Abstract
Purpose
To investigate the prevalence of Chlamydia trachomatis (CT), Neisseria gonorrhoeae (NG), Mycoplasma genitalium (MG), and Ureaplasma urealyticum (UU) in first-voided urine samples and to determine the factors associated with positivity for sexually transmissible microorganisms in healthy, middle-aged Korean men.
Materials and Methods
Five hundred fifty-one men who came to the hospital for a general prostate health checkup were tested between August 2011 and December 2011. PCR assays for CT, NG, MG, and UU were done with first-voided urine samples and the prevalence of microorganism positivity and association with several clinical parameters were evaluated.
Results
The mean age of the men studied was 50.8±4.7 years. Among the 551 men, 72 (13.1%) had a positive result for at least one microorganism; one (0.2%) had two different species. The overall prevalence of asymptomatic sexually transmitted infections was 11.1% (61/551). The prevalence rates of CT, NG, MG, and UU infection in the general population were 0.4% (2/551), 0.0% (0/551), 1.0% (6/551), and 11.8% (65/551), respectively. CT-positive patients had a lower mean age than did CT-negative patients. There were no significant differences in symptoms by positivity of each microorganism.
Conclusions
We checked the prevalence rates of four microorganisms, the proportion of symptomatic people, and the association of microbes, age, and symptoms, as the baseline data for Korean middle-aged men. In this population, CT, NG, MG, and UU infections do not seem to be symptomatic. However, the potential role of CT in young men and of UU in middle-aged men with a high rate of detection should be studied continuously as a source of opportunistic infection.
Sexually transmitted disease (STD) is a clinical syndrome caused by pathogens that can be acquired and transmitted through sexual activity. Bacteria, viruses, fungi, protozoa, and epizoa are known pathogens of STDs. Even today, the incidence of STDs is still high in developing countries, and developing countries are affected by several pathogens disproportionately [1,2]. Bacterial pathogens causing STDs are not usually found in prostatic tissue, urine, or prostatic fluid by conventional culture. In addition, routine culture may give negative results for generally healthy men who recently experienced unprotected sexual contact and have acquired an STD [3]. Furthermore, there are silent patients in the community who can serve as a reservoir of the STD [4]. Thus, recognizing the existence of yet unknown infectious pathogens and establishing strategies for the diagnosis and treatment of STDs are very important issues.
The growing health burden of STDs and their spiraling costs has led to a need for rapid and reliable laboratory techniques to identify the causative pathogens and to thereby reduce complication rates and disease spread [5]. Several clinical studies have relied on nonculture methods, such as polymerase chain reaction (PCR) [6-9]. PCR has distinct advantages over culture and other standard methods with respect to rapidity and sensitivity [10,11]. Many kinds of samples are used for PCR. Among them, a previous study showed that with the use of a standard sample preparation method, male first-voided urine is superior to urethral swabs for detection of Mycoplasma genitalium (MG) and Chlamydia trachomatis (CT) [12]. In addition, urine sampling is noninvasive and rapid.
For a long time, many sexually transmitted infection (STI)-inducing strains have been suspected as the cause of prostatitis. The etiology of nonbacterial chronic prostatitis (CP) remains obscure. Although bacterial etiology has frequently been suggested, evidence of both bacterial involvement in CP and the presence of normal bacterial flora in the prostate remain uncertain. The clinical question is whether infection is important in the etiology of CP.
Until now, as far as we know, there have been no studies in the English literature regarding the incidence of CT, Neisseria gonorrhoeae (NG), MG, and Ureaplasma urealyticum (UU) infection in healthy middle-aged Korean men or about the relationship of such organisms and prostatitis-like symptoms. The purpose of this study was therefore to investigate the prevalence of CT, NG, MG, and UU in first-voided urine samples by PCR methods and to determine the associated factors, including the National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI) and age, among middle-aged men being seen for a general health checkup at our institution.
During 5 months beginning in August 2011, 702 men (age, over 40 years), all of whom worked as policemen, participated in a general prostate health checkup program of their own accord. Initially, individuals who had any history of STD, such as any urethritis, syphilis, or chancroid; who had a positive urine culture for bacteria by use of Gram stain; or who had a history of treatment of benign prostatic hyperplasia, overactive bladder, CP, pelvic irradiation or neuropathic bladder were excluded from the study. Finally, 551 men were enrolled in this study. Prostatitis-like symptoms were quantified by the NIH-CPSI. The symptoms were regarded as being prostatitis-like if the respondents reported perineal or ejaculatory pain and had an NIH-CPSI pain score of ≥4 [13]. The study was approved by the institutional review board and ethical committee, and informed consent was obtained from all participants.
