Abstract
Purpose
To compare surgical outcomes and complications after percutaneous nephrolithotomy (PCNL) under regional or general anesthesia.
Materials and Methods
One hundred and one patients who underwent PCNL as a first-line treatment for kidney calculi between June 2004 and June 2013 were enrolled in this retrospective study. Patients were classified into two groups by anesthetic method: 77 were allocated to the regional anesthesia group and 24 to the general anesthesia group. Patient general characteristics, stone features, surgical outcomes, and complications were compared between the two groups.
Results
The two groups were similar in terms of mean age and stone size, number, and type. Furthermore, they did not differ significantly in terms of general characteristics, treatment outcomes, or complications excluding postoperative fever. However, mean hospital stay was significantly shorter in the regional anesthesia group than in the general anesthesia group (8.9±3.2 days vs. 11.5±6.9 days, respectively, p=0.025). Also, the postoperative fever rate was significantly higher in the general anesthesia group (53.2% vs. 83.3%, respectively, p=0.007).
Go to : 
Various modalities, such as percutaneous nephrolithotomy (PCNL), extracorporeal shock wave lithotripsy, and retrograde intrarenal surgery, are used to manage renal stone disease [1-3]. However, PCNL is regarded as the treatment of choice for most renal stones, especially for patients with a large renal stone (>2 cm), an infected stone, or a cystine stone and for those with a history of failed shock wave lithotripsy [4,5].
General anesthesia during PCNL has many advantages, for example, it enables breathing control and improves patient comfort [6]. Thus, at most experienced centers, PCNL is usually performed under general anesthesia [7]. However, associated complications and cost are higher for general anesthesia than for regional anesthesia [8]. For example, endotracheal tube migration and neurologic problems, particularly at the time of position transition, may arise during PCNL under general anesthesia [9]. Unfortunately, few research studies have been conducted to compare regional and general anesthesia with respect to operative parameters [10]. In the present study, therefore, to determine whether PCNL under regional anesthesia is a better alternative than PCNL under general anesthesia, we examined surgical outcomes after these two procedures.
Go to : 
One hundred and one consecutive patients who underwent PCNL as a first-line management for renal stones, including staghorn, pelvic, and calyceal stones, from June 2004 to June 2013 at Inje University Sanggye Paik Hospital were included in this retrospective study. This study was conducted according to the Declaration of Helsinki [11]. The patients were classified into two groups by anesthesia method: a regional anesthesia group (n=77) and a general anesthesia group (n=24). Decisions regarding anesthesia method were mainly based on considerations of medical status, such as cardiac problems and the presence of respiratory illness or coagulopathy. In the absence of such factors, regional anesthesia was performed on the basis of surgeon or patient preference. The contraindications for PCNL were uncorrected coagulopathy, congenital renal anomaly, and metastatic malignancy.
In addition to history taking, we performed a physical examination, preoperative laboratory tests, and a radiological evaluation, which included plain radiography of the kidney-ureter-bladder (KUB) region and abdominopelvic computed tomography (CT). Stone size was defined as the sum of the maximal lengths of renal stones on CT images. Patients with a urinary tract infection were treated preoperatively in accordance with urine culture sensitivity. The clinical and stone parameters compared were age, gender, body mass index, stone laterality, stone size, and stone number, respectively.
Regional anesthesia was induced with 0.5% heavy bupivacaine (Marcaine, Astrazeneca Korea, Seoul, Korea) 12 mL, and a spinal epidural set (Portex, Smiths medical, Kent, UK) was injected intrathecally into the L3-4 or L4-5 interspaces. The level of anesthesia was checked for 5 minutes after injection with the patient in the Trendelenburg position. If surgery was prolonged, levobupivacaine (Chirocaine, Abbott Korea, Seoul, Korea) was administered by an anesthesiologist to maintain adequate anesthesia. General anesthesia was carried out by using intravenous propofol (Pofol, Dongkook pharmaceutical Co., Seoul, Korea) and rocuronium (Esmeron, MSD Korea, Seoul, Korea).
