Abstract
Purpose
We retrospectively investigated the effect of transurethral resection of the prostate (TURP) on the basis of the degree of obstruction seen in preoperative urodynamic study in patients with benign prostatic hyperplasia (BPH) who complained of lower urinary tract symptoms (LUTS).
Materials and Methods
The subjects of this study were 285 patients who were diagnosed with BPH with LUTS and who subsequently underwent TURP. The Abrams-Griffiths number was calculated from the urodynamic results to divide the patients into the following groups: unobstructed, equivocal, and obstructed. There were 26 patients (9.1%) in the unobstructed group, 98 patients (34.4%) in the equivocal group, and 161 patients (56.5%) in the obstructed group. The preoperative and postoperative uroflowmetry, residual urine, International Prostate Symptom Score (IPSS), and quality of life (QoL) score were compared between the three groups to evaluate the outcome of the treatment.
Results
The reduction in the IPSS was 14.4 in the obstructed group, which was higher than the reductions of 12.7 in the equivocal group and 9.5 in the unobstructed group, but this difference was not statistically significant (p=0.227). The QoL score was also not significantly different across the three groups (p=0.533). The postoperative maximum flow rate was significantly improved in all three groups. The obstructed group had an improvement of 7.8±7.2 mL/s, which was higher than the improvement of 3.7±6.2 mL/s in the unobstructed group (p=0.049) but was not significantly different from the improvement of 5.6±6.9 mL/s in the equivocal group (p=0.141).
Lower urinary tract symptoms (LUTS) are the most common urological condition seen in elderly males, the main cause of which is benign prostatic hyperplasia (BPH) leading to bladder outlet obstruction (BOO) [1,2]. The most widely used surgical treatment for BPH with LUTS is transurethral resection of the prostate (TURP). Various tests can be used to subjectively assess the degree of preoperative LUTS. Of these, the International Prostate Symptom Score (IPSS) and urodynamic study are the most used. The IPSS is a method to quantify LUTS, and although it is limited by its subjectivity for each patient, its advantage is that it is a noninvasive method that can readily be used in the outpatient setting [3]. Urodynamic study, on the other hand, is more invasive, time-consuming, and costly and thus its need is debatable. However, it is one of the most accurate methods for identifying the cause of LUTS and for describing the symptoms objectively [4].
It is possible to assess the presence of BOO by using pre-TURP urodynamic study. It is known that those with BOO tend to have more successful operative outcomes, whereas those without BOO have lower success rates [5,6]. Yet, Van Venrooij et al. [7] reported that LUTS had improved after TURP in patients who were found to be unobstructed or equivocal in preoperative urodynamic study.
The urodynamic study is the most trustworthy test for objectively assessing the cause and symptoms of LUTS in BPH. However, the effect of TURP for LUTS without BOO has not been clearly identified. We therefore investigated the effect of BOO in preoperative urodynamic studies on the outcome of TURP in BPH patients with LUTS.
The subjects of this retrospective study were 285 patients of the 338 who visited Eulji General Hospital between 2006 and 2011 for LUTS who were subsequently diagnosed with BPH, underwent TURP, and could be followed up for more than 3 months. We included those who had an IPSS of at least 12, with a maximum urine flow of less than 15 mL/s. The mean age of the patients was 69.1 years (range, 50 to 86 years). All patients underwent preoperative urodynamic study and had their histories taken, as well as a physical examination, urine test, prostate ultrasonography, and assessment of IPSS, quality of life (QoL), and prostate-specific antigen (PSA). The patients were assessed 3 months after the operation by use of the IPSS, QoL, uroflowmetry, and residual urine tests.
The extent of BOO of the patients was assessed by calculating the Abrams-Griffiths (AG) number and the information gained from the preoperative urodynamic study [8].
