Abstract
Purpose
To evaluate the outcome of fulguration of Hunner's ulcers (HUs) in painful bladder syndrome/interstitial cystitis (PBS/IC) that is refractory to conservative treatment.
Materials and Methods
Patients diagnosed with refractory PBS/IC and treated with fulguration between 2011 and 2013 were identified through screening of medical records. To evaluate treatment outcomes, voiding diaries, the visual analogue scale (VAS) for pain, and two IC symptom questionnaires (pelvic pain and urgency/frequency scale [PUF] and O'Leary-Sant IC symptom index and IC problem index [OS]) were used. Fulguration was deemed to be successful if the VAS score was <2 or less than half of the preoperative VAS score.
Results
In total, 27 patients with PBS/IC in whom conservative treatments had failed were enrolled. Two months after fulguration, decreases were observed in the mean 24-hour urinary frequency (from 16.0 to 10.2), 24-hour urgency episodes (8.0 to 1.8), and the VAS (5.8 to 1.2), PUF symptom (15.1 to 7.0), PUF bother (8.4 to 2.7), OS symptom (15.1 to 7.2), and OS problem (13.8 to 6.0) scores. At 5 and 10 months, all variables had worsened. At 2, 5, and 10 months, the success rates were 94.1%, 70.0%, and 33.3%, respectively. Four patients underwent one repeat fulguration on average 11.3 months after the first fulguration. Repeat fulguration was not significantly associated with any clinical characteristics.
Painful bladder syndrome/interstitial cystitis (PBS/IC) is diagnosed if a patient complains of chronic pelvic pain, pressure, or discomfort that is perceived to be related to the urinary bladder and these symptoms are accompanied by at least one other urinary symptom, such as a persistent urge to void or high urinary frequency. Other diseases that could cause the symptoms must be excluded [1]. Between 5% and 20% of patients with PBS/IC have ulcers, which were first described by Hunner. Consequently, PBS/IC is frequently subdivided into a classic ulcerative form and the so-called early [2] or nonulcerative [3,4] form. Hunner's ulcers (HUs) typically present on cystoscopy as a circumscript, reddened mucosal area with small vessels radiating toward a central scar.
Although several different nonoperative therapies are available, including bladder hydrodistention [5], intravesical instillations [6], and oral medication with sodium pentosan polysulfate [7] or amitriptyline [8], these treatments often fail or become less effective despite inducing an initial response. For several decades, HU-related symptoms have been treated by endourologic ablation of this bladder pathology. Indeed, the 2011 American Urological Association guidelines state that if HUs are present, then fulguration with a laser or electrocautery or injection of triamcinolone should be performed [9].
The reported success rates of fulguration for HUs vary from 66% to 90% [10-12]. However, because of the diversity of symptoms, it is difficult to objectively assess therapeutic outcomes. Moreover, although significant numbers of patients require repeat treatment owing to ulcer recurrence, the distribution and numbers of recurring ulcers have not yet been described.
The present study investigated the efficacy of fulguration of HUs in PBS/IC. To determine treatment efficacy, patient symptoms were recorded and a voiding diary and the visual analogue scale (VAS) were used along with two published IC symptom questionnaires: the O'Leary-Sant IC symptom index and the IC problem index [13] and the pelvic pain and urgency/frequency (PUF) scale [14]. The questionnaire scores before and after HU fulguration were then compared.
The medical records of Asan Medical Center, which is a tertiary referral center, were screened for patients who had been diagnosed with PBS/IC with HUs by cystoscopy, whose treatments with amitriptyline or pentosan polysulfate for more than 3 months or other remedies such as hydro distension or bladder instillation of hyaluronic acid or chondroitin sulphate were ineffective, and who were then treated with fulguration by a single surgeon (M.S.C.) between September 2011 and December 2012. All patients who met these criteria were enrolled in the study. To diagnosis PBS/IC, the definition of the European Society for the Study of Interstitial Cystitis was used [1]. If cystoscopy revealed the presence of abnormal mucosal lesions as well as HUs, cold cup biopsy was performed to rule out malignancy. However, in all biopsied patients, the pathological reports demonstrated transmural inflammation.
