factors for recatheterization after HoLEP has been reported to date.
One of the differences between TURP and HoLEP is that HoLEP requires an additional morcellation procedure. During the morcellation procedure, the bladder is frequently over-distended to prevent bladder mucosal injury. We took note of the distention of the bladder as a risk factor for postoperative voiding failure and recatheterization and began measuring the intraoperative bladder distention volume in January 2010.
In this study, we assumed that the larger the distended bladder, the more recatheterization would be required, and we evaluated the relationship between intraoperative bladder distention volume and recatheterization.
We conducted a retrospective analysis of data collected for 166 consecutive patients treated with HoLEP between January 2010 and June 2011 at the Department of Urology of the Seoul National University Hospital. All operations were performed under general anesthesia by a single surgeon (JSP) at a single center. We have been using HoLEP for the surgical management of BPH since July 2008, and we began measuring the intraoperative bladder distension volume in January 2010 after we had experienced 120 cases of HoLEP.
Patients were divided into two groups to analyze the relationship of the bladder distension volume and recatheterization. Group 1 included patients who voided successfully after removal of the catheter, and group 2 included patients who required recatheterization. Except for cases of severe hematuria, catheters were removed routinely within 24 hours of the operation. Patients who failed to void or had measured postvoid residual urine (PVR) volume greater than 300 mL were recatheterized. We excluded cases of recatheterization due to clot retention or delayed hematuria.
All perioperative clinical values were collected and compared between the two groups. Serum prostate-specific antigen (PSA) represented the last value obtained before HoLEP. Transrectal ultrasound was used for preoperative measurement of prostate volume, including total volume and transition zone volume. All patients were evaluated preoperatively by uroflowmetry and urodynamic study.
Intraoperative variables included enucleated prostate volume, enucleation time, morcellation time, used energy, and bladder distention volume. The intraoperative bladder distention volume was determined by measuring the volume of drained irrigating fluid after the morcellation procedure. Irrigating fluid pressure was approximately 60 cmH2O.
IBM SPSS ver. 19.0 (IBM Co., Armonk, NY, USA) was used in the performance of all statistical analyses. The Mann-Whitney test was used for comparison of numerical data. Binary logistic regression analysis was used for calculation of the odds ratios of risk factors. All hypotheses were evaluated in a two-sided manner, and p-values <0.05 were considered significant. Values are presented as mean±standard deviation.
Of the 166 patients with a mean age of 69.2±6.9 years, 9 patients (5.4%) required recatheterization after HoLEP. The preoperative characteristics of the patients are shown in Table 1. The patients' mean prostate volume was 60.0±22.7 mL and their mean preoperative serum PSA was 3.7±4.4 ng/mL. The patients' preoperative International Prostate Symptom Score (IPSS) and quality of life score were 19.6±7.2 and 4.2±1.1, respectively. The mean preoperative peak urinary flow rate (Qmax) and PVR on uroflowmetry were 9.1±4.2 mL/s and 69.0±106.5 mL, respectively. The results of the urodynamic study showed the patients to have a mean preoperative maximal bladder capacity of 363.6±128.3 mL. The results of a comparative analysis of the recatheterization group (group 2) with the group that did not require recatheterization (group 1) showed no significant differences in preoperative characteristics, including age, body mass index, prostate volume, or the uroflowmetry and urodynamic study parameters (Table 1).
The intraoperative values were also compared between the two groups (Table 2). Mean enucleation time was 50.0±13.8 minutes and mean morcellation time was 9.0±7.4 minutes for all patients. The mean enucleated tissue weight was equivalent to 37.5% of total prostate volume, which was measured by TRUS. No statistically significant differences in operation time, used energy, or enucleated weight were observed between the two groups. However, the value of morcellation time (which is divided by the weight of enucleated tissue) was higher in group 2 than group 1 (0.45±0.33 in group 1 vs. 0.47±0.35 in group 2, p=0.005). Also, a significantly larger intraoperative bladder distention volume was observed for group 2 than for group 1 (770.7 mL in group 1 vs. 897.8 mL in group 2, p<0.001).
In the multivariate analysis using a logistic regression model, after adjustment for other variables, the intraoperative bladder distention volume was still a statistically significant independent risk factor for postoperative recatheterization (hazard ratio, 1.006; confidence interval, 1.002 to 1.010; p=0.002).