AG number = [PdetQmax-(2×Qmax)]
where PdetQmax is detrusor pressure at maximum flow and Qmax is maximum flow. Patients with an AG number greater than 40 were classified into the obstructed group, whereas those with an AG number between 20 and 40 were placed in the equivocal group and those with an AG number less than 20 were placed in the unobstructed group. The bladder contractility index (BCI) was calculated as PdetQmax+5Qmax, and detrusor underactivity (DU) was defined as BCI<100. Indication for operation in the unobstructed group was persistent symptoms even after medication for longer than 3 months. Those who had a history of neurogenic bladder, prostate cancer, urethral strictures, or recurrent urinary tract infections were excluded from this study. In addition, patients with an acontractile detrusor in urodynamic study were excluded.
There were 26 patients in the unobstructed group (9.1%) with a mean age of 69.0 years (range, 50 to 82 years), 98 patients in the equivocal group (34.4%) with a mean age of 68.5 years (range, 51 to 84 years), and 161 patients in the obstructed group (56.5%) with a mean age of 69.8 years (range, 50 to 83 years). The preoperative and postoperative uroflowmetry, residual urine test, IPSS, and QoL variables were compared between the groups to evaluate the outcome of the treatment. Depending on the symptoms, the IPSS questions were divided into those asking about voiding symptoms, such as incomplete voiding, intermittency, weak stream, and hesitancy (questions 1, 3, 5, and 6), and those asking about storage symptoms, such as frequency, urgency, and nocturia (questions 2, 4, and 7), and the scores were compared.
The difference between the clinical markers of each comparison group were compared by using analysis of variance with SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA), and the Bonferroni test was used for post-hoc analysis. A p-value of 0.05 or less was taken to have statistical significance.
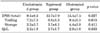
There were no significant differences in age or PSA level across the three groups. The mean prostate volume in the obstructed group was 61.6±26.7 g, which was significantly larger than that of the unobstructed group (43.8±21.2 g) and the equivocal group (44.8±19.8 g) (p<0.001). The preoperative IPSS was 22.8±7.9 in the unobstructed group, 22.4±6.1 in the equivocal group, and 23.4±6.9 in the obstructed group (p=0.567). There was no significant difference in the voiding symptoms or storage symptoms between the three groups. For the QoL assessment, the unobstructed, equivocal, and obstructed groups scored 4.4±1.2, 4.5±1.0, and 4.5±1.1, respectively (p=0.926) (Table 1). The maximum flow rate in the unobstructed group was 9.5±3.2 mL/s, which was not significantly different from that of the equivocal group (9.2±3.4 mL/s, p=0.420) but was higher than that of the obstructed group (8.2±3.3 mL/s, p=0.045). The voided volume of the unobstructed group was 198.9±127.7 mL, which was not significantly different from that of the equivocal group (192.1±114.1 mL) but was greater than that of the obstructed group (158.9±92.1 mL). The BCI of the unobstructed group was 81.9±19.5, which was not significantly different from that of the equivocal group (87.7±21.9) but was smaller than that of the obstructed group (115.6±32.5). DU was identified 21 patients (80.8%) in the unobstructed group and 51 patients (31.7%) in the obstructed group (Table 2).
The IPSS had decreased to 9.1±7.8 postoperatively from a preoperative score of 22.8±7.9 in the unobstructed group, whereas the score in the equivocal group had decreased from 22.4±6.1 to 8.6±4.5 and that in the obstructed group had decreased from 23.4±6.9 to 8.1±5.4. The reduction in the IPSS in the obstructed group was 14.4, which was greater than the reduction in the equivocal group (12.7) or the unobstructed group (9.5), but this difference was not statistically significant (p=0.227). Dividing the IPSS into voiding and storage symptoms, the reduction in voiding symptom scores in the obstructed group was 9.4, compared with 8.8 in the equivocal group and 7.2 in the unobstructed group. However, this difference was not statistically significant (p=0.615). The reduction in storage symptom scores in the obstructed group was 4.4, compared with 3.7 in the equivocal group and 2.3 in the unobstructed group (p=0.411) (Table 3). The QoL score decreased by 2.2, from 4.4±1.2 preoperatively to 1.7±1.2 postoperatively, in the unobstructed group. In the equivocal group the score was reduced by 2.7 from 4.5±1.0 to 1.8±1.2, and in the obstructive group it was reduced by 2.9 from 4.5±1.1 to 1.5±1.0. There was no statistical difference in the reduction in QoL score between the three groups (p=0.533) (Table 3).
