Abstract
Purpose
We investigated the impact on prostate-specific antigen (PSA) and prostate volume (PV) of statin medication for 1 year in patients with benign prostatic hyperplasia (BPH).
Materials and Methods
We retrospectively investigated 791 patients in whom BPH was diagnosed. For analysis, the patients were divided into four groups according to their medications: group A, α-blocker; group B, α-blocker+statin; group C, α-blocker+dutasteride; group D, α-blockers+statin+dutasteride. To investigate changes in serum PSA, PV, and total cholesterol, we analyzed the data at the time of initial treatment and after 1 year of medication.
Results
After 1 year, group A showed a 1.3% increase in PSA and a 1.0% increase in PV. Group B showed a 4.3% decrease in PSA and a 1.8% decrease in PV. The difference in PV reduction between groups A and B was statistically significant (p<0.001). Group C showed a 49.1% reduction in PSA and a 22.9% reduction in PV. Group D showed a 51.6% reduction in PSA and a 24.5% reduction in PV. The difference in PV reduction between groups C and D was not statistically significant (p=0.762). By use of a multivariate logistic regression model, we found that the probability of PV reduction after 1 year was more than 14.8 times in statin users than in statin nonusers (95% confidence interval, 5.8% to 37.6%; p<0.001).
Benign prostatic hyperplasia (BPH) is a progressive disease that occurs with lower urinary tract symptoms (LUTS). Approximately 25% of all men experience BPH, and the prevalence of histopathologic BPH is age dependent, with initial development usually after 40 years of age. The prevalence of BPH is about 50% by 60 years of age and is as high as 90% by age 85 [1]. Symptomatic bladder outlet obstruction typically requires medication, such as with an α-blocker and 5-α reductase inhibitor (5ARI).
The 5ARIs decrease prostate-specific antigen (PSA) and prostate volume (PV) through inhibition of the nuclear-bound steroid 5-alpha reductase (5AR), which chemically reduces testosterone to dihydrotestosterone (DHT), the principal androgen stimulating prostatic growth.
Dutasteride is the first selective dual inhibitor of both type 1 and type 2 5AR, whereas finasteride is a selective mono-inhibitor of type 2 5AR. Dual inhibition of 5ARIs with dutasteride results in near-complete and consistent suppression of serum DHT. The treatment reduces serum PSA levels by approximately 50% in 6 months and total prostatic volume by 25% in 2 years [2-4].
3-Hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase plays the rate-limiting step in cholesterol biosynthesis, and inhibition of this enzyme decreases cholesterol synthesis. By inhibiting cholesterol biosynthesis, statins lead to increased hepatic low-density lipoprotein (LDL) receptor activity and accelerated clearance of circulating LDL, resulting in a dose-dependent reduction of LDL-cholesterol (LDL-C) in plasma. Statins also reduce plasma triglycerides. Statins also have a mild high-density lipoprotein.raising effect (5.10%). In this way, statins can reduce cardiovascular morbidity associated with dyslipidemia and vascular disease [5-8].
Statins also reduce isoprenylation of the G-proteins Rho and Ras, which could lead to prostatic smooth muscle relaxation [9], increased apoptosis/reduced proliferation of prostatic epithelium and stroma [10], reduced bladder and prostatic fibrosis through modulation of expression of connective tissue growth factor [11], and enhanced blood flow to the lower urinary tract. These actions could lead to beneficial effects on BPH. In addition, the growth-inhibitory effect on prostatic epithelium may be related in the prevention or treatment of prostate cancer [12]. Reduction of serum cholesterol may also be related in the treatment of BPH, because a high-cholesterol diet leads to histologic changes in the rat prostate that are similar to those in prostatic hyperplasia [13].
In the present study, we investigated the changes in serum PSA, PV, and total cholesterol after 1 year in BPH patients taking statins to determine whether statins really decrease PSA and PV.
BPH patients who had a follow-up in Kangbuk Samsung Medical Center from January 2008 to December 2011 were included, and the results after medication for 1 year were compared retrospectively. Patients with abnormal PSA levels in whom BPH was diagnosed by prostate biopsy were included.
The exclusion criteria were a history of taking a 5ARI in another hospital before the start of the study, treatment for hyperlipidemia, persistent local lower urinary tract pathology (e.g., bladder stone, urethral stricture, prostatitis, recurrent gross hematuria, transitional cell carcinoma, bladder-neck contracture, large bladder diverticulum), unexplained microscopic hematuria, neurogenic bladder, urinary tract infection, prostate cancer, cystoscopy or catheterization within 1 month before PSA evaluation, and patients who underwent transurethral resection of the prostate.
