Abstract
Purpose
We evaluated oncologic outcomes following radical prostatectomy (RP) in patients with a Gleason score (GS) of 7 with tertiary Gleason pattern 5 (TGP5).
Materials and Methods
We retrospectively reviewed the medical records of 310 patients who underwent RP from 2005 to 2010. Twenty-four patients who received neoadjuvant or adjuvant antiandrogen deprivation or radiation therapy were excluded. Just 239 (GS 6 to 8) of the remaining 286 patients were included in the study. Patients were classified into four groups: GS 6, GS 7 without TGP5, GS 7 with TGP5, and GS 8. We analyzed preoperative clinical factors, postoperative pathological outcomes, and biochemical recurrence (BCR).
Results
TGP5 in GS 7 was an independent predictor of primary Gleason pattern 4, tumor volume larger than 10%, positive surgical margin, and lymphovascular invasion. The presence of TGP5 in GS 7 was not associated with BCR-free survival. Subgroup analyses revealed that BCR-free survival did not differ significantly between patients with GS 7 with TGP5 and those with GS 8 (p=0.120). In addition, time to BCR in patients with a higher percentage of TGP5 was shorter than that in patients with a lower percentage of TGP5. TGP5 in GS 7 was not a significant predictive factor for BCR, whereas prostate-specific antigen density and a positive surgical margin were shown to be independent predictors of BCR.
Radical prostatectomy (RP) is the definitive treatment for localized prostate cancer [1,2]. Many investigators have reported predictive factors for biochemical recurrence (BCR), such as preoperative prostate-specific antigen (PSA), pathological stage, the Gleason score (GS), and surgical margin status [3,4].
For needle biopsy specimens, both the primary pattern and the highest grade should be added to derive the GS. Unlike needle biopsy, however, it would be misleading to derive the GS by adding the most common Gleason pattern and the highest Gleason pattern on RP specimens. Therefore, in RP specimens, the routine GS consisting of the most prevalent and the second most prevalent architectural patterns should be recorded along with a note stating that there is a tertiary high-grade pattern. It was the consensus of the group that one assigns the GS for a RP specimen on the basis of the primary and secondary patterns with a comment as to the tertiary pattern [5,6].
In RP specimens, GS 7 is the most commonly assigned grade, ranging in frequency from 30% to 50%. GS 7 tumors have been shown to behave significantly worse than tumors with a GS of 6 or less and to have a better prognosis than those with a GS of 8 or more [7]. However, GS 7 tumors have heterogeneous features. Multiple authors have reported differences in recurrence-free survival among patients with Gleason pattern 4+3 and patients with Gleason pattern 3+4 tumors following RP. Chan et al. [8] found that the 5-year actuarial risk of progression was 15% and 40% for Gleason score 3+4 and 4+3 tumors, respectively. Ro et al. [9] revealed that the 5-year BCR-free survival for patients with primary Gleason grades of 3 or 4 was 85.4% and 66.7%, respectively (p<0.001). Patients with GS 7 tumors and a tertiary Gleason pattern 5 (TGP5) appear to have more advanced pathological features and increased rates of biochemical progression compared with patients without a TGP5 component [8]. In contrast with the above study, TGP5 was not an independent factor for BCR-free survival in patients in the GS 7 and GS 8 groups in another study [10]. However, there are few studies on the characteristics of GS 7 disease with TGP5 after RP [5-7,10,11-17]. Thus, we evaluated pathological and oncologic outcomes following RP in patients with GS 7 with TGP5.
We retrospectively reviewed the medical records of 310 patients who underwent RP from January 2005 to December 2010. Twenty-four patients who underwent neoadjuvant antiandrogen deprivation (11 patients) or adjuvant antiandrogen deprivation therapy (ADT) or radiation therapy (10 patients) as well as patients with histomorphological post-ADT cancer (2 patients) or pathological stage T0 (1 patient) were excluded. Just 239 (GS 6 to 8) of the remaining 286 patients were included in the study. The patients were classified into four groups: GS 6 (62 patients), GS 7 without TGP5 (132 patients), GS 7 with TGP5 (35 patients), and GS 8 (10 patients).
