Abstract
Purpose
To evaluate the validity of the University of California San Francisco Cancer of the Prostate Risk Assessment-S score (CAPRA-S score), a biochemical indicator of recurrent prostate cancer that uses histopathologic data, in Korean prostate cancer patients.
Materials and Methods
A total of 203 prostate cancer patients who underwent radical prostatectomy between February 1997 and November 2010 were observed for longer than 6 months. The CAPRA-S score of 134 patients for whom records were available for preoperative prostate-specific antigen (PSA), pathologic specimen Gleason score, surgical margin, seminal vesicle invasion, extracapsular extension, and lymph node invasion were calculated. Biochemical recurrence was defined as repetitive measurement of PSA ≥0.2 ng/mL at least 6 months after surgery with at least a 4-week interval. The Cox proportional hazard model and Kaplan-Meier analysis were used for the statistical testing.
Results
The CAPRA-S scores were divided into nine groups. The 5-year disease-free survival rate was reduced as the CAPRA-S score increased compared with the group with a CAPRA-S score of 0-1. The CAPRA-S score in this study was more sensitive to biochemical recurrence than was the CAPRA score conducted at this institution (CAPRA-S concordance index, 0.776; CAPRA concordance index, 0.728).
Approximately 217,730 persons were diagnosed with prostate cancer in the United States in 2010, which makes up 28% of all cancers in men. Of the 217,730 persons, 32,250 died, which is the second highest mortality rate of male cancers despite the small number when considering the number of people diagnosed [1]. Therefore, risk assessment is essential in prostate cancer in both high-risk and low-risk patients to avoid the potential effects of additional treatment on quality of life.
Cooperberg et al. [2] proposed the Cancer of the Prostate Risk Assessment (CAPRA) score, which is a prognosis-predicting method that uses age, clinical stage, prostate-specific antigen (PSA) before surgery, biopsy Gleason score, and malignancy ratio of the biopsy cores. The accuracy of the CAPRA score has been verified in the United States and Europe [3-6].
However, the clinical stage, biopsy Gleason score, and malignancy ratio of the biopsy cores, 3 of the variables that define the CAPRA score, can overestimate or underestimate the actual stage or the range of cancer [7]. Information on pathologic specimen Gleason score (pGS), surgical margin (SM), extracapsular extension (ECE), seminal vesicle invasion (SVI), and lymph node invasion (LNI) that can be obtained after prostate resection may help to assess the risk of cancer [8]. Accordingly, Cooperberg et al. [9] proposed the CAPRA-S score, which uses additional information that can be obtained after surgery and that can predict relapse of cancer accurately and easily.
The aim of the present study was therefore to assess the validity of applying the CAPRA-S score, which is an assessment measure of biochemical recurrence (BCR) that uses histopathologic data after prostate cancer surgery, to Koreans.
In 2011, Cooperberg et al. [9] analyzed the data of 3,837 patients who underwent prostatectomy in UCSF Cancer of the Prostate Strategic Urologic Research Endeavor (CaPSURE, University of California, San Francisco, CA, USA) to investigate the CAPRA-S score and reported that it can be applied to the prediction of BCR after surgery and for determining suitable treatment [9]. On the basis of these findings, 203 prostate cancer patients who underwent radical prostatectomy between February 1997 and November 2010 were observed for longer than 6 months and the CAPRA-S score of 134 patients for whom records for preoperative PSA, pGS, SM, SVI, ECE, and LNI were available were calculated. BCR was defined as repetitive measurement of PSA ≥0.2 ng/mL at least 6 months after surgery with at least a 4-week interval.
The purpose of the CAPRA-S score is to predict BCR more accurately than with existing pathologic data. The CAPRA-S score was calculated by using PSA, SM, SVI, pGS, ECE, and LNI (Table 1). These variables were each verified for BCR by use of the Cox proportional hazards regression model (Table 2).
For statistical analysis, we used a Cox proportional hazards regression model and Kaplan-Meier survival analysis by use of IBM SPSS ver. 18.0 (IBM Co., Armonk, NY, USA).
The 134 patients were divided into groups with a CAPRA-S score of 0, 1, 2, 3, 4, 5, 6, 7, 8 and ≥9, respectively, (Table 1), and survival analysis was performed for each group (Fig. 1). Of the 134 patients, 16 patients had a CAPRA-S score of 0, 15 patients had a score of 1, 13 patients had a score of 2, 17 patients had a score of 3, 12 patients had a score of 4, 13 patients had a score of 5, 11 patients had a score of 6, 6 patients had a score of 7, 11 patients had a score of 8, and 20 patients had a score of 9 or higher.
When the patients were divided according to CAPRA-S score into 10 groups, the 5-year disease-free survival rate was predicted in each group differently. Although the groups with scores of 4 and 8 showed different tendencies for 5-year disease-free survival from the other neighboring groups, overall, the 5-year disease-free survival rate decreased with increasing CAPRA-S score (p=0.03) (Fig. 1).