We investigated 791 patients who were diagnosed with BPH, and the patient population was divided into four groups according to medication: group A, α-blocker; group B, α-blocker+statin; group C, α-blocker+dutasteride; group D, α-blockers+statin+dutasteride. The type of α-blocker used was tamsulosin, 0.2 mg, terazosin, 2 mg, and alfuzosin, 10 mg, and the type of statin used was atorvastatin, 10 mg, fluvastatin, 80 mg, and simvastatin, 20 mg. Statins were used in the case of hyperlipidemia (total serum cholesterol exceeding 240 mg/dL or triglyceride greater than 200 mg/dL). Dutasteride was used for an enlarged prostatic volume (more than 35 g), if the patient had experienced acute urinary retention, or if the patient showed no improvement of urinary symptoms with treatment with an α-blocker alone.
PSA, PV, and total cholesterol were measured before medication in all patients receiving a combination of α-blocker, statin, and dutasteride. Prostate size was measured with a biplanar transrectal ultrasonography (TRUS) probe and PV was calculated by using the formula for a prostate ellipse (width×length×height×0.52). Enzyme immunoassay was used for the measurement of PSA (Cisbio Bioassays, Codolet, France). One year later, the results of PSA, PV, and total cholesterol were also investigated.
Data were expressed as mean±standard deviation for continuous variables and as percentages of the number for categorical variables. According to the duration of treatment, the paired t-test was applied to PSA, PV, and total cholesterol changes in each group. Also, the differences in reduction of PSA, PV, and total cholesterol between each group were analyzed by use of the independent t-tests for continuous variables and Pearson chi-square tests for categorical variables. Also, of the variables, PSA and PV were log-transformed and were analyzed by use of independent t-tests.
Statistically significant differences between groups were compared with one-way analysis of variance (Table 1). Multivariable analysis using logistic regression was performed with adjustment for the following variables: age, hypertension (HTN), diabetes mellitus (DM), coronary heart disease (CHD), total cholesterol, and body mass index (BMI).
Statistical analysis was performed by using IBM SPSS ver. 21.0 (IBM Co., Armonk, NY, USA). Statistical significance was defined as a p-value of <0.05.
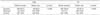
Baseline characteristics and 1-year follow-up results in each group are shown in Table 1 and Fig. 1.
After 1 year, PSA in group A was increased by 1.3% from 2.36 to 2.39 ng/mL (paired t-test, p<0.001), and PSA in group B was decreased by 4.3% from 2.33 to 2.23 ng/mL (p<0.001). PSA in group C was decreased by 49.1% from 3.34 to 1.87 ng/mL (p<0.001), and PSA in group D was decreased by 51.6% from 3.43 to 1.66 ng/mL (p<0.001). In addition, the difference in PSA reduction between groups A and B was significant by chi-square test (p<0.001) and independent t-test (p<0.001). However, the difference in PSA reduction between groups C and D was not statistically significant by chi-square test (p=0.682) or independent t-test (p=0.696).
After 1 year, PV in group A was increased by 1.0% from 35.28 to 35.63 cm3 (paired t-test, p=0.001). On the other hand, PV in group B was reduced by 1.8% from 35.25 to 34.60 cm3 (p<0.001). In addition, the difference in PV reduction between groups A and B was significant by chi-square test (p<0.001) and independent t-test (p<0.001). Also, PV in group C was decreased by 22.9% from 43.73 to 33.71 cm3 (p<0.001), and PV in group D was decreased by 24.5% from 43.53 to 32.85 cm3 (p<0.001). The difference in PV reduction between groups C and D was not significant by chi-square test (p=0.762) or independent t-test (p=0.776).
After 1 year, total cholesterol in group A was increased by 0.6% from 193.24 to 194.32 mg/dL (paired t-test, p=0.471), and total cholesterol in group B was decreased by 25.6% from 229.86 to 171.15 mg/dL (p<0.001). The difference in total cholesterol reduction between groups A and B was significant by chi-square test (p<0.001) and independent t-test (p<0.001). Total cholesterol in group C was increased by 0.1% from 193.89 to 194.14 mg/dL (paired t-test, p=0.354). Total cholesterol in group D was decreased by 25.8% from 229.55 to 170.43 mg/dL (p<0.001). The difference in total cholesterol reduction between group C and group D was significant by chi-square test (p<0.001) and independent t-test (p<0.001). The use of statins in groups B and D reduced the level of cholesterol after 1 year. However, the difference in total cholesterol reduction between groups B and D was not significant by chi-square test (p=0.792) or independent t-test (p=0.784).