Following the induction of anesthesia, patients were placed in the lithotomy position. An occlusion ureteral catheter was then inserted into the renal pelvis and ballooning (1 mL) was performed to prevent stone fragments from descending into the proximal ureter. Patients were then rotated to the prone position and percutaneous nephrostomy was performed under ultrasonographic guidance. The access tract was dilated with an Amplatz and a balloon dilator, and stone fragmentation was performed by using a combination of ultrasonic and pneumatic lithotripsy. Stone fragments were removed by using grasping forceps under a 24-Fr nephroscope. A 20-Fr nephrostomy tube was left and a fluoroscopic nephrostogram was routinely obtained to assess status at the end of the procedure.
Patients in both groups were radiologically followed up at 1 day (initial) and 1 month (overall) after surgery to assess status. Stone-free status was defined as the absence of any fragment greater than 4 mm by KUB. When stones were radiolucent, dimensions were obtained by ultrasonography. Operative outcomes, surgical times, hospital stays, stone-free rates, perioperative complications, and changes in hemoglobin and white blood cell counts were compared by using the modified Clavien grading system, which was proposed to grade perioperative complications of general surgery and has been validated in a cohort of 6,336 patients [12].
Fever was defined as a temperature exceeding 37.7℃ at 1,600 on the first postoperative day [13]. Postoperative antipyretics (Arthagyl, Ilyang pharmaceutical Co., Seoul, Korea), analgesics (Tridol, Yuhan Co., Seoul, Korea), antiemetics (Mexolon, DongA Pharm, Seoul, Korea), and diuretics (Lasix, Handok Inc., Seoul, Korea) were injected intravenously when symptoms appeared during the operative or first postoperative day. Blood transfusions were done in the operating room on the basis of decisions made by anesthesiologists.
Statistical analysis was performed by using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). Because the number of patients in the general anesthesia group was small (n=24), continuous variables were assessed by using the Mann-Whitney test, and categorical variables were analyzed by using the chi-square test. Clinical parameters are expressed as mean±standard deviations, and statistical significance was accepted for p-values <0.05.
Go to : 
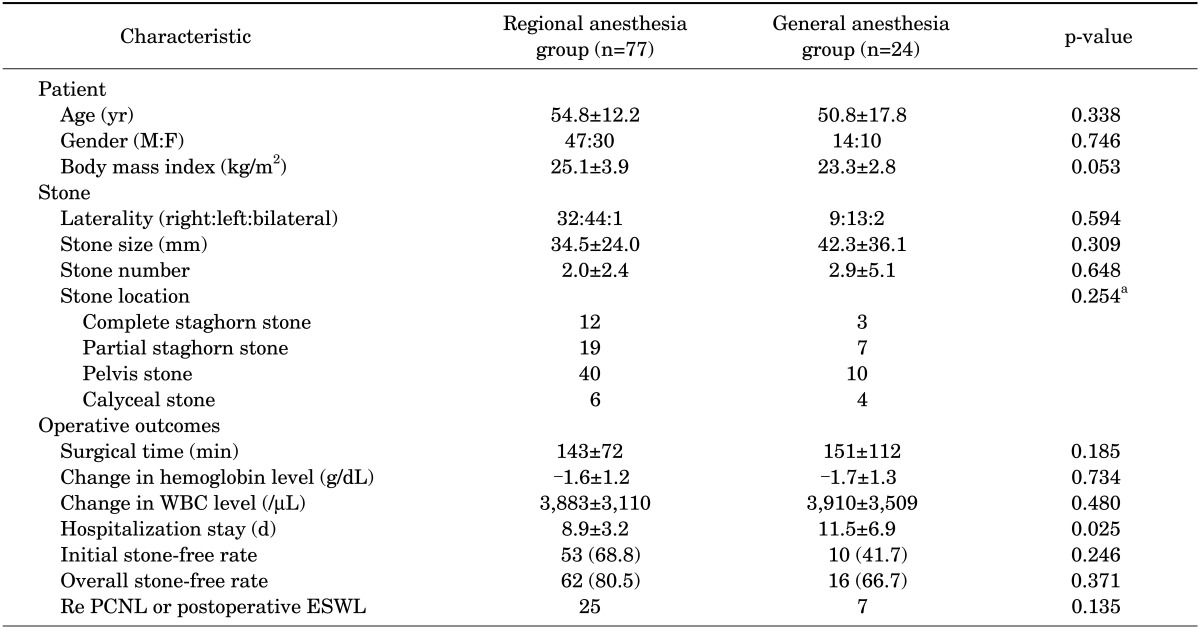
Patient and stone characteristics in the regional and general anesthesia groups are compared in Table 1. Mean ages in these groups were 54.8±12.2 years and 50.8±17.8 years, respectively (p=0.338). Gender and body mass index were nonsignificantly different, and mean stone sizes (34.5±24.0 mm and 42.3±36.1 mm, respectively; p=0.309), mean stone numbers (2.0±2.4 and 2.9±5.1, respectively; p=0.648), and the distributions of renal stones were similar (p=0.254).
Operative outcomes are summarized in Table 1. Intergroup differences between initial stone-free rates (68.8% and 41.7%, respectively; p=0.246) and overall stone-free rates (80.5% and 66.7%, respectively; p=0.371) were nonsignificantly different. No significant intergroup differences were found between mean surgical times (143±72 minutes and 151±112 minutes, respectively; p=0.185) or changes in hemoglobin levels (-1.6±1.2 g/dL and -1.7±1.3 g/dL, respectively; p=0.734) in the regional and general anesthesia groups. Furthermore, white blood cell levels were not significantly changed in the two groups (3,883±3,110/µL and 3,910±3,509/µL, respectively; p=0.480). However, mean hospital stay was significantly shorter in the regional anesthesia group (8.9±3.2 days vs. 11.5±6.9 days, respectively; p=0.025).
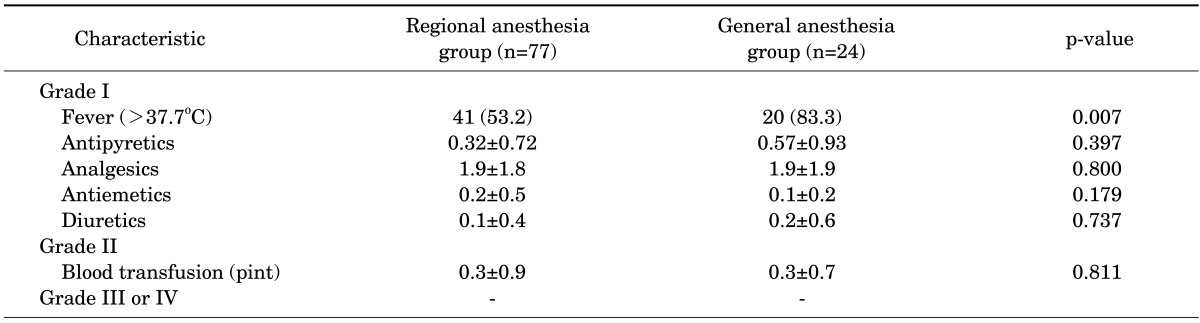
Perioperative complications were investigated by using the modified Clavien grading system, and the results are summarized in Table 2. A smaller proportion of patients in the regional anesthesia group experienced postoperative fever (p=0.007). However, mean dosages of antipyretics (p=0.397), analgesics (p=0.800), antiemetics (p=0.179), and diuretics (p=0.737) administered were not significantly different. Furthermore, the mean number of pints of blood transfused per patient was similar in the two groups (0.3±0.9 vs. 0.3±0.7, respectively; p=0.811). No patient experienced a grade III or IV complication according to the modified Clavien grading system.
Go to : 
PCNL remains the first-line treatment of choice for managing renal stone disease, although minimally invasive modalities, such as retrograde intrarenal surgery, have been introduced [4,5]. Furthermore, most urologists prefer general anesthesia for PCNL owing to the high level of anesthesia achieved, the ability to control the patient's breathing, and because it is more comfortable for patients [7,14]. However, general anesthesia is more likely to cause severe morbidities, such as drug-induced anaphylaxis, complications associated with endotracheal tube insertion, and cardiovascular, pulmonary, and neurologic complications, than is regional anesthesia [15].
