Abstract
The fate of testicular salvage in spermatic cord torsion depends on the duration of ischemia and the degree of torsion. Even though spermatic cord torsion (SCT) can occur at any age, it is rarely reported in older patients. If the physician does not pay close attention to this unusual situation, the lack of suspicion for SCT may result in a missed or delayed diagnosis. We report a very uncommon case of missed SCT occurring in a 63-year-old man.
Spermatic cord torsion (SCT) is one of the true urological emergencies that mainly develop during puberty and the early adolescent period, with a calculated annual incidence of 1 in 4,000 among those under 25 years old [1]. The salvage rate of an affected testis largely depends on the duration and degree of torsion [2,3]. Although SCT can be seen at any age, in fact, there have been few reports of older men with SCT [4,5]. Because of its rarity in the older age group, the lack of suspicion for SCT may lead to delayed diagnosis or misdiagnosis. To the best of our knowledge, this seems to be the first reported case of SCT in an aged patient older than 60 years in Korea. Herein, we report this very unusual case of missed SCT occurring in a 63-year-old man.
A 63-year-old man presented with right scrotal pain and swelling. A couple of weeks previously, he had experienced right scrotal pain when he woke up. The scrotal swelling and dull scrotal pain had gradually increased over a few days. He was then seen by a primary care physician. However, the physician failed to find any abnormalities other than epididymal enlargement on scrotal ultrasonography. The patient was then referred because his symptoms did not improve despite empirical antibiotics use. He denied having any history of trauma to the testis, strenuous exercise, sexual activity, or febrile illness. He also had no known sexually transmitted diseases. On physical examination, a swollen, edematous, and erythematous change in the right hemiscrotum was noted. The right testis was enlarged, hard, consistent, and somewhat tender on palpation compared with the intact left testis. The results of a complete blood count, chemistry profile, and urinalysis were normal. Serum levels of α-fetoprotein and β-human chorionic gonadotropin were in the normal range. Gray-scale ultrasonography of the scrotum demonstrated heterogenous echotextures in the right testis that were combined with a thickened scrotal wall and hyperechoic supratesticular mass (Fig. 1A). Color Doppler sonography revealed that blood flow was present in the asymptomatic left testis, but absent in the right testis. An increased blood flow in peritesticular structures adjacent to the nonperfused testis was identified (Fig. 1B). Torsion of the right spermatic cord was strongly suspected judging from the sonographic findings. Although very rare, a few cases of intrascrotal torsion of a testis tumor have been reported [6]. Therefore, we could not absolutely exclude the possibility of a testis tumor and thus planned to perform radical orchiectomy of the symptomatic right testis.
The patient was taken for surgical exploration of the right testis through a right inguinal incision. Severe adhesion and inflammation around the torsed testis were found. Radical orchiectomy was done in the usual manner. The frozen section examination of the right orchiectomy specimen revealed testicular infarction with suppurative inflammation. Hence, left transscrotal orchiopexy was done to prevent contralateral torsion at a later date. An underlying anatomic abnormality, the bell-clapper deformity, was found in the left testis. In the cut section, the right testis was 4.3 cm×3.2 cm×4.2 cm in size and had reddened parenchyma rimmed with several scattered lesions of dirty yellow pus-like exudates. A twisted intravaginal spermatic cord was identified (Fig. 2A). Final histopathological examinations revealed a total hemorrhagic infarct of the testis and diffuse chronic inflammation of the peritesticular soft tissues (Fig. 2B).
The causes of acute scrotal pain vary with age, but in all ages, infection and SCT are the most common etiology. Differentiating SCT from infection in the epididymis or testis is critical. Although intravaginal SCT is primarily a condition of puberty and early adolescence, it is not exclusive to that population. The onset of pain in SCT is usually acute; however, up to 25% of patients also have a gradual onset [7]. Thus, delayed presentation or diagnosis may result in patients with gradual onset of scrotal pain. In addition, age may be another factor that affects the testicular salvage rate. Because SCT is uncommon and is associated with more severe cord twisting in the older aged group, the prognosis of testicular salvage in this age group may be worse [4]. Therefore, a high index of suspicion is the first step to determine the presence of SCT even if symptoms are equivocal in older patients.