All patients underwent the standard hospital procedure, as follows. Before the operation, comorbidities (diabetes mellitus, hypertension, or history of tuberculosis), body mass index, duration of symptoms, and previous treatment for PBS/IC (including medications, bladder instillation, and hydrodistention) were recorded. Voiding function was evaluated by uroflowmetry and residual urine.
During the operation, cystoscopy was performed with the patient under general anesthesia. The bladder was fully inspected at a low filling volume for abnormal lesions, including HUs and scars. After a biopsy was taken in the area in question, deep and full fulguration of the ulcerative tissue was performed. A ball-shaped coagulating electrode set to a current of 40 V was used to point-cauterize the HU base. The fulguration was performed at a low bladder filling volume and an effort was made to not fulgurate the normal mucosa beyond the region of the initially identified HU. Rather than brief surface fulguration, the cautery current was applied at the HU base to transmit it to deeper tissue layers. Bleeding from the biopsy sites and ulcers was electrically coagulated. The Foley catheter was maintained for a day.
After the fulguration, the patients visited Asan Medical Center 2, 5, and 10 months after surgery. To determine the treatment outcomes, the voiding diary was assessed and the VAS score, PUF symptom score, PUF bother score, O'Leary-Sant IC symptom index, and IC problem index scores before and 2, 5, and 10 months after fulguration for HUs were assessed. At each postoperative visit, fulguration was considered to be successful if the VAS score was <2 or less than half of the preoperative VAS score.
Patients who did not meet the criteria for success after fulguration at a postoperative visit were treated with oral medications or application of intravesical medication. Patients in whom the symptoms were refractory to the medications underwent cystoscopic examination. If HUs were detected during cystoscopy, a secondary fulguration of the HUs was performed. The clinical characteristics of the patients who underwent fulguration twice and the patterns of HU recurrence were assessed.
Patient characteristics are reported as mean standard deviation (SD) unless otherwise indicated. IBM SPSS ver. 18.0 (IBM Co., Armonk, NY, USA) was used for statistical analysis. A p-value <0.05 was deemed to indicate statistical significance.
In total, 27 females with a mean (SD) age of 63 (8.3) years were included in this study. The mean symptomatic period before fulguration was 55.9 months. Before fulguration, all patients had been treated with medications such as amitriptyline or pentosan polysulfate for more than 3 months (Table 1): eight patients (29.6%) underwent on average 6.1 intravesical medication applications and 12 (44.4%) underwent one to three sessions of hydrodistention. Before fulguration, the mean peak micturition flow and residual urine after micturition at uroflowmetry were 16.7 (6.5) mL/s and 20.7 (31.6) mL, respectively. Analysis of the micturition diaries revealed a mean 24-hour urinary frequency of 16.0 (5.0) and 8.0 (6.4) urgency episodes. The mean VAS score was 5.8 (1.9); the PUF symptom and bother scores were 15.1 (3.1) and 8.4 (2.5), respectively; and the IC symptom and problem index scores were 15.1 (3.8) and 13.8 (3.3), respectively.
On the first fulguration, the patients had on average 2.9 (range, 1 to 5) HU lesions. The overall mean follow-up period was 171 days. There were no intraoperative complications and one postoperative complication. One patient visited the emergency room 1 week after fulguration because of hematuria; however, it was spontaneously resolved within a few hours.
Of the 27 study patients, 4 (14.8%) underwent one repeat fulguration session, resulting in a total of 31 fulguration procedures. The mean interval between the first and repeat fulgurations was 11.3±2.9 months. A review of the clinical characteristics of the patients who underwent repeat fulguration failed to detect marked differences between these patients and the patients who underwent only one fulguration (Table 2). At the repeat fulguration, the location of most HUs was different from the location of the HUs at the first fulguration except for two patients. In total, 19 patients visited the hospital 2 months after the fulguration. As shown in Fig. 1, their 24-hour urinary frequency and urgency episodes were then 10.2 (2.8) and 1.8 (3.3), respectively; their VAS score was 1.2 (1.3); their PUF symptom and bother scores were 7.0 (3.7) and 2.7 (1.6), respectively; and their IC symptom index score and problem index scores were 7.2 (6.5) and 6.0 (4.2), respectively. All scores had significantly improved relative to the preoperative data.