The assay was performed by the real-time PCR DNA detection method. Real-time PCR involved the selective amplification of a target sequence while monitoring the progress of amplification in real time through the use of a visualizing agent, such as fluorescent dyes (MG and UU, FAM; CT&NG, CT-FAM; NG, Texas Red). Monitoring of the amplified product was conducted by labeling the hydrolysis probe with a matched pair of fluorescent dyes. Owing to fluorescence resonance energy transfer, an intact probe would not emit light. However, upon cleavage by the 5'-3' exonuclease activity of the DNA polymerase during PCR, dyes would emit a specific wavelength (FAM, 520 nm; Texas Red, 610 nm) of light within the visible spectrum after binding to the amplicon.
All patients had a complete history, physical examination, and urine culture. CT, NG, MG, and UU were all tested in first-voided urine samples. First-voided urine specimens were collected in sterile 50 mL screw-cap plastic bottles. The specimens from the 551 men were equilibrated to room temperature and centrifuged at 5000×g for 15 minutes. The supernatant was discarded, and the pellet was resuspended in 1 mL resuspension (RS) buffer before DNA extraction. Genomic DNA was extracted from the pretreated specimens by using an automated DNA extraction instrument, ExiPrep 16 Dx (Cat. No. A-5050, Bioneer Co., Daejeon, Korea), and the ExiPrep Dx bacteria genomic DNA Kit (Cat. No. K-4414, Bioneer Co.), which is a DNA extraction kit optimized to the instrument. Extracted DNA was amplified by using a thermal cycler, Exicycler 96 real-time quantitative thermal block (Cat. No. A-2060M, Bioneer Co.), and commercial premix kits: AccuPower CT&NG real-time PCR Kit (Cat. No. STD2A-1111, Bioneer Co.), AccuPower MG real-time PCR Kit (Cat. No. MPG-1111, Bioneer Co.), and AccuPower UU real-time PCR Kit (Cat. No. UUU-1111, Bioneer Co.).
Before performing PCR, we made a premix reconstitution mixture by combining 44 µL of PCR-grade water and 1 µL of internal positive control per reaction. After adding 45 µL of the premix reconstitution mixture to all the premix tubes, 5 µL of nucleic acid extracts was added to the tubes except from control tubes. After sealing the tubes, we mixed the tubes thoroughly by using ExiSpin (Cat. No. A-7040, Bioneer Co.) to dissolve the premix pellet with the DNA extracts.
The process was evaluated by amplification of a tobacco mosaic virus genome as an internal positive control measure. Positive and negative control reactions were also included in each batch of amplifications. The positive control consisted of DNA extracted from microorganism-confirmed positive cultures. Negative controls consisted of DNA extracted from urine of healthy subject and blank tubes containing just distilled water. The assay was considered positive when one of the PCR products was present. Precautions to avoid cross-contamination and false-positive results were taken in every assay.
Statistical analysis was performed by using the PASW ver. 18.0 (IBM Co., Armonk, NY, USA). Chi-square or Fisher's exact test was used to compare nominal or categorical variables and independent sample t-test was used to test the significant differences between the means. For all analyses, p<0.05 was considered statistically significant.
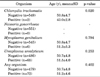
A total of 551 men were enrolled in this study. The patients' mean age was 50.8±4.7 years (Table 1). The mean pain, urinary, quality of life (QoL), and total NIH-CPSI scores were 2.2±3.0, 2.9±2.3, 3.7±2.4, and 8.9±6.4, respectively. Seventy-two (13.1%) men had at least one microorganism in their genitourinary tract. The prevalences of CT, NG, MG, and UU in the study population were 0.4% (2/551), 0.0% (0/551), 1.0% (6/551), and 11.8% (65/551), respectively (Table 2). The most common infection in the urinary tract was UU. In one person (0.2%), two microorganisms (MG and UU) were detected at the same time.
Among the 551 men, 95 (17.2%) had a prostatitis-like symptom (Table 1). CT-positive patients did not have symptoms; by contrast, 16.7% (1/6) and 15.4% (10/65) of MG- and UU-positive patients, respectively, had symptoms. However, MG- and UU-negative patients showed similar results for symptoms (17.2% and 17.5%, respectively). In the asymptomatic group, 13.4% of patients had any detected microorganism. CT, NG, MG, and UU were detected in 0.4%, 0.0%, 1.1%, and 12.1%, respectively (Table 3). Comparison of the mean age, according to CT, NG, MG, and UU positivity in the study group, is shown in Table 4. The mean age was lower when CT was identified than when not identified (p=0.020). For the other organisms, no significant differences were seen in the mean age between the positive and negative groups. In addition, the pain, urinary, QoL, and total NIH-CPSI scores according to organism positivity were analyzed (Table 5). However, there were no significant differences between the positive and negative groups of each microorganism.