SM positivity showed statistical significance with a hazard ratio (HR) of 1.663 (p=0.048), and pGS also showed statistical significance (HR, 1.603; p=0.01). The statistical significance of other variables could not be verified.
The survival rate was analyzed according to the CAPRA-S score, with a score of 0-2 as the low-risk group, a score of 3-5 as the intermediate-risk group, and a score of 6 and higher as the high-risk group. The 5-year disease-free survival rate differed significantly between the groups (p=0.002) (Fig. 2).
Radical prostatectomy is done in more than one third of all patients diagnosed with prostate cancer. Some of the patients scheduled for surgery experience BCR, and some of these patients experience clinical recurrence and metastasis, eventually leading to death. Variation in the postoperative PSA level helps to identify high-risk patients, but there are demerits such as the need for repetitive tests and delayed initiation of some treatments such as radiation therapy and hormonal therapy. Also, a number of high-risk patients, in whom only restricted pathological factors were considered, can avoid the morbidity caused by additional treatment because they do not progress after surgery [10-12].
Recently, several models for predicting biochemical outcomes after prostatectomy have been reported, and the validity of the prediction formula suggested by Bauer et al. [13], the nomogram developed by Kattan et al. [14], and the updated version of Stephenson et al. [15] have been verified externally on the basis of standard clinical and pathological variables. The c-index of these models is reported to be in the range of 0.77 to 0.86, and the possibility of non-progression tends to be exaggerated in high-risk patients. The original CAPRA-S study reported by Cooperberg et al. [9] showed relatively accurate distinction with a c-index of 0.77 [13-15].
The c-index in the present study was 0.776, which indicates that this score can predict the prognosis of prostate cancer in Koreans very accurately. The results, however, represent only relative risks, and continuous correction may be required with the use of additional clinical data.
Two studies have directly compared the pretreatment CAPRA score and the established popular nomogram; one is a United States study that compared the CAPRA score with the original Kattan preoperative nomogram, and the other is a European study that compared the CAPRA score with the updated preoperative nomogram of Stephenson et al. [2,13-15]. The accuracy of the CAPRA score was shown to be similar to these nomograms in these two studies, but the CAPRA score showed superiority in calibration and decision curve analysis in the European study [2,13-15]. Cooperberg et al. [9] reported that the postoperative nomogram, which is different from the CAPRA-S score, shows similar distinction when looking at the calculation by c-index, and the CAPRA-S score showed superiority in calibration and decision curve analysis [13-15].
Cooperberg et al. [2,9] reported that although the CAPRA-S score shows a tendency of relatively many patients converging in the lower score, there was wider patient distribution than the original pretreatment CAPRA score. Therefore, the CAPRA-S score is expected to be more useful for understanding the risk of recurrence and the availability of adjuvant therapy.
The CAPRA-S score shows more diverse score distribution compared with the CAPRA score, which is the preoperative recurrence prediction score, and the CAPRA-S score can be said to be more useful than the CAPRA score at predicting the recurrence risk or determining whether to perform adjuvant therapy because the clinical staging, biopsy Gleason score, and malignancy ratio of the biopsy cores used in the CAPRA score can overestimate or estimate the actual stage or range of cancer [2,9,16-18].
However, it has to be acknowledged that LNI, which is expected to have more influence on recurrence, only contributes 0 to 1 points in the CAPRA-S score despite the fact that the original CAPRA-S score is a pathologic record recorded with various subjective criteria by several pathologists. It seems that although the actual LNI rate is high, lymph node dissection is done restrictively even in high-risk patients in the United States, where the CAPRA-S score was devised. Thus, the score contributed by LNI has been limited to minimize the effects of unknown LNI [19-21]. Therefore, active lymph node dissection as well as giving more contributable points to LNI in the CAPRA-S score must be considered for a more accurate CAPRA-S score in Koreans.
The groups with a CAPRA-S score of 4 and 8 showed different tendencies for the 5-year disease-free survival rate from other neighboring groups. However, it is estimated that this arose as a statistical error owing to the small population number and also owing to the nonequality of score distribution of LNI mentioned before. However, a significant difference was shown when the CAPRA-S score divided into low-risk (1-2), intermediate-risk (3-5), and high-risk (≥6) groups, which is easier for clinical application (p=0.002) (Fig. 2).
Although BCR does not necessarily correlate with the ultimate mortality of prostate cancer, the CAPRA-S score is expected to be able to predict cancer-specific mortality, and it is also expected to be used to predict cancer-specific and overall mortality through accumulation of more patient data and partial correction and supplementation in the future.
Application of the CAPRA-S score in Koreans is significant in that it becomes easier to apply in practice by objectively charting the prediction of prognosis, which is partially dependent on empirical data. The CAPRA-S score can be easily calculated with data on several variables and can be applied to predicting postoperative recurrence and classifying high-risk patients who need adjuvant therapy. However, the relatively few data compared with the United States. studies suggests the necessity of continuous revision using additional clinical data.