In total, 13 patients visited the hospital 5 months after the fulguration. All scores were slightly increased relative to the 2-month data: the 24-hour urinary frequency and urgency episodes were 15.4 (6.2) and 5.2 (6.2), respectively; the VAS score was 2.8 (2.7); the PUF symptom and bother scores were 11.8 (4.7) and 5.5 (3.3), respectively; and the IC symptom index score and problem index score were 11.4 (6.6) and 9.9 (5.0), respectively (Fig. 1).
In total, 10 patients visited the hospital 10 months after the fulguration. The scores were slightly higher than the 5-month scores. The 24-hour urination frequency and urgency episodes were 14.7 (6.4) and 6.5 (8.6), respectively, whereas the VAS score was 3.5 (2.2); the PUF symptom and bother scores were 11.6 (4.4) and 6.1 (2.1), respectively; and the IC symptom index and problem index scores were 13.1 (5.7) and 10.4 (4.4), respectively (Fig. 1). Of the 31 fulgurations, the success rates at 2, 5, and 10 months after treatment were 94.1%, 70.0%, and 33.3%, respectively. Ten patients who did not meet the criteria for success were treated with intravesical instillation.
Patients with PBS/IC and HU usually have severe symptoms and it is a challenge for the urologist to treat them effectively. There is no gold standard treatment method for this disease, and the regimen is usually trial-and-error in nature. Patients with PBS/IC are often offered an array of nonsurgical treatments, such as intravesical instillation, oral medication, and transcutaneous electrical nerve stimulation. However, the effectiveness of these treatments is usually of limited duration and relapse is common. In the present series, all patients had undergone multiple medical treatments with no significant response. However, fulguration for HU rapidly led to a satisfactory improvement in symptoms, as shown by the objective improvements in the IC symptom questionnaire as well as the pain and voiding symptoms.
Endourological ablation of bladder tissue aims to eliminate visible lesions, in particular HUs. In the study of Fall [11], complete transurethral resection (TUR) of all visible lesions in 30 patients with HU resulted in the initial disappearance of pain in all patients and a decrease in urinary frequency in 21 patients. The same center recently reported the largest series to date of patients with HU treated with complete TUR [12]. They found that it ameliorated the pain symptoms in 40% of the patients. Fall [11] suggested that TUR may alleviate pain in patients with PBS/IC because it removes the intramural nerve endings that are affected by inflammation. However, TUR is associated with a risk of bladder perforation because the resection is being performed in areas that have already been thinned by ulceration.
Another modality, laser fulguration, was reported to be a more easily performed alternative endoscopic treatment to TUR for PBS/IC. Malloy and Shanberg [15] performed neodymium:yttrium-aluminium-garnet (Nd:YAG) laser ablation in 27 patients with PBS/IC by delivering 20 to 25 Watts to the HU and the immediately adjacent mucosa. Although the symptoms of 21 patients (78%) improved immediately after laser treatment, 12 of these 21 (57%) developed recurrent symptoms within an 18-month period. Recently, Rofeim et al. [16] removed the HUs of 24 patients with refractory classic PBS/IC by ablative Nd:YAG laser and found that all patients had symptom improvement within days without complications. However, 11 patients (46%) required one to four additional treatments.
Another approach is electrocautery. Hillelsohn et al. [17] reported the long-term clinical outcomes of 59 patients with HUs who were treated by electrocautery by using the Bugbee electrode. Of the 32 patients who underwent a single fulguration, 25 (78%) reported improved or stable symptoms. However, 27 of the 59 patients (45.8%) required repeat fulguration at a median follow-up period of 44.8 months.