Receiver operating characteristic (ROC) curve analysis was applied for evaluation of the power of the intraoperative bladder distention volume for prediction of recatheterization postoperatively (Fig. 1). According to the results, bladder distention volume was a good indicator of postoperative recatheterization (area under the curve, 0.780; p=0.002) with the optimal cutoff of 790 mL, which corresponded to 77.8% sensitivity and 72.9% specificity.
The findings of our study showed that the incidence of recatheterization due to voiding failure after HoLEP was approximately 5%, which is comparable with that of TURP [21], and that a larger distended volume of the bladder during the operation is related to a higher risk for recatheterization. To the best of our knowledge, no previous study of the relationship of intraoperative distention volume and recatheterization has been reported.
HoLEP has recently emerged as an attractive alternative for the treatment of BPH [3]. One of the advantages of HoLEP compared with traditional TURP is a shorter postoperative catheterization period and a shorter hospital stay in addition to a relatively bloodless operation and a decreased need for bladder irrigation [21-24]. According to several randomized studies, the mean duration of catheterization was 1.2 days shorter for HoLEP than for TURP [22-24]. Therefore, effort to decrease the incidence of recatheterization after HoLEP, which reduces the advantage of the surgery, is worthwhile.
In our study, the recatheterization rate was 5.4% (9 of 166 patients). Reports on the incidence of recatheterization after surgery for treatment of BPH have varied. Failure to void after TURP is reported to occur in 0.5% to 21% of patients [6-12]. Failure to void after HoLEP is reported to occur in 1.4% to 12.1% of patients [12-17]. In a randomized trial, the rate of recatheterization after HoLEP did not differ significantly from that after TURP [21]. Our result was also comparable with those of previous studies.
The incidence of voiding failure after prostatectomy is known to be higher in patients with BPH who have experienced acute urinary retention. The volume of retention is thought to be an important factor in predicting prognosis [10,19]. Reynard and Shearer [10] reported on the incidence of and risk factors for voiding following an initial trial without a catheter after TURP in 379 patients. Forty-five patients (12%) failed to void after TURP on the initial trial without a catheter. Six of 60 (10%) patients with acute urinary retention (painful inability to void, retention volume less than 800 mL), 15 of 55 (38%) patients with chronic retention (maintenance of spontaneous voiding, retention volume greater than 500 mL), and 20 of 65 (44%) patients with acute or chronic retention (painful retention, retention volume greater than 800 mL) failed to void after TURP. No instances of failure to void were observed in patients who presented without retention. Age and resected tissue weight showed no association with recatheterization. In a prospective study of voiding failure after TURP in patients with acute urinary retention, Djavan et al. [19] identified several risk factors. They studied 81 patients with acute urinary retention. Fourteen patients (17%) who failed to void after initial catheter removal and 11 (13%) who were unable to void at 3 to 6 months after TURP were classified as treatment failures. Significant differences regarding age (83.5 mL vs. 1,080 mL, p<0.001) and preoperative retention volume (1,780 mL vs. 1,080 mL, p<0.001), but not IPSS, PSA, or prostate volume measured by transrectal ultrasound, were observed between patients with treatment failure and those with treatment success. The results of these two studies indicate that preoperative retention volume is a predictive factor for voiding failure after TURP. However, in a study of 50 patients with acute urinary retention, Radomski et al. [20] found no significant difference in retention volume in patients who were able to void after TURP compared with those who failed to void (mean retention volume of 1,135 mL vs. 1,500 mL, p=0.058).
The relationship of preoperative acute urinary retention and postoperative voiding failure help to explain our result: that the intraoperative bladder distention volume is an independent predictor of recatheterization. This is because an intraoperative bladder distention volume larger than 790 mL could mean that transient iatrogenic urinary retention was inflicted upon patients.
The harmfulness of acute bladder over-distension had been demonstrated in several experimental animal models. In a rat model, acutely over-distended bladder shows structural modifications that alter the arrangement and interaction of collagen fibrils and incipient tissue damage as edema in the lamina propria and smooth muscle layers [25]. Shimizu et al. [26] reported that acute urinary retention results in an increase in intravesical pressure and a decrease in blood flow, resulting in intramural ischemia and nerve damage. In addition, the results of another study proved that more detrimental reperfusion damage occurs after transient urinary retention has been resolved [27].