Color Doppler ultrasound performed by a trained radiologist proved to be a somewhat more desirable modality because it is performed more rapidly and equal to nuclear scintigraphy with respect to sensitivity and specificity [8]. The sonographic appearance of SCT depends on the duration of the torsion. Patients who are very early in the course of torsion may have only minimal enlargement of the testis with normal or slightly decreased echogenicity. As time goes on, the echogenicity of the testis becomes heterogeneous owing to hemorrhage and necrosis. A swollen epididymis may be also seen because the deferential artery supplying the epididymis is often involved [7]. Particularly, scanning the spermatic cord in the inguinal canal can be helpful. An abrupt increase in the size and alteration of the spermatic cord may be noted below the point of torsion. This finding of a twisted cord is a highly sensitive and specific sign of SCT. In the present case, we suggest some possible reasons for the misdiagnosis during the patient's first visit at the local clinic. In most cases of SCT, the epididymal head is only mildly enlarged, whereas the spermatic cord, which passes just superoposteriorly to the epididymal head, is grossly enlarged. Thus, the swollen spermatic cord may be mistaken for an enlarged epididymal head. In cases of missed torsion, marked hyperemia may exist in the tunica vaginalis, which is adjacent to the testis. This flow may be mistaken for testicular capsular artery flow, thus causing the diagnosis of torsion to be missed [7]. Less likely, a testis with spontaneous detorsion may be hyperemic, simulating epididymo-orchitis.
Because a missed diagnosis is the most frequent medicolegal concern in our litigious society, many urologists logically consider that acute scrotum is SCT until proved otherwise. Clinical symptoms and physical examination are often not enough for prompt diagnosis, especially in cases with delayed presentation. Because the adult type of SCT is thought to be rare, this rarity may result in missed torsion unless special attention is paid to the possibility of SCT. The present unusual case reminds us to maintain suspicion of SCT in males of any age presenting with acute scrotum.
Figures and Tables
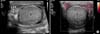 | FIG. 1(A) Gray-scale imaging demonstrates that the right testis shows a heterogeneous echotexture with thickening of the scrotal wall. A twisted cord structure (white arrows) is identified as an echogenic extratesticular mass. (B) Color Doppler ultrasonography shows the complete absence of detectable flow inside the right testis. T, testis. |
 | FIG. 2(A) Gross appearance of the specimen. The cord appears as a twisted breadstick within the thickened vaginalis. (B) Microscopic finding. Hemorrhagic testicular infarct of this case reveals typical coagulative necrosis of almost the entire seminiferous tubules in the background of stromal hemorrhage (H&E, ×100). |
References
1. Anderson JB, Williamson RC. Testicular torsion in Bristol: a 25-year review. Br J Surg. 1988; 75:988–992.
2. Cuckow PM, Frank JD. Torsion of the testis. BJU Int. 2000; 86:349–353.
3. Ellati RT, Kavoussi PK, Turner TT, Lysiak JJ. Twist and shout: a clinical and experimental review of testicular torsion. Korean J Urol. 2009; 50:1159–1167.
4. Cummings JM, Boullier JA, Sekhon D, Bose K. Adult testicular torsion. J Urol. 2002; 167:2109–2110.
5. Allen B, Ball AJ, Desai A. Delayed presentation of acute scrotum: a rare age for torsion. Intern Emerg Med. 2010; 5:553–554.
6. Seaman EK, Sawczuk I. Testis tumor in an adult presenting with torsion of testis. Urology. 1993; 42:453–454.
7. Stavros A, Rapp C, McGrath J. Color duplex sonography of acute scrotal pain. In : Bluth EI, Arger PH, Benson CB, Ralls PW, Siegel MJ, editors. Ultrasound: a practical approach to clinical problems. New York: Thieme;2000. p. 135–152.
8. Kalfa N, Veyrac C, Lopez M, Lopez C, Maurel A, Kaselas C, et al. Multicenter assessment of ultrasound of the spermatic cord in children with acute scrotum. J Urol. 2007; 177:297–301.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download