The American Urological Association 2011 guideline panel assigned the evidence grade C recommendation for fulguration with laser, electrocautery, and/or injection of triamcinolone [9]. This guideline recommended that fulguration should be performed if HUs are present on cystoscopic examination. The European Association of Urology 2010 guideline on chronic pelvic pain also recommended TUR or laser ablation for HUs after a diagnosis of classic PBS/IC by cystoscopy [18]. In patients who have inadequate response to this treatment, noninvasive therapies can be followed.
In the present series, 94.1% of the patients who underwent initial HU fulguration using a ball-shaped coagulating electrode showed rapid symptomatic improvement at 2 months. The mean scores of two validated questionnaires, the PUF symptom scale and O'Leary-Sant IC index, which have not been used in previous studies of HU fulguration, also showed symptom improvement. Although the mechanism by which this method improved the symptoms is not clear, it could be the result of the destruction of afferent neurons, inflammatory cell lysis, or the fact that fulguration causes a sudden release of inflammatory mediators that leads to a deficit later. However, at the 5- and 10-month follow-up visits in the present study, the symptoms and the questionnaire scores were worse than at 2 months. This indicates that this procedure does not cure the underlying disease; rather, it works by just symptomatic treatment. Supporting this is that 4 of the 27 patients (14.8%) had recurrent HUs and underwent a repeat fulguration.
These four patients underwent their repeat fulguration on average 11.3 months after the initial procedure. This retreatment rate is lower than the rates reported by other fulguration studies [16,17]. This may be because 1) the follow-up period of our study was shorter than those of the previous studies, and 2) when symptoms recurred after the first fulguration, we treated them with intravesical instillation; repeat fulguration was applied only if the patient still did not show symptom improvement. None of the clinical characteristics of the four repeat fulguration patients were significantly associated with the need for repeat fulguration.
In the present study, fulguration was performed by using a low bladder filling volume (up to 200 mL) because a high filling volume can lead to cracking and bleeding from ulcer sites and increase the risk of bowel injury, especially during fulguration of HUs at the bladder dome. In addition, because fulguration of the HU alone and the HU plus the surrounding tissue yields identical symptom improvement [16], an effort was made during surgery in the present study to fulgurate only the initially identified HUs and to not remove normal mucosa as well.
This study is based on a consistently treated patient population. The symptoms of the patients were well documented owing to the use of two published questionnaires and all patients were operated on by the same surgeon using the same technique. The observed improvements were statistically significant at 2 months postoperatively, which suggests that the treatment was clinically helpful. We believe that this study objectively determined the effects of fulguration for HUs in patients with PBS/IC.
The limitations of the study included that it was a retrospective study; namely, the patient population was identified after the data were collected. It should be noted, however, that all patients were treated and followed up according to the protocol of our department. In addition, there was no control group. Furthermore, the sample size was small and the follow-up period was relatively short. However, the study was still adequately powered to obtain significance in the primary outcome of the study.
It remains unclear whether the HUs in repeat fulgurations are true recurrences (i.e., located at the previously fulgurated site), recurrences in a remote site, or HUs that were not identified during the previous fulguration. To address this, narrow band imaging cystoscopy will be used to map the location of HUs in PBS/IC in a future study. Narrow band imaging cystoscopy will be used because it seems to be more sensitive than conventional cystoscopy in terms of finding HUs.
The present study showed that the elimination of HUs in PBS/IC by fulguration is effective in patients whose symptoms are refractory to medication or other conservative treatments. Although it is not curative, fulguration provides patients an opportunity to experience decreased symptoms for an extended period. The locations of most HUs at the repeat fulguration differed from those at the first fulguration.
