INTRODUCTION
Most bladder squamous cell carcinomas have been described in paraplegics or in patients with spinal trauma. They are also known to occur in patients with long-term indwelling catheters and during chronic inflammatory states associated with frequent irritation and persistent infection. Here we report a case study of a patient who developed a squamous cell carcinoma involving the bladder mucosa from a well-healed suprapubic cystostomy scar after 9 years.
CASE REPORT
A 56-year-old male patient who had a suprapubic Foley catheter for 9 years after the formation of an urethrocutaneous fistula presented with a spontaneous suprapubic urinary leak from a well-healed suprapubic cystostomy tract scar. He originally had a urethral stricture that required multiple surgical corrections for 16 years beginning at the age of 28 years. Nineteen years later (at the age of 47 years), a urethrocutaneous fistula occurred spontaneously and a suprapubic cystostomy tube was eventually required for urinary diversion.
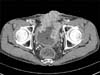
Physical examination revealed an erythematous lesion in the abdominal wall enveloping the suprapubic catheter. The result of ThinPrep smear urine cytology was suspicious of malignancy. Cystoscopy revealed a bladder mass in the dome. Ultrasound examination of the kidneys did not show any dilatation. On the computed tomographic (CT) scan of the abdomen, a tumor mass surrounding the suprapubic cystostomy tract was clearly visible (Fig. 1). Transurethral biopsy of the bladder mass was performed. Histological examination of the biopsy from the bladder mass revealed squamous cell carcinoma, moderately differentiated, probably originating from the vesicocutaneous fistula tract involving the bladder mucosa (Fig. 2).
The patient did not want to undergo aggressive surgical excision of the complete bladder and the abdominal wall and underwent radiation therapy. Although a CT scan of the abdomen after radiation therapy showed partial remission (Fig. 3), the patient died of lung metastasis and pneumonia at 6 months after the start of radiation therapy.
DISCUSSION
Squamous cell carcinoma is a rare form of carcinoma of the bladder that accounts for only 5% of such carcinomas [1]. It is usually caused by chronic irritation from urinary calculi, long-term indwelling catheters, chronic urinary infections, or bladder diverticula. As many as 80% of paraplegics with chronic infections or indwelling catheters experience squamous changes in the bladder, and about 5% develop squamous cell carcinoma [2]. Cigarette smoking is also significantly associated with an increased risk of bladder squamous cell carcinoma [3]. Male predominance is far less striking in squamous cell carcinoma (male to female ratio, 1.3:1 to 1.7:1) [4].
There are only four case reports of suprapubic catheter tract squamous cell carcinoma (two of them involving the bladder) in the English literature [5-8]. The case reported here is the third case of suprapubic catheter tract squamous cell carcinoma extending into the bladder. We present the published cases of suprapubic catheter tract squamous cell carcinoma in Table 1.
The prolonged presence of a tube with continuous irritation of the tract site leading to metaplasia and carcinoma provides a possible mechanism for carcinoma [6]. In the literature, a 10% incidence of squamous cell carcinoma of the bladder has been noted in patients who have had indwelling catheters for more than 10 years [5]. Kaufman et al. [9] found that spinal cord injury patients who have had indwelling catheters for more than 10 years have a 20% prevalence of squamous cell carcinoma of the bladder, and those authors advocated for periodic cystoscopies combined with random bladder biopsies for this category of patients.
Because this type of cancer is extremely rare, insufficient experience exists to postulate the etiology in cases that present several years later in a well-healed suprapubic catheter tract site. Persistent discharge is often attributed to recurrence of stricture, for which cystostomies are frequently performed, leading to missed malignancies. These lesions are usually localized and are best treated by radical excisional surgery because of the rapid death of conservatively treated patients [1]. Bladder involvement generally dictates surgical management because long-term survival benefits resulting from radiotherapy or chemotherapy have not been reported to date [8].
However, the patient in our study chose not to undergo planned aggressive surgical excision of the complete bladder and the abdominal wall and was instead treated with radiation therapy. He died 6 months after the start of radiation therapy owing to lung metastasis and pneumonia.
Several reports suggest that the stage-by-stage prognosis of squamous cell carcinoma is comparable to that of transitional cell carcinoma [10]. The prognosis of suprapubic catheter tract squamous cell carcinoma is comparatively poor because most patients have advanced disease at the time of diagnosis.
In conclusion, persistent discharge from a well-healed suprapubic catheter scar site several years after a cystostomy should be grounds for suspicion of this rare clinical entity, and an excisional biopsy should always be performed, especially when no stricture or bladder pathology is detectable on cystoscopy. This case study underscores the need for close monitoring of patients with any type of long-term indwelling catheter.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download