Also, excluding dutasteride users, because dutasteride could affect the PSA and PV, we split the patients in two groups, statin users and nonusers, and analyzed the correlation between variables and statin (Table 2). We also investigated the increase or decrease in PSA and PV within each group after 1 year (Table 3).
Statin users had a 21.6-fold (95% confidence interval [CI], 12.8% to 36.3%; p<0.001) higher probability of PSA reduction after 1 year than did nonusers, and the odds ratio adjusted for age, HTN, DM, CHD, total cholesterol, and BMI was 12.4 (95% CI, 5.1% to 33.2%; p<0.001) (Table 4). Also, statin users had a 25.7-fold (95% CI, 15.0% to 43.9%; p<0.001) higher probability of PV reduction after 1 year than did nonusers and the odds ratio adjusted for age, HTN, DM, CHD, total cholesterol, and BMI was 14.8 (95% CI, 5.8% to 37.6%; p<0.001) (Table 5).
We performed logistic regression analysis by regarding a reduction in PV of over 1% after 1 year as a valid result, in light of error in TRUS. As a result, the crude odds ratio was 25.7 and the adjusted odds ratio was 14.5. Moreover, we did logistic regression analysis by regarding a reduction in PV of over 2% after 1 year as a valid result. As a result, the crude odds ratio was 30.6 and the adjusted odds ratio was 10.6. Thus, statin users, despite physician error, really had a high probability of prostatic volume reduction.
Statins (HMG-CoA reductase inhibitors) reduce cholesterol biosynthesis. By inhibiting cholesterol biosynthesis, statins lead to increased hepatic LDL receptor activity and accelerated clearance of circulating LDL, resulting in a dose-dependent reduction of LDL-C in plasma. Except for rosuvastatin, differences in the effects of statins on LDL-C reduction have been reported among statins with similar baseline characteristics in most studies.
Atorvastatin, 10 mg, fluvastatin, 80 mg, lovastatin, 40-80 mg, and simvastatin, 20 mg can reduce LDL-C by 30-40%; fluvastatin, 40 mg, lovastatin, 10.20 mg, and simvastatin, 10 mg can decrease LDL-C by 20-30% [14]. In the current study, atorvastatin, 10 mg, fluvastatin, 80 mg, and simvastatin, 20 mg were considered to have similar baseline characteristics.
In Muller et al. [15]'s study, in BPH patients taking a statin medication, the PSA level decreased by 4.1% within 1 year and PV was reduced by 4% within 2 years. The PSA decline after statin initiation was positively associated with LDL-C decline in a near linear fashion. After adjustment for multiple factors, for every 10% decline in LDL-C after statin initiation, PSA declined by 1.64% [16,17].
In the current study, PSA in group B taking a statin and an α-blocker medication was reduced by 4.3% and PV was reduced by 1.8% after 1 year. The result of the change in the PSA level in statin users was statistically valid compared with statin nonusers (+1.3% vs. -4.3%, respectively, p<0.001).
We found that the PSA decline after taking statins was significantly associated with the decline in total cholesterol. Prostate growth and cancer development have been related to abnormal cholesterol metabolism. For example, it has been noted that increased cholesterol content in prostate tissue is correlated with the presence of malignancy [18,19]. Furthermore, reducing cholesterol bioavailability has been found to alter the composition of membrane-signaling domains and to induce apoptosis in prostate cells. Replete cholesterol content reverses the apoptotic effects, suggesting that cholesterol reduction by statins may influence prostate biology [20,21]. It is conceivable that by influencing cholesterol metabolism, statins may lower the levels of intraprostatic androgens, which could reduce PSA levels.
In vitro, evidence suggests that statins influence prostate biology. Statins might play a role by inhibiting inflammation [22], cell proliferation [23], migration/adhesion [24], and angiogenesis [25]; promoting apoptosis [10], and invasion [24]; and affecting intracellular survival signals such as Rho and Ras [9].
A recent laboratory study by Parikh et al. [26] demonstrated that statins induced autophagy and cell death in prostate cancer cells, likely through inhibition of geranylgeranylation, which might explain the protective effects of statins on prostate cancer progression. Also, statin medication was associated with a decreased risk of prostate cancer, less frequent high-grade prostate cancer, and a lower volume of prostate cancer, which suggests that statin medication has a protective effect against prostate cancer [27].