Studies have been conducted to demonstrate the benefits of regional anesthesia in other types of surgery, such as radical retropubic prostatectomy [16] and total hip arthroplasty [17]. Salonia et al. [16] asserted that regional anesthesia permits fine muscle relaxation and achieves excellent surgical outcomes after radical retropubic prostatectomy. Furthermore, regional anesthesia has been reported to reduce the risk of intraoperative hemorrhage, to be associated with less postoperative pain, and to allow earlier restoration than general anesthesia [18-20]. In addition, Gonano et al. [21] reported that the cost of regional anesthesia is 40% less than that of general anesthesia during orthopedic surgeries.
Several comparative studies on anesthesia methods in PCNL have demonstrated various benefits for PCNL under regional anesthesia compared with general anesthesia. In a retrospective comparative study of 37 patients who underwent regional anesthesia and 45 who underwent general anesthesia, it was concluded that the results were comparable in terms of general profiles, operative times, and stone-free rates [14]. In another study of 50 patients who underwent PCNL, regional anesthesia was found to be associated with greater patient satisfaction, less early postoperative pain, and fewer adverse events than general anesthesia [15]. Furthermore, in a prospective randomized study on PCNL in 64 patients (32 general and 32 regional anesthesia), patients in the regional anesthesia group were found to have significantly lower postoperative analgesic demands and shorter hospitalization periods [7]. Corbel et al. [22] reported that general anesthesia increases the probabilities of fluid absorption and electrolyte imbalance, and other authors have recommended regional anesthesia for patients with an electrolyte imbalance, especially for morbidly obese patients [2,23].
Despite the opinion held by some that regional anesthesia is unsuitable for PCNL of calculi in the upper pole of the kidney [24], regional anesthesia (bupivacaine [Marcaine], 12-15 mg) can be used to anesthetize up to the T4 level (level of axilla) according to an anesthesiology textbook [25]. Furthermore, this allows enough access to the supracostal and intercostals from this level.
General anesthesia is associated with significant changes in the shape of the chest and alveolar gas contents. This process results in atelectasis and postoperative fever. Outside of that, these changes result in continued elevation of the risk for reintubation, mechanical ventilation, and nosocomial pneumonia, all of which prolong the hospital stay [26].
Regarding hospital stay, it was previously reported that average hospital stay is approximately 5 to 7 days regardless of anesthesia type [27]. However, in the present study, hospital stays were 8.9±3.2 days and 11.5±6.9 days, respectively, which could have been due to the exclusion of time spent at the hospital before surgery and the procedure used to determine the discharge date.
In addition, according to a large-scale study, initial and overall stone-free rates were 69.9% and 88.8%, respectively [27], and another study conducted on 610 patients found corresponding rates of 57.6% and 84.9%, respectively [28]. In the present study, values were 68.8% and 80.5% in the regional anesthesia group and 42.9% and 71.4% in the general anesthesia group, which were relatively low and did not represent a significant intergroup difference. We attribute these differences to the different definitions used for the stone-free rate and patient descriptive features.
In brief, this retrospective study showed that despite similar patient characteristics in the two groups, postoperative fever rates and hospital stays were significantly greater in the general anesthesia group. Thus, it may be more helpful for patients to implement PCNL under regional anesthesia than general anesthesia in matters of fever control and cost of hospitalization.
The present study had some limitations that deserve mention. First, it was inherently limited by its retrospective design; as such, lack of control of basic patient factors may have introduced bias. Second, the study was performed at a single center, and the general anesthesia group was appreciably smaller than the regional anesthesia group. Third, no attempt was made to assess patient satisfaction with treatment. Accordingly, we suggest that a prospective study is needed to confirm our results.
Go to : 
The present study showed that in terms of general characteristics and procedural success, the outcomes of PCNL conducted by use of regional or general anesthesia are similar. Nevertheless, PCNL with regional anesthesia required fewer hospital days and was associated with a lower postoperative fever rate. Accordingly, we conclude that PCNL under regional anesthesia is at least as advantageous as PCNL under general anesthesia in patients with kidney calculi.
Go to : 
References
1. Al-Kohlany KM, Shokeir AA, Mosbah A, Mohsen T, Shoma AM, Eraky I, et al. Treatment of complete staghorn stones: a prospective randomized comparison of open surgery versus percutaneous nephrolithotomy. J Urol. 2005; 173:469–473. PMID: 15643212.