The procedure for HoLEP consists of enucleation and morcellation procedures. HoLEP enables dissection of intact median and lateral lobes from the prostatic capsule. Once enucleation of prostatic lobes is completed, a mechanical morcellator is applied transurethrally with subsequent aspiration of the tissue from the bladder. During enucleation or morcellation procedures, bladder distention by irrigating fluid occurs and the intraoperative bladder distention volume of HoLEP is usually greater than that of traditional TURP. Such intraoperative bladder distention can cause temporary neurogenic detrusor dysfunction [25-29]. In our study, intraoperative bladder distention volume was found to be a significant risk factor for recatheterization after HoLEP. Intraoperative bladder distention volume showed a strong correlation with morcellation time and a weak correlation with Qmax and PVR in preoperative uroflowmetry. Morcellation time per enucleated prostate weight was also found to be a significant risk factor for recatheterization. Morcellation time has an important role in voiding failure after HoLEP, and we believe that an effort should be made to reduce intraoperative bladder distention and morcellation time.
Owing to the difficulty of the surgical techniques, the learning curve is an important issue when evaluating the postoperative complications of HoLEP. In our previous study, we analyzed the relationship of early postoperative complications and the learning curve. According to the results of our previous study, the recatheterization rate showed improvement with accumulation of cases; however, there was no statistical significance [30]. Before conducting the present study, we had already experienced 120 cases of HoLEP. Therefore, in the present study, the learning curve was not considered in the analysis.
This study is limited by the small number of patients, especially in the recatheterization group. For this reason, other possible risk factors with statistical significance could have been missed. However, despite the small number of patients, the intraoperative bladder distention volume was significantly higher in the recatheterization group. It was also found to be a significant risk factor in multivariate analysis, and the ROC curve indicated its usefulness as a predictor of recatheterization. According to the results of our analyses, we conclude that reducing intraoperative bladder distention volume has a significant role in preventing recatheterization after HoLEP: thus, we paid significant attention to the reduction of bladder distention volume during HoLEP. To exclude bias, patients who underwent HoLEP after the analysis were not be included in our study.
The incidence of recatheterization after HoLEP is similar to that after traditional TURP. In our study, 9 of 166 (5.4%) patients failed to void after HoLEP and required recatheterization. Intraoperative bladder distention volume and morcellation time per enucleated prostate weight are statistically significant risk factors for recatheterization after HoLEP. Therefore, an effort to reduce intraoperative bladder distention is necessary in the performance of HoLEP.
Figures and Tables
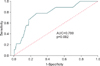 | FIG. 1Receiver operating characteristic curve analysis using intraoperative bladder distention volume to predict recatheterization after holmium laser enucleation of the prostate. AUC, area under the curve. |
References
1. Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications of transurethral resection of the prostate (TURP): incidence, management, and prevention. Eur Urol. 2006. 50:969–979.
2. Reich O, Gratzke C, Bachmann A, Seitz M, Schlenker B, Hermanek P, et al. Morbidity, mortality and early outcome of transurethral resection of the prostate: a prospective multicenter evaluation of 10,654 patients. J Urol. 2008. 180:246–249.
3. Elzayat EA, Habib EI, Elhilali MM. Holmium laser enucleation of the prostate: a size-independent new "gold standard". Urology. 2005. 66:5 Suppl. 108–113.
4. Kuntz RM, Ahyai S, Lehrich K, Fayad A. Transurethral holmium laser enucleation of the prostate versus transurethral electrocautery resection of the prostate: a randomized prospective trial in 200 patients. J Urol. 2004. 172:1012–1016.
5. Kuntz RM, Lehrich K, Ahyai SA. Holmium laser enucleation of the prostate versus open prostatectomy for prostates greater than 100 grams: 5-year follow-up results of a randomised clinical trial. Eur Urol. 2008. 53:160–166.
6. Doll HA, Black NA, McPherson K, Flood AB, Williams GB, Smith JC. Mortality, morbidity and complications following transurethral resection of the prostate for benign prostatic hypertrophy. J Urol. 1992. 147:1566–1573.
7. Thorpe AC, Cleary R, Coles J, Vernon S, Reynolds J, Neal DE. Northern Regional Prostate Audit Group. Deaths and complications following prostatectomy in 1400 men in the northern region of England. Br J Urol. 1994. 74:559–565.
8. Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Transurethral prostatectomy: immediate and postoperative complications. A cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol. 1989. 141:243–247.
9. Kim HG, Choi DY, Yoo TK. Catheter removal on the first day after transurethral prostatectomy: probability of successful voiding and its safety. Korean J Urol. 2000. 41:218–222.
10. Reynard JM, Shearer RJ. Failure to void after transurethral resection of the prostate and mode of presentation. Urology. 1999. 53:336–339.