Genitourinary tract infections are a major cause of morbidity in sexually active individuals worldwide. The World Health Organization has reported that STDs rank second in importance after cancer among diseases in women for which treatment is possible [14]. Our study showed that the incidence of CT, NG, MG, and UU positivity was 0.4%, 0.0%, 1.0%, and 11.8% among general middle-aged men, respectively. In asymptomatic men, the detection rates of each microorganism were 0.4%, 0.0%, 1.1%, and 12.1%, respectively. Our results confirm that there are many silent infections in the community.
Mason et al. [15] reported that the prevalence of CT in asymptomatic men is 4%. One Japanese study reported that CT was detected in 6% of samples from healthy young Japanese men [16]. Fortunately, in our study, CT was observed in only 2 persons (0.4%) in the asymptomatic group. However, most asymptomatic patients are neglected unless they visit the clinic to be evaluated for STI by chance or face complications, such as urethritis. In addition, CT infection is usually not detected by routine microbiologic diagnosis. Although gonorrhea can be diagnosed by inspection of the yellowish discharge from the urethra, many patients infected with NG have no discharge. Furthermore, 10% of infected men and 50% of infected women are asymptomatic. Regardless of age, one surveillance study reported prevalence rates of NG in healthy people of 0.06% to 0.18% [17]. In our study, the detection rate in asymptomatic people was 0.0%. This is similar to the previous result. This suggests that, in healthy people, the probability of silent NG infection is minimal. MG is known as a causative pathogen of nongonococcal urethritis (NGU). In British data, Ross et al. [18] reported a detection rate of 0.6% for MG in asymptomatic persons. In Japan, the detection rates of urinary MG in one study were 1% in the total group and 1.3% in asymptomatic men [16]. Another report showed that 1.1% of asymptomatic men were positive for MG [19]. Our study showed that the detection rates of MG in the symptomatic and asymptomatic groups were 1.0% and 1.1%. These results are similar to those of the previous studies. Wikstrom and Jensen [20] reported that MG is a common cause of recurrent urethritis among doxycycline-refractory or erythromycin-refractory men. As a silent pathogen, screening for this pathogen is important to identify asymptomatic individuals who have a history of STI [3,4].
The detection rate of UU was relatively higher than that of the other STI pathogens in our study. UU is frequently isolated from the urethra of healthy men. Hooton et al. [21] reported that there is no significant difference in the prevalence of UU infection between men with NGU and men without NGU. On the other hand, there are some reports that UU serves as a cause of persistent NGU [22,23]. Thus, UU is sometimes recognized as a pathogen and sometimes as a commensal microorganism. Japanese studies have reported that the detection rates of UU in the urine specimens of asymptomatic men range from 9.5% to 12.0% [16,24]. In our study, the detection rates of UU in the asymptomatic and symptomatic groups were 12.1% and 10.5%, respectively. Although additional data determining whether UU is a definitive pathogen of urethritis will be required, our data suggest that UU might colonize in the urethra without any symptoms.
The bacterial component is incontrovertible in acute and chronic bacterial prostatitis [25] but questionable in category III CP [26]. The results of studies that have used PCR to define the role of bacteria in the pathogenesis of CP and the presence of the bacterial flora harbored by the normal prostate are controversial and difficult to compare owing to methodological differences. The involvement of bacteria in CP is supported by many studies [27], whereas other studies have failed to demonstrate normal bacterial flora in the prostate or any clear connection between bacteria and chronic pelvic pain syndrome [28]. Lee et al. [29] reported that conventional bacterial cultures of prostate biopsy specimens failed to show any differences between men with and without CP.
In the current study, first-voided urine samples from 72 (13.1%) of the 551 patients were found to contain 1 or more pathogens and 95 (17.2%) of the patients had a prostatitis-like symptom. There were no associations between prostatitis-like symptoms and bacterial positivity for any organism. Thus, we analyzed the association between bacterial positivity and pain, urinary, QoL, and total NIH-CPSI scores, according to organism positivity. However, there were no significant differences in symptom scores between the positive and negative groups of each microorganism. Thus, in our study, involvement of bacteria did not appear to be associated with CP-like symptoms. This suggests the importance of treatment of silent or latent infection with these organisms, such as in the case of CT.