2. Preminger GM, Assimos DG, Lingeman JE, Nakada SY, Pearle MS, Wolf JS Jr. Chapter 1: AUA guideline on management of staghorn calculi: diagnosis and treatment recommendations. J Urol. 2005; 173:1991–2000. PMID: 15879803.

3. Fernstrom I, Johansson B. Percutaneous pyelolithotomy: a new extraction technique. Scand J Urol Nephrol. 1976; 10:257–259. PMID: 1006190.
4. Stening SG, Bourne S. Supracostal percutaneous nephrolithotomy for upper pole caliceal calculi. J Endourol. 1998; 12:359–362. PMID: 9726403.

5. Lojanapiwat B, Prasopsuk S. Upper-pole access for percutaneous nephrolithotomy: comparison of supracostal and infracostal approaches. J Endourol. 2006; 20:491–494. PMID: 16859462.

6. Jun-Ou J, Lojanapiwat B. Supracostal access: does it affect tubeless percutaneous nephrolithotomy efficacy and safety? Int Braz J Urol. 2010; 36:171–176. PMID: 20450501.

7. El-Husseiny T, Moraitis K, Maan Z, Papatsoris A, Saunders P, Golden B, et al. Percutaneous endourologic procedures in high-risk patients in the lateral decubitus position under regional anesthesia. J Endourol. 2009; 23:1603–1606. PMID: 19747056.

8. Kuzgunbay B, Turunc T, Akin S, Ergenoglu P, Aribogan A, Ozkardes H. Percutaneous nephrolithotomy under general versus combined spinal-epidural anesthesia. J Endourol. 2009; 23:1835–1838. PMID: 19630480.

