Abstract
Purpose
Enterococcus faecalis is one of the most common pathogens linked to chronic bacterial prostatitis (CBP). Owing to a limited number of previous studies addressing this topic, we aimed to determine the drug resistance patterns of E. faecalis strains isolated from CBP patients.
Materials and Methods
One thousand twenty-one patients visited a single hospital owing to chronic prostatitis for 5 years. Culture specimens were obtained by use of a modified Meares-Stamey method. The minimal inhibitory concentrations of the antimicrobials were assessed by use of the Vitek II microbial identification system as suggested by the Clinical and Laboratory Standards Institute.
Results
Forty-one samples from 41 patients who had significant E. faecalis loads for defining CBP were included in this study. The E. faecalis strains in our study were resistant to penicillin (9.7%), ampicillin (0%), ampicillin/sulbactam (0%), nitrofurantoin (0%), imipenem (0%), vancomycin (0%), teicoplanin (0%), quinupristin/dalfopristin (100%), ciprofloxacin (9.7%), levofloxacin (4.8%), norfloxacin (26.8%), erythromycin (95%), gentamicin (46.3%), tetracycline (97.5%), and trimethoprim/sulfamethoxazole (31.5%), respectively.
Conclusions
Fluoroquinolones have been the preferred antibiotics for treating CBP. Because of their low rate of drug resistance, fluoroquinolones are suitable therapeutic agents for E. faecalis strains causing CBP in Korea. Even though tetracycline, erythromycin, and trimethoprim/sulfamethoxazole have been prescribed as an empirical antimicrobial therapy for chronic prostatitis, we cannot recommend these drugs for treatment of E. faecalis isolates because of the high rates of drug resistance.
Chronic bacterial prostatitis (CBP) is diagnosed when a patient has recurrent urinary tract infections (UTIs) caused by bacteria localized in the prostate. Because it is a relapsing and indolent disease with occasional acute exacerbations, CBP is difficult to treat [1]. The clinical picture of chronic prostatitis or CBP is one of recurrent episodes of inflammatory voiding symptoms such as frequency, urgency, or dysuria, which are often associated with suprapubic, genital, perineal, or lower back pain [2,3].
Aerobic gram-negative enteric bacteria have been well documented as the pathogens commonly associated with CBP [1,4]. Even though the role of gram-positive bacteria in CBP has been controversial, it is well known that Enterococcus faecalis is one of the most prevalent etiologic pathogens in CBP [5,6].
The approach to treating CBP largely focuses on empirical antibiotic therapy. Various fluoroquinolones have become the standard therapy for CBP [1,7]. Trimethoprim (TMP) or trimethoprim-sulfamethoxazole (TMP-SMX), tetracycline, and macrolides are also well known as a traditional second-line treatment of CBP [8,9]. To be effective as therapeutic agents for CBP, the ideal antibiotics must be able to diffuse and easily penetrate into the prostate tissue. In addition, the ideal antibiotic also shows bacteriocidal susceptibility for each drug [1,9,10].
The current management of chronic prostatitis is usually a long course of empirical antibiotic therapy [10]. Although fluoroquinolones are not the recommended antibiotic for treatment of enterococcal UTIs, fluoroquinolones are the drug of choice for chronic prostatitis [1,11]. Generally, these antibiotics are tried without performing a urine or prostate culture or susceptibility testing to guide the therapy. Unfortunately, the increasing antibiotic resistance today affects the success rate of this empirical treatment. Furthermore, fluoroquinolone resistance by gram-negative enteric bacteria has been detected at a high rate in the Asia-Pacific region in recent years [12]. Moreover, patients with CBP are usually treated with inadequate, longer, and repetitive empirical antibiotic therapies because of recurrent episodes of CBP.
The fluoroquinolone-resistant patterns of gram-negative enteric bacteria in UTI have been well studied [12,13]. To our knowledge, however, few studies have focused on E. faecalis strains isolated from the prostate, even though these organisms are the second most common cause of CBP. Furthermore, there are few reported data on the antibiotic resistance patterns of E. faecalis from CBP for clinicians to use when choosing an appropriate empirical therapy. Many urologists believe that the bacterial culture step from prostatic secretion is critical or important for characterizing infection. However, they usually do not perform the time-consuming prostate culture step.