Our data showed that there are age differences according to the isolated microorganism. CT-positive patients were younger than were CT-negative patients. A Western group also reported age-based estimates. Younger patients had a higher prevalence than did older. Fenton et al. [30] showed that age-specific prevalence was highest among men aged 25 to 34 years. These findings of increased chlamydia among young men echo our findings.
A number of factors may contribute to the variation between the findings of the current study and earlier studies. First, our study is the first study of the relevance of STI, NIH-CPSI symptom score, and age in Korea. Second, unlike existing studies, a well-defined and relatively homogeneous group of patients was studied, because our study group consisted of middle-aged men receiving a general health checkup. Third, the number of subjects was larger than in the previous domestic study. Fourth, only first-voided urine specimens were used for PCR. Fifth, the data were collected intensively for a short period of 5 months. Thus, the present results are contemporary results that are not influenced by a time-trend effect.
There were several limitations to this study. First, our study did not compare actual clinical patients with CP strains with asymptomatic persons. Second, the age range of the study population was relatively narrow because we included men in their 40s to 50s only. Third, we could not compare our results with clinical factors such as sexual history and marital status. Finally, the occupation of the targeted group was policemen only. We do not know if this had an effect on the results. In the future, it would be beneficial to compensate for these weak points to achieve better results.
Our study reports the prevalence rates of CT, NG, MG, and UU as baseline data for Korean middle-aged men. Patients in whom chlamydia was detected had a lower mean age than did those in whom it was not detected. The four microorganisms did not seem to induce symptoms in this population. However, the potential role of chlamydia for young men and UU for middle-aged men with a high rate of detection should be studied as a source of opportunistic infection.
Figures and Tables
TABLE 2
Frequency of single and coinfection of Chlamydia trachomatis, Neisseria gonorrhoeae, Mycoplasma genitalium, and Ureaplasma urealyticum in first-voided urine of 551 men

References
1. Aral S, Over M, Manhart L, Holmes KK. Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, editors. Sexually transmitted infections. Disease control priorities in developing countries. 2006. 2nd ed. New York: Oxford University Press;311–330.
2. Wellings K, Collumbien M, Slaymaker E, Singh S, Hodges Z, Patel D, et al. Sexual behaviour in context: a global perspective. Lancet. 2006. 368:1706–1728.
3. Centers for Disease Control and Prevention. Workowski KA, Berman SM. Sexually transmitted diseases treatment guidelines, 2006. MMWR Recomm Rep. 2006. 55(RR-11):1–94.
4. Leblanc MM. When to refer an infertile mare to a theriogenologist. Theriogenology. 2008. 70:421–429.
5. Lee SR, Chung JM, Kim YG. Rapid one step detection of pathogenic bacteria in urine with sexually transmitted disease (STD) and prostatitis patient by multiplex PCR assay (mPCR). J Microbiol. 2007. 45:453–459.
6. Jensen JS, Uldum SA, Sondergard-Andersen J, Vuust J, Lind K. Polymerase chain reaction for detection of Mycoplasma genitalium in clinical samples. J Clin Microbiol. 1991. 29:46–50.
7. Palmer HM, Gilroy CB, Furr PM, Taylor-Robinson D. Development and evaluation of the polymerase chain reaction to detect Mycoplasma genitalium. FEMS Microbiol Lett. 1991. 61:199–203.
8. Abele-Horn M, Wolff C, Dressel P, Zimmermann A, Vahlensieck W, Pfaff F, et al. Polymerase chain reaction versus culture for detection of Ureaplasma urealyticum and Mycoplasma hominis in the urogenital tract of adults and the respiratory tract of newborns. Eur J Clin Microbiol Infect Dis. 1996. 15:595–598.
9. Watson EJ, Templeton A, Russell I, Paavonen J, Mardh PA, Stary A, et al. The accuracy and efficacy of screening tests for Chlamydia trachomatis: a systematic review. J Med Microbiol. 2002. 51:1021–1031.
10. Cosentino LA, Landers DV, Hillier SL. Detection of Chlamydia trachomatis and Neisseria gonorrhoeae by strand displacement amplification and relevance of the amplification control for use with vaginal swab specimens. J Clin Microbiol. 2003. 41:3592–3596.
11. Stellrecht KA, Woron AM, Mishrik NG, Venezia RA. Comparison of multiplex PCR assay with culture for detection of genital mycoplasmas. J Clin Microbiol. 2004. 42:1528–1533.