11. Tascı AI, Ilbey YO, Tugcu V, Cicekler O, Cevik C, Zoroglu F. Transurethral resection of the prostate with monopolar resectoscope: single-surgeon experience and long-term results of after 3589 procedures. Urology. 2011. 78:1151–1155.
12. Okamura K, Nojiri Y, Seki N, Arai Y, Matsuda T, Hattori R, et al. Perioperative management of transurethral surgery for benign prostatic hyperplasia: a nationwide survey in Japan. Int J Urol. 2011. 18:304–310.
13. Du C, Jin X, Bai F, Qiu Y. Holmium laser enucleation of the prostate: the safety, efficacy, and learning experience in China. J Endourol. 2008. 22:1031–1036.
14. Kuo RL, Paterson RF, Siqueira TM Jr, Watkins SL, Simmons GR, Steele RE, et al. Holmium laser enucleation of the prostate: morbidity in a series of 206 patients. Urology. 2003. 62:59–63.
15. Gong YG, He DL, Wang MZ, Li XD, Zhu GD, Zheng ZH, et al. Holmium laser enucleation of the prostate: a modified enucleation technique and initial results. J Urol. 2012. 187:1336–1340.
16. Hwang JC, Park SM, Lee JB. Holmium laser enucleation of the prostate for benign prostatic hyperplasia: effectiveness, safety, and overcoming of the learning curve. Korean J Urol. 2010. 51:619–624.
17. Shah HN, Mahajan AP, Hegde SS, Bansal MB. Peri-operative complications of holmium laser enucleation of the prostate: experience in the first 280 patients, and a review of literature. BJU Int. 2007. 100:94–101.
18. Girou E, Rioux C, Brun-Buisson C, Lobel B. Infection Committee of the French Association of Urology. The postoperative bacteriuria score: a new way to predict nosocomial infection after prostate surgery. Infect Control Hosp Epidemiol. 2006. 27:847–854.
19. Djavan B, Madersbacher S, Klingler C, Marberger M. Urodynamic assessment of patients with acute urinary retention: is treatment failure after prostatectomy predictable? J Urol. 1997. 158:1829–1833.
20. Radomski SB, Herschorn S, Naglie G. Acute urinary retention in men: a comparison of voiding and nonvoiding patients after prostatectomy. J Urol. 1995. 153(3 Pt 1):685–688.
21. Wilson LC, Gilling PJ, Williams A, Kennett KM, Frampton CM, Westenberg AM, et al. A randomised trial comparing holmium laser enucleation versus transurethral resection in the treatment of prostates larger than 40 grams: results at 2 years. Eur Urol. 2006. 50:569–573.
22. Gilling PJ, Mackey M, Cresswell M, Kennett K, Kabalin JN, Fraundorfer MR. Holmium laser versus transurethral resection of the prostate: a randomized prospective trial with 1-year followup. J Urol. 1999. 162:1640–1644.
23. Gilling PJ, Kennett KM, Fraundorfer MR. Holmium laser resection v transurethral resection of the prostate: results of a randomized trial with 2 years of follow-up. J Endourol. 2000. 14:757–760.
24. Fraundorfer MR, Gilling PJ, Kennett KM, Dunton NG. Holmium laser resection of the prostate is more cost effective than transurethral resection of the prostate: results of a randomized prospective study. Urology. 2001. 57:454–458.
25. de Souza GM, Costa WS, Bruschini H, Sampaio FJ. Morphological analysis of the acute effects of overdistension on the extracellular matrix of the rat urinary bladder wall. Ann Anat. 2004. 186:55–59.
26. Shimizu S, Saito M, Kinoshita Y, Kazuyama E, Tamamura M, Satoh I, et al. Acute urinary retention and subsequent catheterization cause lipid peroxidation and oxidative DNA damage in the bladder: preventive effect of edaravone, a free-radical scavenger. BJU Int. 2009. 104:713–717.
27. Bratslavsky G, Kogan BA, Matsumoto S, Aslan AR, Levin RM. Reperfusion injury of the rat bladder is worse than ischemia. J Urol. 2003. 170:2086–2090.
28. Choong S, Emberton M. Acute urinary retention. BJU Int. 2000. 85:186–201.
29. Madersbacher H, Cardozo L, Chapple C, Abrams P, Toozs-Hobson P, Young JS, et al. What are the causes and consequences of bladder overdistension? ICI-RS 2011. Neurourol Urodyn. 2012. 31:317–321.
30. Bae J, Oh SJ, Paick JS. The learning curve for holmium laser enucleation of the prostate: a single-center experience. Korean J Urol. 2010. 51:688–693.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download