We analyzed not only preoperative factors such as age, preoperative PSA, total prostate volume, preoperative PSA density (PSAD), digital rectal examination, biopsy GS, percentage biopsy positive cores, and clinical stage, but also postoperative pathological outcomes, including pathological stage, RP GS, percentage tumor volume (%TV), prostatic intraepithelial neoplasia, positive surgical margin (PSM), lymphovascular invasion (LVI), perineural invasion, and BCR.
RP specimens were reviewed by a single experienced pathologist. Pathological examinations were performed by using the whole-mount step-section technique. After the seminal vesicles were removed, the prostate specimens were fixed and serially-sectioned at 3 mm intervals. The pathological stage of RP was determined by using the 2010 TNM classification [18]. Final GS was reviewed according to the 2005 International Society of Urological Pathology (ISUP) Consensus on Gleason grading of prostate cancer [6]. On all slides involved with tumor, the tumor area was marked and the %TV (overall tumor percentage for the entire prostate and percentage tertiary pattern 5 cancer within the tumor) was calculated on the basis of the cumulative percentages of tumor on each slide divided by the number of slides with a significant volume of prostate tissue.
Postoperative follow-up was performed by serum PSA measurements at intervals of 1 to 3 months. BCR was defined as PSA greater than 0.2 ng/mL following an initial postoperative PSA level of less than 0.1 ng/mL [10].
The chi-square test and Mann-Whitney U test were performed to compare the clinical and pathological characteristics between the GS 7 without TGP5 and GS 7 with TGP5 groups. Logistic regression analyses were used for the prediction of pathologic outcomes according to TGP5 in GS 7. The BCR-free survival of each GS group was compared by using the Kaplan-Meier method with the log-lank test. Cox proportional hazards models were used to assess the risk factors of BCR. Statistical analysis was performed with SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA) and statistical significance was defined as a p-value of <0.05.
Mean follow-up time was 33.7±18.7 months. Of the 239 patients, the number of patients with GS 6, GS 7 without TGP5, GS 7 with TGP5, and GS 8 was 62 (25.9%), 132 (55.2%), 35 (14.5%), and 10 (4.2%), respectively. The comparisons of clinical and pathological characteristics between the GS 7 groups with and without TGP5 are summarized in Table 1. PSAD (p=0.022), pathological stage (p=0.037), primary Gleason pattern 4 (p≤0.001), %TV (p= 0.001), presence of PSM (p=0.004), and LVI (p≤0.001) were higher in the GS 7 group with TGP5 than in the group without TGP5.
In logistic regression analyses (after adjustment for age, preoperative PSA, total prostate volume, and digital rectal examination) for prediction of pathologic outcomes, GS 7 with TGP5 was an independent predictor of primary Gleason pattern 4 (p=0.007), %TV larger than 10% (p= 0.011), PSM (p=0.012), and LVI (p≤0.001) (Table 2).
Kaplan-Meier survival analysis revealed that the presence of TGP5 in GS 7 was not associated with BCR-free survival (p=0.306). In further subgroup analyses, the BCRfree survival of the group with GS 7 without TGP5 differed from that of the groups with GS 6 and GS 8 (p=0.038 and p=0.008). However, BCR-free survival did not show any significant difference between patients with GS 7 with TGP5 and patients with GS 8 (p=0.120) (Fig. 1). Additionally, in analyses according to the percentage of TGP5, time to BCR was shorter in patients with a higher percentage of TGP5 (≥5%) than in those with a lower percentage of TGP5 (<5%, 61 months vs. 17 months, p=0.044) (Fig. 2).
In the multivariate analysis for assessment of independent predictors of BCR by use of the Cox proportional hazards model, TGP5 in GS 7 was not a significant predictive factor for BCR (p=0.442). However, PSAD (HR, 3.87; p= 0.006) and PSM (HR, 3.22; p=0.002) were shown to be independent predictors of BCR (Table 3).