Nowadays, because the identification of enterococci and the determination of their resistance patterns are important for choosing an empirical treatment, we aimed to determine the antibiotic resistance patterns of E. faecalis strains isolated from CBP patients in Korea.
One thousand twenty-one patients visited a single university hospital owing to symptoms suggestive of chronic prostatitis from September 2007 to March 2012. None had taken antimicrobial or anti-inflammatory drugs during the 4 weeks before the evaluation.
According to the National Institutes of Health (NIH) definition, CBP (Category II, NIH-National Institute of Diabetes and Digestive and Kidney Diseases) is diagnosed when pathogens are cultured from a chronically infected prostate in patients suffering from repeated prostate-specific symptomatic episodes [14]. The syndrome is characterized by an array of signs and symptoms, including perineal pain, testicular pain and/or other forms of pelvic pain, irritative and/or obstructive bladder symptoms, ejaculatory pain, and sexual dysfunction [14,15].
Culture specimens for diagnosing CBP were obtained by using a modified Meares-Stamey method [16,17]. In brief, after periurethral cleansing with an alcohol sponge, the patient provided a VB1 specimen consisting of the initial 5 to 10 mL of voided urine, followed by a VB2 urine specimen. After production of expressed prostatic secretions (EPS) by digital prostatic massage, the patient provided 5 to 10 mL of voided urine for the VB3 specimen.
Only one VB1 and one EPS specimen were enrolled per person. Each VB1 specimen was cultured within 4 hours of collection by spreading 100 µL onto plates containing 5% sheep blood and MacConkey's agar, incubated aerobically, and examined for bacterial growth after 48 hours. Similarly, 100 µL of EPS was cultured onto the same culture plates for 2 days. The criterion for CBP was that the bacterial colony concentration of the EPS specimens increased by at least 10-fold (one log) compared with the colony numbers of the VB1 specimen.
The minimal inhibitory concentrations (MICs) of the antimicrobials were assessed by use of the Vitek II microbial identification system (bioMérieux, Marcy-I'Etoile, France) as suggested by the Clinical and Laboratory Standards Institute [12]. The test results were expressed as MICs with interpretation of the category of microbial susceptibility as susceptible, intermediate, or resistant strains.
Patients were excluded from the analysis if they had active urethral discharge and were also excluded if they had bacteriuria, gross hematuria, or a urologic diagnosis other than CBP.
Forty-one samples from 1,021 patients (mean age, 61.12±12 years) with significant E. faecalis loads for defining CBP were included in this study. For easy handling of the data, we placed the E. faecalis isolates with intermediate resistance into the resistant categories of each antimicrobial.
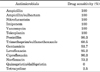
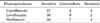
All 41 stains from 41 patients were sensitive to ampicillin, ampicillin/sulbactam, nitrofurantoin, imipenem, vancomycin, and teicoplanin; 90.3% were sensitive to penicillin; 68.5% to TMP-SMX; and 53.7% to gentamicin. The quinolone sensitivity of the E. faecalis strains was as follows: 95.2% were sensitive to levofloxacin, 90.3% to ciprofloxacin, and 73.2% to norfloxacin, respectively. Finally, E. faecalis strains in our study were highly resistant to quinupristin/dalfopristin (100%), erythromycin (95%), and tetracycline (97.5%) (Table 1). The ciprofloxacin intermediate-resistance strains revealed drug sensitivity to levofloxacin. However, ciprofloxacin-resistant E. faecalis consistently showed drug resistance to levofloxacin (Table 2). Finally, in Table 3 we summarize the antimicrobial sensitivity of the E. faecalis isolates in this study and in prostatic penetration studies of the drugs as reviewed in the literature.
It is commonly known that only 5% to 10% of chronic prostatitis patients have a bacterial infection detectable by conventional cultures. CBP is a persistent infection of the prostate characterized by poor quality of life mainly due to frequent relapsing episodes caused by incomplete eradication of the causative pathogens [18]. Aggressive antibacterial therapy is required to attenuate the severe symptoms of CBP and to achieve a permanent cure.