The maximum flow rate was increased postoperatively in all three groups. The improvement in maximum flow rate was greater in the obstructed group (7.8±7.2 mL/s) than in the unobstructed group (3.7±6.2 mL/s, p=0.049) but was not significantly different from that of the equivocal group (5.6±6.9 mL/s, p=0.141) (Table 4). The number of patients with improved Qmax of more than 20% from baseline was 20 (76.9%) in the unobstructed group, 89 (90.8%) in the equivocal group, and 150 (93.2%) in the obstructed group. The improvement in maximum flow rate was 6.4±5.0 mL/s, 7.4±5.7 mL/s, and 9.2±6.4 mL/s in the unobstructed group, equivocal group, and obstructed group, respectively (p=0.141).
LUTS become more prevalent with increasing age, and the causes include age, bladder dysfunction, infection, and BPH [9]. The prevalence of BPH increases after the age of 50. Of the various causes of LUTS, it is believed that BOO is the main cause in BPH patients [10]. Yet, one cannot say that all BPH patients have BOO. Abrams et al reported that 70% of BPH patients have BOO, whereas Lee et al. [11] reported that only 51% of 100 BPH patients with LUTS had confirmed BOO after urodynamic studies [6]. Seo et al. [12] reported that preoperative urodynamic study revealed that 81% of patients with LUTS for which they received TURP had obstruction, whereas the remaining 19% were unobstructed. Similar to these findings, of the 285 patients in this study, 161 (56.5%) were found to be obstructed, whereas 98 (34.4%) were equivocal and the remaining 26 (9.1%) were unobstructed.
The degree of BOO in BPH patients can vary, but the LUTS that patients complain of do not seem to correlate with the presence of BOO. Chung et al. [13] reported that the IPSS in BPH patients with BOO was 27.2, whereas the score in those without BOO was 24.6, showing no significance difference. The QoL score was also not statistically different between the two groups. Similarly, in this study, the IPSS was 22.8 in the unobstructed group, 22.4 in the equivocal group, and 23.4 in the obstructed group, showing no significant difference. The QoL score was 4.1 in the unobstructed group, 4.4 in the equivocal group, and 4.3 in the obstructed group, showing no significant difference. These results suggest that the patients with BPH who complain of LUTS but who are found to have no BOO in urodynamic studies may have symptom severity comparable to that of patients with BOO.
TURP can be said to be the safest and most effective treatment for BPH patients who complain of LUTS [14,15]. Yet, although the success rate of TURP is relatively high, a subset of patients continue to have symptoms even after the operation. Poor TURP outcome is not related to the prostate volume or the symptom score, but is reported to be associated with older age, high residual urine volume, and detrusor pressure during voiding [16-18]. Uroflowmetry is most frequently used to indirectly measure the contraction of the detrusor muscles to check for the presence of BOO, but its efficacy has been debated [19]. Uroflowmetry alone cannot distinguish between BOO and detrusor muscle dysfunction, which poses a need for urodynamic study. Of the various urodynamic study components, the pressure-flow test can measure the maximum flow rate and the voiding pressure simultaneously to deliver an objective diagnosis of BOO. The presence of BOO in pre-TURP urodynamic study is an important factor that affects the treatment outcome.
Robertson et al. [20] reported that whereas 79% of BPH patients who had BOO preoperatively had successful surgical outcomes, only 55% without BOO had symptomatic improvement after the operation. Seo et al. [12] also suggested that the surgical success rate of patients who had BOO was 87.2%, which was higher than the success rate of 63.6% of patients without BOO. Thus, it can be said that the postoperative success rate and patient satisfaction is higher in patients who have confirmed BOO in preoperative urodynamic study. However, other studies reported that TURP is still an effective treatment for patients without BOO. Van Venrooij et al. [7] showed that unobstructed and equivocal patients were found to have increased bladder volume and reduced residual urine volume, as well as an improvement in LUTS, thus suggesting that TURP is effective in patients without BOO. In addition, Chung et al. [13] reported that although patients without BOO had smaller IPSS improvement than did those with BOO, the scores in the former patients were reduced from 24.6 to 14.0, showing a significant decrease. The QoL score in patients with BOO was reduced by 2.9, whereas the score in patients without BOO was reduced by 2.2, showing no statistically significant difference between these two groups.