The GS is an important predictor of BCR and disease-specific survival in men with prostate cancer after definitive treatment [19]. The ISUP Consensus Conference on Gleason Grading on Prostatic Carcinoma decided in 2005 that the GS should include the primary and secondary patterns, with a separate comment on the presence of a tertiary pattern of a higher grade in the RP specimen [6]. Recent studies suggest that the tertiary pattern is significant to pathological outcomes and BCR. A tertiary pattern is observed in 7.5% to 48% of specimens and is associated with BCR [6,10-15]. In our study, among a total of 239 patients, 167 (70%) had GS 7 tumors and 35 of them (21%) had TGP5 in GS 7, which is comparable to findings in other recent studies.
Our results showed that patients with GS 7 with TGP5 had higher PSAD, pathological stage, GS, %TV, presence of PSM, and LVI than did patients with GS 7 without TGP5. Also, logistic regression analyses revealed that TGP5 in GS 7 was an independent predictor of primary Gleason pattern 4, %TV larger than 10%, PSM, and LVI. The association between the presence of a TGP5 and adverse histopathological features, such as higher GS, pathologic stage, extracapsular extension, LVI, and PSM has been confirmed in several publications [11,16,17]. Interestingly, in terms of correlation between TGP5 and primary Gleason pattern 4, a positive but inverse correlation was reported in previous studies [7,11,16]. Primary Gleason pattern 4 tumors are significantly more likely to contain TGP5 than are tumors with a primary Gleason pattern 3 in GS 7 (Mosse et al., 58% vs 32%; Whittemore et al., 41% vs 10%; and Hattab et al., 41% vs 9%).
In many previous studies, the presence of a tertiary pattern in RP specimens was associated with a higher risk of biochemical failure than that in patients without a tertiary pattern [5,7,12,13,16,17]. Whittemore et al. [16] noted that patients with GS 7 with TGP5 cancer had significantly lower BCR-free survival than did patients with GS 7 cancer (p=0.001). BCR was significantly altered by the presence of a TGP5 in patients with primary Gleason pattern 3 compared with patients with a primary Gleason pattern 4. The overall 5-year BCR-free survival rates for patients with GS 7 tumors and GS 7 with TGP5 tumors were 70% and 40%, respectively. However, Hashine et al. [10] found the 5- and 10-year BCR-free survival rates in the GS 7 group were 78.4% and 75.0%, respectively, among patients with no TGP5 and were 75.4% and 75.4%, respectively, in patients with TGP5. Similarly, our data showed that the presence of TGP5 in GS 7 was not associated with BCR (p=0.306).
In the further subgroup analyses, as for BCR-free survival, there was a considerable difference between patients with GS 6 and those with GS 7 without TGP5 (p=0.038), but no significant difference was found between patients with GS 7 with TGP5 and those with GS 8 (p=0.120). That is to say, a notable finding was that, unlike GS 7 without TGP5, GS 7 with TGP5 had a similar rate of BCR to GS 8. Therefore, the absence of TGP5 does not necessarily mean a better prognosis, but the presence of TGP5 clearly indicates a worse prognosis. These data suggest that GS is an important predictive factor for BCR and that the presence of TGP5 has a potential impact on disease progression.
Pan et al. [5] showed that patients with GS 7 with TGP5 tumors had significantly higher pathological stages and shorter times to BCR than did those with GS 7 tumors but that these variables did not differ statistically from patients with GS 8 tumors. Mosse et al. [11] found that adverse pathological features were significantly associated with GS 7 with TGP5 tumors in patients with primary Gleason pattern 3 compared with patients with primary Gleason pattern 4. Turker et al. [14] revealed shorter BCR-free survival rates for GS <7 with tertiary Gleason component (TGC) tumors than for GS <7 tumors without TGC (p<0.0001) and similar BCR-free survival rates to GS 3+4 tumors. Similarly, GS (3+4) with TGC tumors had shorter BCR-free survival rates than did GS 3+4 tumors without TGC (p=0.001), and GS (4+3)+TGC tumors had shorter BCR-free survival rates than did GS 4+3 tumors without TGC (p=0.04). However, GS (3+4)+TGC, GS (4+3)+TGC, and GS >7 tumors had similar 5-year BCRfree survival (p>0.5). Thus, we suggest that TGP5 in GS 7 tumors should always be reported in RP specimens.