Also, statin medication was associated with a decreased risk of developing moderate/severe LUTS and decreased risks of maximum flow rate and BPH [28]. Several studies have suggested that men with elevated LDL-C levels or other metabolic risk factors (such as HTN, diabetes, and obesity) had an increased odds of having BPH or LUTS. It was possible that these conditions could have confounded or modified associations between statin medication and the outcomes. In the current study, after adjustment for HTN, diabetes, CHD, total cholesterol, and BMI, the difference in PV reduction between these comorbidities (such as HTN, DM, hyperlipidemia, CHD, obesity) and statin medication was not statistically significant.
In a study on PV changes using dutasteride, dutasteride resulted in PV reduction of 19.9% in 6 months, 23.6% in 1 year, 26% in 2 years, and 27.3% in 4 years [29]. In the current study of dutasteride therapy for 1 year, PV was reduced by 22.9%, which was similar to previous results. When a statin and dutasteride were administered during the first 1 year, PSA and PV were significantly decreased. Also, the PSA and PV reduction in groups C and D were greater than in groups A and B, which might have been due to the effect of dutasteride. However, the rates of reduction in PV were not significantly different between groups C and D. This suggests that a low DHT concentration could be a counter effect against statins. Thus, this might be the effect of dutasteride, which offsets statin function by decreasing the DHT level.
The current study had several limitations. First, the effects of α-blockers were considered to be the same. Second, this research was not subdivided into categories for statin, because the statin group was not subdivided.
Despite these limitations, we believe that our investigation showed an association among statin use, PSA levels, and PV.
Serum PSA, PV, and total cholesterol were decreased in BPH patients taking statin medication for 1 year compared with the group taking α-blocker alone. Also, the effect of 5ARI on the reduction of PSA and PV was not affected by adding a statin.
Statin administration reduced PSA and PV in BPH patients. This infers that statin medication could improve LUTS in addition to preventing cardiovascular disease, which might play a role in the chemoprevention of prostate cancer.
Figures and Tables
FIG. 1
Mean percentage change from baseline in PSA (A), PV (B), and total cholesterol (C) after treatment for 1 year. Error bars indicate standard deviation. PSA, prostate-specific antigen; PV, prostate volume.

TABLE 1
Baseline characteristics of the patients and results of the analysis of variance

Values are presented as mean±standard deviation or number (%). A p-value is for one-way analysis of variance.
PSA, prostate-specific antigen; PV, prostate volume; BMI, body mass index.
a-c:Different symbols for each variable indicate statistical significance (p<0.05) based on Tukey multiple comparisons.
References
1. AUA Practice Guidelines Committee. AUA guideline on management of benign prostatic hyperplasia (2003). Chapter 1: Diagnosis and treatment recommendations. J Urol. 2003; 170(2 Pt 1):530–547.
2. Bruchovsky N, Rennie PS, Batzold FH, Goldenberg SL, Fletcher T, McLoughlin MG. Kinetic parameters of 5 alpha-reductase activity in stroma and epithelium of normal, hyperplastic, and carcinomatous human prostates. J Clin Endocrinol Metab. 1988; 67:806–816.
3. Marihart S, Harik M, Djavan B. Dutasteride: a review of current data on a novel dual inhibitor of 5alpha reductase. Rev Urol. 2005; 7:203–210.
4. Choi YH, Cho SY, Cho IR. The different reduction rate of prostate-specific antigen in dutasteride and finasteride. Korean J Urol. 2010; 51:704–708.
5. Cannon CP, Braunwald E, McCabe CH, Rader DJ, Rouleau JL, Belder R, et al. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004; 350:1495–1504.
6. Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005; 366:1267–1278.
7. Ray KK, Cannon CP. Atorvastatin and cardiovascular protection: a review and comparison of recent clinical trials. Expert Opin Pharmacother. 2005; 6:915–927.
8. Ndrepepa G, Fusaro M, King L, Cassese S, Tada T, Schomig A, et al. Statin pretreatment and presentation patterns in patients with coronary artery disease. Cardiol J. 2013; 20:52–58.
9. Rees RW, Foxwell NA, Ralph DJ, Kell PD, Moncada S, Cellek S. Y-27632, a Rho-kinase inhibitor, inhibits proliferation and adrenergic contraction of prostatic smooth muscle cells. J Urol. 2003; 170(6 Pt 1):2517–2522.
10. Watts KL, Spiteri MA. Connective tissue growth factor expression and induction by transforming growth factor-beta is abrogated by simvastatin via a Rho signaling mechanism. Am J Physiol Lung Cell Mol Physiol. 2004; 287:L1323–L1332.