Broad consensus exists for the use of fluoroquinolones as first-line antibacterial agents for the treatment of CBP. International guidelines recommend a 4- to 12-week course of ciprofloxacin, lomefloxacin, ofloxacin, levofloxacin, or norfloxacin for the eradication of susceptible pathogens [1,7,13].
Norfloxacin and ofloxacin are indicated for the management of CBP caused by E. coli, and ciprofloxacin has been approved for CBP caused by E. coli or Proteus mirabilis [19]. In addition, levofloxacin is approved for the treatment of CBP caused by E. coli, E. faecalis, or Staphylococcus epidermidis. However, the norfloxacin sensitivity of the E. faecalis strains from our study was 73.2%. Even though norfloxacin has good penetration into the prostate, norfloxacin treatment for CBP caused by E. faecalis is not currently justified in Korea [20]. Ciprofloxacin has good penetration into the prostate and a good prostate tissue-to-plasma ratio [21]. It is well known that ciprofloxacin is currently the most appropriate antimicrobial agent for the treatment of CBP. Thirty-seven samples revealed ciprofloxacin-sensitive E. faecalis, 2 samples had intermediate sensitivity to ciprofloxacin, and the last 2 samples showed ciprofloxacin resistance. Levofloxacin sensitivity was shown in 95.2% of the E. faecalis samples in our study. Furthermore, the samples that showed intermediate resistance to ciprofloxacin had antimicrobial sensitivity to levofloxacin. However, ciprofloxacin-resistant E. faecalis also consistently showed drug resistance to levofloxacin (Table 2). This finding was also found in our previous study of antimicrobial resistance patterns in Korean patients with acute uncomplicated cystitis [12]. In addition, levofloxacin shows a broad antibacterial spectrum for both gram-negative and gram-positive pathogens from CBP. Furthermore, it is dosed on a once-daily basis and displays significant penetration into the prostate with a favorable prostate tissue-to-plasma ratio [22]. For these reasons, we conclude that levofloxacin may have better cure rates for E. faecalis from CBP than any other fluoroquinolones such as norfloxacin and ciprofloxacin.
All E. faecalis strains from our study revealed 100% drug sensitivity to ampicillin and ampicillin/sulbactam and 90.3% drug sensitivity to penicillin. However, natural penicillin or penicillin derivatives penetrate very poorly into the human prostate [23]. Even though E. faecalis strains in vitro show high drug susceptibility to these antimicrobials, these drugs have typically shown very low pharmacokinetic levels in prostatic fluid or tissues.
Nitrofurantoin is widely used for the treatment of UTI. In addition, the E. faecalis strains in our study showed high drug sensitivity to this antibiotic. Nitrofurantoin is a lipid-soluble weak acid that is somewhat favorable for diffusion into prostatic fluid. However, low levels of nitrofurantoin were achieved in prostatic fluid in dogs, and the administration of standard oral doses of this drug to men results in lower therapeutic levels in blood [23,24]. Half of E. faecalis strains showed gentamicin sensitivity in our study. Aminoglycosides do not penetrate prostatic tissue well, and the prostatic tissue levels of these antibiotics are probably inadequate to eradicate gram-negative bacteria [25]. Furthermore, the oral form of aminoglycosides has not yet been developed. For these reasons, aminoglycosides cannot be recommended as the ideal therapeutic drug for E. faecalis strains isolated from CBP.
TMP with or without SMX has traditionally been the first-line treatment of CBP. It has been shown that TMP concentrations in the human prostate are 2 to 3 times higher than those in plasma [26]. TMP with or without SMX can be both theoretically and to some extent experimentally ideal for gram-negative enterococcal strains from CBP. However, increased drug resistance to TMP-SMX, probably as a result of the indiscriminate use of this drug in CBP patients, has recently been evidenced [27-29]. Furthermore, TMP may appear active in vitro but is not effective clinically. We suggest that TMP-SMX may not be an ideal antibiotic for E. faecalis in CBP because the drug sensitivity of the strains in our study to TMP-SXM was 68.5%.