There are few published data on the percentage of TGP5. Pan et al. [5] suggested that tertiary TV and volume ratio do not correlate with progression. The results of this analysis did not differ after deleting those cases with a tertiary volume ratio more than 5%. In contrast, we found that time to BCR was shorter in patients with a higher percentage of TGP5 (≥5%) than that in patients with a lower percentage of TGP5 (<5%, 61 months vs. 17 months, respectively; p=0.044).
In many previous studies, TGP5 in GS 7 was a statistically significant predictor of clinical failure when the analysis was adjusted for pathological stage, surgical margin status, extraprostatic extension, and seminal vesicle invasion [7,12,14,17]. However, multivariate analysis showed that TGP5 was not an independent factor for BCR-free survival in patients in the GS 7 and 8 groups [10]. Similarly, in our study, TGP5 was not a significant predictive factor for BCR (HR, 0.76; p=0.442). However, PSAD (HR, 3.87; p=0.006) and PSM (HR, 3.22; p=0.002) were shown to be independent predictors of BCR in GS 7.
There were some limitations to our study. First, it was based on a relatively small sample size, which consequently lowered the statistical power, especially for the subgroup analyses. Furthermore, because of its retrospective nature, it had the possibility of selection bias, although all of the RP specimens were uniformly reevaluated by an experienced pathologist for this study. This study was based on a relatively short period of time; however, because most BCR occurs within 3 years of surgery, the mean follow-up time was about 3 years and only BCR was assessed. Thus, further research is needed to confirm cancer-specific survival and oncologic outcomes. Despite these limitations, this is the first study to report the significance and characteristics of TGP5 in GS 7 cancer after RP in Korea.
TGP5 in GS 7 was an independent predictor of primary Gleason pattern 4, %TV larger than 10%, PSM, and LVI. The BCR-free survival of GS 7 with TGP5 was similar to that of GS 8. Also, a higher percentage of TGP5 (≥5%) was associated with a shorter time to BCR in our study. Therefore, TGP5 should be reported in RP specimens. Larger prospective studies are required to assess the predictive value of TGP5 compared with other parameters in predicting the long-term oncologic outcome after RP.
Figures and Tables
FIG. 1
Kaplan-Meier survival analysis of patients with GS 6 vs. GS 7 without TGP5, GS7 without TGP5 vs. GS 7 with TGP5, GS7 without TGP5 vs. GS 8, and GS 7 with TGP5 vs. GS 8. GS, Gleason score; TGP5, tertiary Gleason pattern 5; BCR, biochemical recurrence; RP, radical prostatectomy.
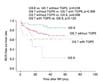
FIG. 2
Kaplan-Meier survival analysis of patients with GS 7 with <5% vs. ≥5% TGP5. GS, Gleason score; TGP5, tertiary Gleason pattern 5; BCR, biochemical recurrence; RP, radical prostatectomy.

TABLE 1
Comparisons of clinical and pathological characteristics between Gleason score 7 without and with TGP5

References
1. Roehl KA, Han M, Ramos CG, Antenor JA, Catalona WJ. Cancer progression and survival rates following anatomical radical retropubic prostatectomy in 3,478 consecutive patients: long-term results. J Urol. 2004; 172:910–914.
2. Lim TJ, Lee JH, Lim JW, Moon SK, Jeon SH, Chang SG. Preoperative factors predictive of continence recovery after radical retropubic prostatectomy. Korean J Urol. 2012; 53:524–530.
3. Uhlman MA, Sun L, Stackhouse DA, Caire AA, Polascik TJ, Robertson CN, et al. Tumor volume, tumor percentage involvement, or prostate volume: which is predictive of prostate-specific antigen recurrence? Urology. 2010; 75:460–466.