9. Barak M, Putilov V, Meretyk S, Halachmi S. ETView tracheoscopic ventilation tube for surveillance after tube position in patients undergoing percutaneous nephrolithotomy. Br J Anaesth. 2010; 104:501–504. PMID: 20185518.

10. Singh V, Sinha RJ, Sankhwar SN, Malik A. A prospective randomized study comparing percutaneous nephrolithotomy under combined spinal-epidural anesthesia with percutaneous nephrolithotomy under general anesthesia. Urol Int. 2011; 87:293–298. PMID: 21921573.

11. Reynolds T. Declaration of Helsinki revised. J Natl Cancer Inst. 2000; 92:1801–1803. PMID: 11078756.

12. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213. PMID: 15273542.
13. Kasper DL, Braunwald E, Hauser S, Fauci AS, Longo D, Jameson JL, et al. Harrison's principle of internal medicine. 16th ed. London: McGrawhill;2005.
14. Trivedi NS, Robalino J, Shevde K. Interpleural block: a new technique for regional anaesthesia during percutaneous nephrostomy and nephrolithotomy. Can J Anaesth. 1990; 37(4 Pt 1):479–481. PMID: 2340620.

15. Tangpaitoon T, Nisoog C, Lojanapiwat B. Efficacy and safety of percutaneous nephrolithotomy (PCNL): a prospective and randomized study comparing regional epidural anesthesia with general anesthesia. Int Braz J Urol. 2012; 38:504–511. PMID: 22951179.

16. Salonia A, Suardi N, Crescenti A, Colombo R, Rigatti P, Montorsi F. General versus spinal anesthesia with different forms of sedation in patients undergoing radical retropubic prostatectomy: results of a prospective, randomized study. Int J Urol. 2006; 13:1185–1190. PMID: 16984550.

17. Maurer SG, Chen AL, Hiebert R, Pereira GC, Di Cesare PE. Comparison of outcomes of using spinal versus general anesthesia in total hip arthroplasty. Am J Orthop (Belle Mead NJ). 2007; 36:E101–E106. PMID: 17694193.
18. Shir Y, Raja SN, Frank SM, Brendler CB. Intraoperative blood loss during radical retropubic prostatectomy: epidural versus general anesthesia. Urology. 1995; 45:993–999. PMID: 7771032.

19. Faas CL, Acosta FJ, Campbell MD, O'Hagan CE, Newton SE, Zagalaniczny K. The effects of spinal anesthesia vs epidural anesthesia on 3 potential postoperative complications: pain, urinary retention, and mobility following inguinal herniorrhaphy. AANA J. 2002; 70:441–447. PMID: 12526149.
20. Davis FM, McDermott E, Hickton C, Wells E, Heaton DC, Laurenson VG, et al. Influence of spinal and general anaesthesia on haemostasis during total hip arthroplasty. Br J Anaesth. 1987; 59:561–571. PMID: 3107600.

21. Gonano C, Leitgeb U, Sitzwohl C, Ihra G, Weinstabl C, Kettner SC. Spinal versus general anesthesia for orthopedic surgery: anesthesia drug and supply costs. Anesth Analg. 2006; 102:524–529. PMID: 16428554.

22. Corbel L, Guille F, Cipolla B, Staerman F, Leveque JM, Lobel B. Percutaneous surgery for lithiasis: results and perspectives. Apropos of 390 operations. Prog Urol. 1993; 3:658–665. PMID: 8401627.
23. Aravantinos E, Karatzas A, Gravas S, Tzortzis V, Melekos M. Feasibility of percutaneous nephrolithotomy under assisted local anaesthesia: a prospective study on selected patients with upper urinary tract obstruction. Eur Urol. 2007; 51:224–227. PMID: 16842905.

24. Mehrabi S, Mousavi Zadeh A, Akbartabar Toori M, Mehrabi F. General versus spinal anesthesia in percutaneous nephrolithotomy. Urol J. 2013; 10:756–761. PMID: 23504678.
25. Miller RD, Pardo MC Jr. Basics of anesthesia. 6th ed. Philadelphia: Elsevier;2011.
26. Neligan PJ. Postoperative noninvasive ventilation. Anesthesiol Clin. 2012; 30:495–511. PMID: 22989591.

27. Shin TS, Cho HJ, Hong SH, Lee JY, Kim SW, Hwang TK. Complications of percutaneous nephrolithotomy classified by the modified Clavien grading system: a single center's experience over 16 years. Korean J Urol. 2011; 52:769–775. PMID: 22195267.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download