Tetracycline or tetracycline derivatives have been prescribed as ideal drugs for the treatment of chronic prostatitis. Most tetracyclines have high lipid solubility, an important factor for ideal antibiotics for the treatment of CBP. However, Quinones et al [30] reported that the tetracycline resistance rate in E. faecalis was 78.6%, which is similar to our findings. For this reason, tetracycline is not recommended for eradicating the E. faecalis infection in CBP in Korea.
Imipenem, vancomycin, and teicoplanin have traditionally been reserved as drugs of last resort and are used after treatment with other antibiotics has failed. However, organisms resistant to these drugs are now common worldwide. In our study, we did not find any drug resistance to imipenem, vancomycin, or teicoplanin among the E. faecalis strains isolated from patients with CBP. From a pharmacokinetic aspect, imipenem has been shown to achieve good concentrations in prostatic tissue [23]. There are few data on the use of vancomycin and teicoplanin in chronic prostatitis.
Quinupristin/dalfopristin is a combination of two antibiotics used to treat infections by staphylococci and by vancomycin-resistant Enterococcus faecium. However, we cannot recommend this drug for treatment of E. faecalis isolates from CBP patients because of high drug resistance.
We have summarized the antimicrobial sensitivity of the E. faecalis isolates in this study and in prostatic penetration studies of the drugs from literature reviews in Table 3.
E. faecalis is one of the most common pathogens in CBP. Fluoroquinolones are strongly recommended as a standard therapeutic agent for CBP caused by E. faecalis. Even though levofloxacin and ciprofloxacin are suitable therapeutic agents for the treatment of patients with CBP, levofloxacin may have better cure rates for E. faecalis from CBP than any other fluoroquinolones such as norfloxacin and ciprofloxacin.
Figures and Tables
TABLE 1
Antimicrobial sensitivity of Enterococcus faecalis isolated from the prostate of patients with chronic bacterial prostatitis
References
1. Naber KG, Busch W, Focht J. The German Prostatitis Study Group. Ciprofloxacin in the treatment of chronic bacterial prostatitis: a prospective, non-comparative multicentre clinical trial with long-term follow-up. Int J Antimicrob Agents. 2000. 14:143–149.
2. Nickel JC, Shoskes DA. Phenotypic approach to the management of the chronic prostatitis/chronic pelvic pain syndrome. BJU Int. 2010. 106:1252–1263.
3. Sharp VJ, Takacs EB, Powell CR. Prostatitis: diagnosis and treatment. Am Fam Physician. 2010. 82:397–406.
4. Meares EM Jr. Bacterial prostatitis vs "prostatosis". A clinical and bacteriological study. JAMA. 1973. 224:1372–1375.
5. Weidner W, Schiefer HG, Krauss H, Jantos C, Friedrich HJ, Altmannsberger M. Chronic prostatitis: a thorough search for etiologically involved microorganisms in 1,461 patients. Infection. 1991. 19:Suppl 3. S119–S125.
6. Cai T, Mazzoli S, Meacci F, Boddi V, Mondaini N, Malossini G, et al. Epidemiological features and resistance pattern in uropathogens isolated from chronic bacterial prostatitis. J Microbiol. 2011. 49:448–454.
7. Panagopoulos P, Antoniadou A, Kanellakopoulou K, Tsiodras S, Katsarolis I, Papadopoulos A, et al. Fluoroquinolone treatment of chronic bacterial prostatitis: a prospective cohort study. J Chemother. 2009. 21:317–321.
8. Milingos S, Creatsas G, Messinis J, Lolis D, Kaskarelis D. Treatment of chronic prostatitis by consecutive per os administration of doxycycline, sulfamethoxazole/trimethoprim, and cephalexin. Int J Clin Pharmacol Ther Toxicol. 1983. 21:301–305.
9. Baumuller A. Antimicrobials for the treatment of bacterial prostatitis. Historical developments and current trends. Scand J Urol Nephrol Suppl. 1987. 104:97–99.