The present study also confirmed that TURP was effective in patients without BOO. The total IPSS decreased after the operation in all three groups of BPH patients. The obstructive group, unobstructed group, and the equivocal group showed decreases of 14.4, 12.7, and 9.5, respectively, which were not significantly different. The voiding symptom score and storage symptom score of the IPSS were not significantly different between the three groups. For the QoL score, the obstructed, equivocal, and unobstructed groups scored 2.9, 2.7, and 2.2, respectively, with no statistically significant difference between the groups. The number of patients with improved Qmax of more than 20% from baseline was 20 (76.9%) in the unobstructed group, 89 (90.8%) in the equivocal group, and 150 (93.2%) in the obstructed group. Furthermore, there was no significant difference in improvement in maximum flow rate between the three groups. Whereas the patients without preoperative BOO had less improvement in the maximum flow rate than did those with preoperative BOO, the improvement of LUTS was not significantly different between these two groups of patients.
Han et al. [21] explained the effect of TURP in patients without BOO by suggesting that patients with weaker detrusor contractility during pressure-flow study may not be diagnosed with obstruction because of an insufficient increase in detrusor pressure. They reported that TURP can treat the obstruction undiagnosed in the pressure-flow study to improve LUTS. A study by van Venrooij et al. [22], which compared patients with BOO with patients without BOO by using pre-TURP and 6-month postoperative urodynamic study, showed that the urethral resistance factor was reduced by 70% in the obstructed group, whereas the equivocal and the unobstructed groups also had a 40% reduction. The findings of van Venrooij et al. [22] suggest that the reduction in urethral resistance postoperatively can increase the maximum flow rate in patients without BOO. Those authors suggested that although the increase in the maximum flow rate after TURP was lower in the unobstructed group than in the obstructed group, this increase was significant enough to lead to an improvement in the LUTS. In the present study, the improvement in the maximum flow rate in the unobstructed and the equivocal groups was lower than that of the obstructed group, but still significant, and the IPSS and the QoL scores had also decreased significantly. This finding suggests that in the unobstructed patients with weak detrusor contractility, it was possible to reduce urethral resistance with TURP, so that the LUTS symptoms were improved in the unobstructed group. However, there was no significant difference in preoperative parameters between improved patients and unimproved patients in the unobstructed group. This is because the number of unobstructed patients was too small; therefore, further studies may be required.
Because the causes of LUTS vary widely, it is difficult to explain them with BOO alone. The extent of detrusor contraction and detrusor hyperactivity should also be considered with BOO in urodynamic study to provide a more accurate prognosis. A limitation of this study is that we only assessed the effect of BOO found in the urodynamic studies on the surgical outcome.
The presence of BOO in BPH patients who complain of LUTS will most likely result in good TURP outcome. However, patients without BOO can also expect post-TURP improvement in maximum flow rate and LUTS. Therefore, TURP can be said to be an effective treatment modality for BPH patients with LUTS, both with and without BOO.
In this study, BPH patients with LUTS but without BOO in urodynamic study showed an improvement in maximum flow rate and LUTS after TURP, although not to the same extent as those who had BOO before TURP. Therefore, TURP can be an effective treatment that leads to symptomatic relief of LUTS in BPH patients, even those without BOO.
Figures and Tables
References
1. Chapple CR, Roehrborn CG. A shifted paradigm for the further understanding, evaluation, and treatment of lower urinary tract symptoms in men: focus on the bladder. Eur Urol. 2006; 49:651–658.
2. Chaikin DC, Blaivas JG. Voiding dysfunction: definitions. Curr Opin Urol. 2001; 11:395–398.
3. Cho HJ, Kang JY, Yoo TK. The International Prostate Symptom Score: discrepancies between self-administration and physician-administration. Korean J Urol. 2007; 48:500–504.