4. Min SH, Park YH, Lee SB, Ku JH, Kwak C, Kim HH. Impact of prostate size on pathologic outcomes and prognosis after radical prostatectomy. Korean J Urol. 2012; 53:463–466.
5. Pan CC, Potter SR, Partin AW, Epstein JI. The prognostic significance of tertiary Gleason patterns of higher grade in radical prostatectomy specimens: a proposal to modify the Gleason grading system. Am J Surg Pathol. 2000; 24:563–569.
6. Epstein JI, Allsbrook WC Jr, Amin MB, Egevad LL. ISUP Grading Committee. The 2005 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma. Am J Surg Pathol. 2005; 29:1228–1242.
7. Hattab EM, Koch MO, Eble JN, Lin H, Cheng L. Tertiary Gleason pattern 5 is a powerful predictor of biochemical relapse in patients with Gleason score 7 prostatic adenocarcinoma. J Urol. 2006; 175:1695–1699.
8. Chan TY, Partin AW, Walsh PC, Epstein JI. Prognostic significance of Gleason score 3+4 versus Gleason score 4+3 tumor at radical prostatectomy. Urology. 2000; 56:823–827.
9. Ro YK, Lee S, Jeong CW, Hong SK, Byun SS, Lee SE. Biochemical recurrence in Gleason score 7 prostate cancer in korean men: significance of the primary Gleason grade. Korean J Urol. 2012; 53:826–829.
10. Hashine K, Yuasa A, Shinomori K, Shirato A, Ninomiya I, Teramoto N. Tertiary Gleason pattern 5 and oncological outcomes after radical prostatectomy. Jpn J Clin Oncol. 2011; 41:571–576.
11. Mosse CA, Magi-Galluzzi C, Tsuzuki T, Epstein JI. The prognostic significance of tertiary Gleason pattern 5 in radical prostatectomy specimens. Am J Surg Pathol. 2004; 28:394–398.
12. Sim HG, Telesca D, Culp SH, Ellis WJ, Lange PH, True LD, et al. Tertiary Gleason pattern 5 in Gleason 7 prostate cancer predicts pathological stage and biochemical recurrence. J Urol. 2008; 179:1775–1779.
13. van Oort IM, Schout BM, Kiemeney LA, Hulsbergen CA, Witjes JA. Does the tertiary Gleason pattern influence the PSA progression-free interval after retropubic radical prostatectomy for organ-confined prostate cancer? Eur Urol. 2005; 48:572–576.
14. Turker P, Bas E, Bozkurt S, Gunlusoy B, Sezgin A, Postacı H, et al. Presence of high grade tertiary Gleason pattern upgrades the Gleason sum score and is inversely associated with biochemical recurrence-free survival. Urol Oncol. 2013; 31:93–98.
15. Isbarn H, Ahyai SA, Chun FK, Budaus L, Schlomm T, Salomon G, et al. Prevalence of a tertiary Gleason grade and its impact on adverse histopathologic parameters in a contemporary radical prostatectomy series. Eur Urol. 2009; 55:394–401.
16. Whittemore DE, Hick EJ, Carter MR, Moul JW, Miranda-Sousa AJ, Sexton WJ. Significance of tertiary Gleason pattern 5 in Gleason score 7 radical prostatectomy specimens. J Urol. 2008; 179:516–522.
17. Servoll E, Saeter T, Vlatkovic L, Lund T, Nesland J, Waaler G, et al. Impact of a tertiary Gleason pattern 4 or 5 on clinical failure and mortality after radical prostatectomy for clinically localised prostate cancer. BJU Int. 2012; 109:1489–1494.
18. Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010; 17:1471–1474.
19. Eggener SE, Scardino PT, Walsh PC, Han M, Partin AW, Trock BJ, et al. Predicting 15-year prostate cancer specific mortality after radical prostatectomy. J Urol. 2011; 185:869–875.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download