10. Thakkinstian A, Attia J, Anothaisintawee T, Nickel JC. α-blockers, antibiotics and anti-inflammatories have a role in the management of chronic prostatitis/chronic pelvic pain syndrome. BJU Int. 2012. 110:1014–1022.
11. Dalhoff A, Weidner W. Diffusion of ciprofloxacin into prostatic fluid. Eur J Clin Microbiol Infect Dis. 1988. 7:438–439.
12. Lee G, Cho YH, Shim BS, Lee SD. Risk factors for antimicrobial resistance among the Escherichia coli strains isolated from Korean patients with acute uncomplicated cystitis: a prospective and nationwide study. J Korean Med Sci. 2010. 25:1205–1209.
13. Jang WH, Yoo DH, Park SW. Prevalence of and risk factors for levofloxacin-resistant E. coli isolated from outpatients with urinary tract infection. Korean J Urol. 2011. 52:554–559.
14. Krieger JN, Nyberg L Jr, Nickel JC. NIH consensus definition and classification of prostatitis. JAMA. 1999. 282:236–237.
15. Nickel JC. Prostatitis: evolving management strategies. Urol Clin North Am. 1999. 26:737–751.
16. Meares EM, Stamey TA. Bacteriologic localization patterns in bacterial prostatitis and urethritis. Invest Urol. 1968. 5:492–518.
17. Krieger JN, Ross SO, Limaye AP, Riley DE. Inconsistent localization of gram-positive bacteria to prostate-specific specimens from patients with chronic prostatitis. Urology. 2005. 66:721–725.
18. Lee KS, Choi JD. Chronic prostatitis: approaches for best management. Korean J Urol. 2012. 53:69–77.
19. Nickel JC, Downey J, Clark J, Ceri H, Olson M. Antibiotic pharmacokinetics in the inflamed prostate. J Urol. 1995. 153:527–529.
20. Chen J, Chen RR, Huang HS. Comparison of ofloxacin and norfloxacin concentration in prostatic tissues in patients undergoing transurethral resection of the prostate. J Formos Med Assoc. 2001. 100:548–552.
21. Grabe M, Forsgren A, Bjork T. Concentrations of ciprofloxacin in serum and prostatic tissue in patients undergoing transurethral resection. Eur J Clin Microbiol. 1986. 5:211–212.
22. Drusano GL, Preston SL, Van Guilder M, North D, Gombert M, Oefelein M, et al. A population pharmacokinetic analysis of the penetration of the prostate by levofloxacin. Antimicrob Agents Chemother. 2000. 44:2046–2051.
23. Charalabopoulos K, Karachalios G, Baltogiannis D, Charalabopoulos A, Giannakopoulos X, Sofikitis N. Penetration of antimicrobial agents into the prostate. Chemotherapy. 2003. 49:269–279.
24. Dunn BL, Stamey TA. Antibacterial concentrations in prostatic fluid. 1. Nitrofurantoin. J Urol. 1967. 97:505–507.
25. Dyderski S, Sokołowski W. Gentamicin level in the prostate and its pharmacokinetics in patients with benign prostatic hypertrophy. Pol Tyg Lek. 1990. 45:517–519.
26. Oosterlinck W, Defoort R, Renders G. The concentration of sulphamethoxazole and trimethoprim in human prostate gland. Br J Urol. 1975. 47:301–304.
27. Schaeffer AJ, Darras FS. The efficacy of norfloxacin in the treatment of chronic bacterial prostatitis refractory to trimethoprim-sulfamethoxazole and/or carbenicillin. J Urol. 1990. 144:690–693.
28. Fowler JE Jr. Antimicrobial therapy for bacterial and nonbacterial prostatitis. Urology. 2002. 60:6 Suppl. 24–26.
29. Sharer WC, Fair WR. The pharmacokinetics of antibiotic diffusion in chronic bacterial prostatitis. Prostate. 1982. 3:139–148.
30. Quinones D, Goni P, Rubio MC, Duran E, Gomez-Lus R. Enterococci spp. isolated from Cuba: species frequency of occurrence and antimicrobial susceptibility profile. Diagn Microbiol Infect Dis. 2005. 51:63–67.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download