4. Steele GS, Sullivan MP, Sleep DJ, Yalla SV. Combination of symptom score, flow rate and prostate volume for predicting bladder outflow obstruction in men with lower urinary tract symptoms. J Urol. 2000; 164:344–348.
5. Rollema HJ, Van Mastrigt R. Improved indication and followup in transurethral resection of the prostate using the computer program CLIM: a prospective study. J Urol. 1992; 148:111–115.
6. Abrams P. Objective evaluation of bladder outlet obstruction. Br J Urol. 1995; 76:Suppl 1. 11–15.
7. Van Venrooij GE, Van Melick HH, Eckhardt MD, Boon TA. Correlations of urodynamic changes with changes in symptoms and well-being after transurethral resection of the prostate. J Urol. 2002; 168:605–609.
8. Eckhardt MD, van Venrooij GE, Boon TA. Urethral resistance factor (URA) versus Schäfer's obstruction grade and Abrams-Griffiths (AG) number in the diagnosis of obstructive benign prostatic hyperplasia. Neurourol Urodyn. 2001; 20:175–185.
9. Thomas AW, Abrams P. Lower urinary tract symptoms, benign prostatic obstruction and the overactive bladder. BJU Int. 2000; 85:Suppl 3. 57–68.
10. Peters TJ, Donovan JL, Kay HE, Abrams P, de la Rosette JJ, Porru D, et al. The International Continence Society "Benign Prostatic Hyperplasia" Study: the botherosomeness of urinary symptoms. J Urol. 1997; 157:885–889.
11. Lee JG, Shim KS, Koh SK. Incidence of detrusor underactivity in men with prostatism older than 50 years. Korean J Urol. 1999; 40:347–352.
12. Seo YJ, Seo HK, Chung MK. The usefulness of pressure-flow study as preoperative evaluation in benign prostatic hyperplasia patients. Korean J Urol. 2003; 44:534–539.
13. Chung HY, Han DS, Jang YS, Song KH. The influences of bladder outlet obstruction on improvement of storage symptoms in patients who underwent transurethral resection of prostate. Korean J Urol. 2008; 49:912–916.
14. Yoo TK, Cho HJ. Benign prostatic hyperplasia: from bench to clinic. Korean J Urol. 2012; 53:139–148.
15. Mayer EK, Kroeze SG, Chopra S, Bottle A, Patel A. Examining the 'gold standard': a comparative critical analysis of three consecutive decades of monopolar transurethral resection of the prostate (TURP) outcomes. BJU Int. 2012; 110:1595–1601.
16. Doll HA, Black NA, McPherson K, Flood AB, Williams GB, Smith JC. Mortality, morbidity and complications following transurethral resection of the prostate for benign prostatic hypertrophy. J Urol. 1992; 147:1566–1573.
17. Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Writing Committee, the American Urological Association. Transurethral prostatectomy: immediate and postoperative complications. Cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol, 141: 243-247, 1989. J Urol. 2002; 167:5–9.
18. Djavan B, Madersbacher S, Klingler C, Marberger M. Urodynamic assessment of patients with acute urinary retention: is treatment failure after prostatectomy predictable? J Urol. 1997; 158:1829–1833.
19. Kuo HC. Clinical prostate score for diagnosis of bladder outlet obstruction by prostate measurements and uroflowmetry. Urology. 1999; 54:90–96.
20. Robertson AS, Griffiths C, Neal DE. Conventional urodynamics and ambulatory monitoring in the definition and management of bladder outflow obstruction. J Urol. 1996; 155:506–511.
21. Han DH, Jeong YS, Choo MS, Lee KS. The efficacy of transurethral resection of the prostate in the patients with weak bladder contractility index. Urology. 2008; 71:657–661.
22. van Venrooij GE, van Melick HH, Boon TA. Comparison of outcomes of transurethral prostate resection in urodynamically obstructed versus selected urodynamically unobstructed or equivocal men. Urology. 2003; 62:672–676.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download