12. Jensen JS, Bjornelius E, Dohn B, Lidbrink P. Comparison of first void urine and urogenital swab specimens for detection of Mycoplasma genitalium and Chlamydia trachomatis by polymerase chain reaction in patients attending a sexually transmitted disease clinic. Sex Transm Dis. 2004. 31:499–507.
13. Litwin MS, McNaughton-Collins M, Fowler FJ Jr, Nickel JC, Calhoun EA, Pontari MA, et al. The National Institutes of Health chronic prostatitis symptom index: development and validation of a new outcome measure. Chronic Prostatitis Collaborative Research Network. J Urol. 1999. 162:369–375.
14. De Schryver A, Meheus A. Epidemiology of sexually transmitted diseases: the global picture. Bull World Health Organ. 1990. 68:639–654.
15. Mason PR, Gwanzura L, Gregson S, Katzenstein DA. Chlamydia trachomatis in symptomatic and asymptomatic men: detection in urine by enzyme immunoassay. Cent Afr J Med. 2000. 46:62–65.
16. Takahashi S, Takeyama K, Miyamoto S, Ichihara K, Maeda T, Kunishima Y, et al. Detection of Mycoplasma genitalium, Mycoplasma hominis, Ureaplasma urealyticum, and Ureaplasma parvum DNAs in urine from asymptomatic healthy young Japanese men. J Infect Chemother. 2006. 12:269–271.
17. Centers for Disease Control and Prevention. Gonorrhea: transmitted disease surveillance 2007. 2008. Atlanta: Division of STD Prevention.
18. Ross JD, Brown L, Saunders P, Alexander S. Mycoplasma genitalium in asymptomatic patients: implications for screening. Sex Transm Infect. 2009. 85:436–437.
19. Uno M, Deguchi T, Saito A, Yasuda M, Komeda H, Kawada Y. Prevalence of Mycoplasma genitalium in asymptomatic men in Japan. Int J STD AIDS. 1997. 8:259–260.
20. Wikstrom A, Jensen JS. Mycoplasma genitalium: a common cause of persistent urethritis among men treated with doxycycline. Sex Transm Infect. 2006. 82:276–279.
21. Hooton TM, Roberts MC, Roberts PL, Holmes KK, Stamm WE, Kenny GE. Prevalence of Mycoplasma genitalium determined by DNA probe in men with urethritis. Lancet. 1988. 1:266–268.
22. Stimson JB, Hale J, Bowie WR, Holmes KK. Tetracycline-resistant Ureaplasma urealyticum: a cause of persistent nongonococcal urethritis. Ann Intern Med. 1981. 94:192–194.
23. Yoshida T, Ishiko H, Yasuda M, Takahashi Y, Nomura Y, Kubota Y, et al. Polymerase chain reaction-based subtyping of ureaplasma parvum and ureaplasma urealyticum in first-pass urine samples from men with or without urethritis. Sex Transm Dis. 2005. 32:454–457.
24. Yoshida T, Maeda S, Deguchi T, Ishiko H. Phylogeny-based rapid identification of mycoplasmas and ureaplasmas from urethritis patients. J Clin Microbiol. 2002. 40:105–110.
25. Weidner W, Schiefer HG, Krauss H, Jantos C, Friedrich HJ, Altmannsberger M. Chronic prostatitis: a thorough search for etiologically involved microorganisms in 1,461 patients. Infection. 1991. 19:Suppl 3. S119–S125.
26. Berger RE, Krieger JN, Kessler D, Ireton RC, Close C, Holmes KK, et al. Case-control study of men with suspected chronic idiopathic prostatitis. J Urol. 1989. 141:328–331.
27. Krieger JN, Riley DE. Bacteria in the chronic prostatitis-chronic pelvic pain syndrome: molecular approaches to critical research questions. J Urol. 2002. 167:2574–2583.
28. Hochreiter WW, Duncan JL, Schaeffer AJ. Evaluation of the bacterial flora of the prostate using a 16S rRNA gene based polymerase chain reaction. J Urol. 2000. 163:127–130.
29. Lee JC, Muller CH, Rothman I, Agnew KJ, Eschenbach D, Ciol MA, et al. Prostate biopsy culture findings of men with chronic pelvic pain syndrome do not differ from those of healthy controls. J Urol. 2003. 169:584–587.
30. Fenton KA, Korovessis C, Johnson AM, McCadden A, McManus S, Wellings K, et al. Sexual behaviour in Britain: reported sexually transmitted infections and prevalent genital Chlamydia trachomatis infection. Lancet. 2001. 358:1851–1854.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download