11. Padayatty SJ, Marcelli M, Shao TC, Cunningham GR. Lovastatin-induced apoptosis in prostate stromal cells. J Clin Endocrinol Metab. 1997; 82:1434–1439.
12. Sivaprasad U, Abbas T, Dutta A. Differential efficacy of 3-hydroxy-3-methylglutaryl CoA reductase inhibitors on the cell cycle of prostate cancer cells. Mol Cancer Ther. 2006; 5:2310–2316.
13. Ploumidou K, Kyroudi-Voulgari A, Perea D, Anastasiou I, Mitropoulos D. Effect of a hypercholesterolemic diet on serum lipid profile, plasma sex steroid levels, and prostate structure in rats. Urology. 2010; 76:1517e.1–1517e.5.
14. Weng TC, Yang YH, Lin SJ, Tai SH. A systematic review and meta-analysis on the therapeutic equivalence of statins. J Clin Pharm Ther. 2010; 35:139–151.
15. Muller R, Gerber L, Moreira D, Andriole G, Parsons JK, Fleshner N, et al. 1249 Statins slow prostate growth: Results from the reduction by dutasteride of cancer events (REDUCE) trial [abstract]. J Urol. 2012; 187:4 Suppl. e505. Abstract no. 1249.
16. Hamilton RJ, Goldberg KC, Platz EA, Freedland SJ. The influence of statin medications on prostate-specific antigen levels. J Natl Cancer Inst. 2008; 100:1511–1518.
17. Kim BS, Yoon YE, Lee SB, Park SY, Son YW, Kim YT, et al. The change of prostate-specific antigen and prostate-specific antigen density in patients with benign prostatic hyperplasia after dutasteride treatment. Korean J Urol. 2008; 49:893–898.
18. Schaffner CP. Prostatic cholesterol metabolism: regulation and alteration. Prog Clin Biol Res. 1981; 75A:279–324.
19. Hager MH, Solomon KR, Freeman MR. The role of cholesterol in prostate cancer. Curr Opin Clin Nutr Metab Care. 2006; 9:379–385.
20. Zhuang L, Kim J, Adam RM, Solomon KR, Freeman MR. Cholesterol targeting alters lipid raft composition and cell survival in prostate cancer cells and xenografts. J Clin Invest. 2005; 115:959–968.
21. Pelton K, Freeman MR, Solomon KR. Cholesterol and prostate cancer. Curr Opin Pharmacol. 2012; 12:751–759.
22. Biasucci LM, Biasillo G, Stefanelli A. Inflammatory markers, cholesterol and statins: pathophysiological role and clinical importance. Clin Chem Lab Med. 2010; 48:1685–1691.
23. Weis M, Heeschen C, Glassford AJ, Cooke JP. Statins have biphasic effects on angiogenesis. Circulation. 2002; 105:739–745.
24. Kusama T, Mukai M, Iwasaki T, Tatsuta M, Matsumoto Y, Akedo H, et al. Inhibition of epidermal growth factor-induced RhoA translocation and invasion of human pancreatic cancer cells by 3-hydroxy-3-methylglutaryl-coenzyme a reductase inhibitors. Cancer Res. 2001; 61:4885–4891.
25. Rao S, Porter DC, Chen X, Herliczek T, Lowe M, Keyomarsi K. Lovastatin-mediated G1 arrest is through inhibition of the proteasome, independent of hydroxymethyl glutaryl-CoA reductase. Proc Natl Acad Sci U S A. 1999; 96:7797–7802.
26. Parikh A, Childress C, Deitrick K, Lin Q, Rukstalis D, Yang W. Statin-induced autophagy by inhibition of geranylgeranyl biosynthesis in prostate cancer PC3 cells. Prostate. 2010; 70:971–981.
27. Tan N, Klein EA, Li J, Moussa AS, Jones JS. Statin use and risk of prostate cancer in a population of men who underwent biopsy. J Urol. 2011; 186:86–90.
28. Guess HA, Gormley GJ, Stoner E, Oesterling JE. The effect of finasteride on prostate specific antigen: review of available data. J Urol. 1996; 155:3–9.
29. Debruyne F, Barkin J, van Erps P, Reis M, Tammela TL, Roehrborn C, et al. Efficacy and safety of long-term treatment with the dual 5 alpha-reductase inhibitor dutasteride in men with symptomatic benign prostatic hyperplasia. Eur Urol. 2004; 46:488–494.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download