Figures and Tables
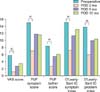 | FIG. 1Change in symptoms after fulguration for Hunner's ulcers in patients with PBS/IC. PBS/IC, painful bladder syndrome/interstitial cystitis; POD, postoperative day; VAS, visual analogue scale; PUF, pelvic pain and urgency/frequency scale; IC, interstitial cystitis. a)p<0.05, otherwise, p>0.05. |
TABLE 1
Demographic and clinical characteristics of the 27 patients who underwent fulguration for Hunner's ulcers

References
1. van de Merwe KP, Nordling J, Bouchelouche P, Bouchelouche K, Cervigni M, Daha LK, et al. Diagnostic criteria, classification, and nomenclature for painful bladder syndrome/interstitial cystitis: an ESSIC proposal. Eur Urol. 2008; 53:60–67.
2. Messing EM, Stamey TA. Interstitial cystitis: early diagnosis, pathology, and treatment. Urology. 1978; 12:381–392.
3. Fall M, Johansson SL, Aldenborg F. Chronic interstitial cystitis: a heterogeneous syndrome. J Urol. 1987; 137:35–38.
4. Koziol JA, Adams HP, Frutos A. Discrimination between the ulcerous and the nonulcerous forms of interstitial cystitis by noninvasive findings. J Urol. 1996; 155:87–90.
5. Glemain P, Riviere C, Lenormand L, Karam G, Bouchot O, Buzelin JM. Prolonged hydrodistention of the bladder for symptomatic treatment of interstitial cystitis: efficacy at 6 months and 1 year. Eur Urol. 2002; 41:79–84.
6. Sant GR, LaRock DR. Standard intravesical therapies for interstitial cystitis. Urol Clin North Am. 1994; 21:73–83.
7. Fritjofsson A, Fall M, Juhlin R, Persson BE, Ruutu M. Treatment of ulcer and nonulcer interstitial cystitis with sodium pentosanpolysulfate: a multicenter trial. J Urol. 1987; 138:508–512.
8. van Ophoven A, Pokupic S, Heinecke A, Hertle L. A prospective, randomized, placebo controlled, double-blind study of amitriptyline for the treatment of interstitial cystitis. J Urol. 2004; 172:533–536.
9. Hanno PM, Burks DA, Clemens JQ, Dmochowski RR, Erickson D, Fitzgerald MP, et al. AUA guideline for the diagnosis and treatment of interstitial cystitis/bladder pain syndrome. J Urol. 2011; 185:2162–2170.
10. Greenberg E, Barnes R, Stewart S, Furnish T. Transurethral resection of Hunner's ulcer. J Urol. 1974; 111:764–766.
11. Fall M. Conservative management of chronic interstitial cystitis: transcutaneous electrical nerve stimulation and transurethral resection. J Urol. 1985; 133:774–778.
12. Peeker R, Aldenborg F, Fall M. Complete transurethral resection of ulcers in classic interstitial cystitis. Int Urogynecol J Pelvic Floor Dysfunct. 2000; 11:290–295.
13. O'Leary MP, Sant GR, Fowler FJ Jr, Whitmore KE, Spolarich-Kroll J. The interstitial cystitis symptom index and problem index. Urology. 1997; 49:5A Suppl. 58–63.
14. Parsons CL, Dell J, Stanford EJ, Bullen M, Kahn BS, Waxell T, et al. Increased prevalence of interstitial cystitis: previously unrecognized urologic and gynecologic cases identified using a new symptom questionnaire and intravesical potassium sensitivity. Urology. 2002; 60:573–578.
15. Malloy TR, Shanberg AM. Laser therapy for interstitial cystitis. Urol Clin North Am. 1994; 21:141–144.
16. Rofeim O, Hom D, Freid RM, Moldwin RM. Use of the neodymium: YAG laser for interstitial cystitis: a prospective study. J Urol. 2001; 166:134–136.
17. Hillelsohn JH, Rais-Bahrami S, Friedlander JI, Okhunov Z, Kashan M, Rosen L, et al. Fulguration for Hunner ulcers: long-term clinical outcomes. J Urol. 2012; 188:2238–2241.
18. Fall M, Baranowski AP, Elneil S, Engeler D, Hughes J, Messelink EJ, et al. EAU guidelines on chronic pelvic pain. Eur Urol. 2010; 57:35–48.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download