Figures and Tables
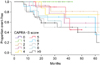 | FIG. 1Five-year disease-free survival rate after radical prostatectomy in terms of likelihood of biochemical progression, stratified by grouped CAPRA-S score: 0, 1, 2, 3, 4, 5, 6, 7, 8, and ≥9 (p=0.03). CAPRA, Cancer of the Prostate Risk Assessment. |
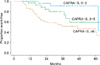 | FIG. 2Five-year disease-free survival rate after radical prostatectomy, stratified by grouped CAPRA-S score in terms of likelihood of biochemical progression: 0-2 indicates relatively low risk; 3-5, intermediate risk; and ≥6, high risk disease (p=0.002). CAPRA, Cancer of the Prostate Risk Assessment. |
References
1. Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010. 60:277–300.
2. Cooperberg MR, Pasta DJ, Elkin EP, Litwin MS, Latini DM, Du Chane J, et al. The University of California, San Francisco Cancer of the Prostate Risk Assessment score: a straightforward and reliable preoperative predictor of disease recurrence after radical prostatectomy. J Urol. 2005. 173:1938–1942.
3. Zhao KH, Hernandez DJ, Han M, Humphreys EB, Mangold LA, Partin AW. External validation of University of California, San Francisco, Cancer of the Prostate Risk Assessment score. Urology. 2008. 72:396–400.
4. Lughezzani G, Budaus L, Isbarn H, Sun M, Perrotte P, Haese A, et al. Head-to-head comparison of the three most commonly used preoperative models for prediction of biochemical recurrence after radical prostatectomy. Eur Urol. 2010. 57:562–568.
5. Cooperberg MR, Freedland SJ, Pasta DJ, Elkin EP, Presti JC Jr, Amling CL, et al. Multiinstitutional validation of the UCSF cancer of the prostate risk assessment for prediction of recurrence after radical prostatectomy. Cancer. 2006. 107:2384–2391.
6. May M, Knoll N, Siegsmund M, Fahlenkamp D, Vogler H, Hoschke B, et al. Validity of the CAPRA score to predict biochemical recurrence-free survival after radical prostatectomy. Results from a european multicenter survey of 1,296 patients. J Urol. 2007. 178:1957–1962.
7. Shariat SF, Karakiewicz PI, Roehrborn CG, Kattan MW. An updated catalog of prostate cancer predictive tools. Cancer. 2008. 113:3075–3099.
8. Cooperberg MR, Broering JM, Carroll PR. Risk assessment for prostate cancer metastasis and mortality at the time of diagnosis. J Natl Cancer Inst. 2009. 101:878–887.
9. Cooperberg MR, Hilton JF, Carroll PR. The CAPRA-S score: a straightforward tool for improved prediction of outcomes after radical prostatectomy. Cancer. 2011. 117:5039–5046.
10. Vickers A. Prediction models in urology: are they any good, and how would we know anyway? Eur Urol. 2010. 57:571–573.
11. Penson DF, Chan JM. Urologic Diseases in America Project. Prostate cancer. J Urol. 2007. 177:2020–2029.
12. Freedland SJ, Humphreys EB, Mangold LA, Eisenberger M, Dorey FJ, Walsh PC, et al. Risk of prostate cancer-specific mortality following biochemical recurrence after radical prostatectomy. JAMA. 2005. 294:433–439.
13. Bauer JJ, Connelly RR, Sesterhenn IA, Bettencourt MC, McLeod DG, Srivastava S, et al. Biostatistical modeling using traditional variables and genetic biomarkers for predicting the risk of prostate carcinoma recurrence after radical prostatectomy. Cancer. 1997. 79:952–962.
14. Kattan MW, Wheeler TM, Scardino PT. Postoperative nomogram for disease recurrence after radical prostatectomy for prostate cancer. J Clin Oncol. 1999. 17:1499–1507.
15. Stephenson AJ, Scardino PT, Eastham JA, Bianco FJ Jr, Dotan ZA, Fearn PA, et al. Preoperative nomogram predicting the 10-year probability of prostate cancer recurrence after radical prostatectomy. J Natl Cancer Inst. 2006. 98:715–717.
16. Messing EM, Manola J, Yao J, Kiernan M, Crawford D, Wilding G, et al. Immediate versus deferred androgen deprivation treatment in patients with node-positive prostate cancer after radical prostatectomy and pelvic lymphadenectomy. Lancet Oncol. 2006. 7:472–479.
17. Thompson IM, Tangen CM, Paradelo J, Lucia MS, Miller G, Troyer D, et al. Adjuvant radiotherapy for pathological T3N0M0 prostate cancer significantly reduces risk of metastases and improves survival: long-term followup of a randomized clinical trial. J Urol. 2009. 181:956–962.
18. Han M, Partin AW, Zahurak M, Piantadosi S, Epstein JI, Walsh PC. Biochemical (prostate specific antigen) recurrence probability following radical prostatectomy for clinically localized prostate cancer. J Urol. 2003. 169:517–523.
19. Burkhard FC, Bader P, Schneider E, Markwalder R, Studer UE. Reliability of preoperative values to determine the need for lymphadenectomy in patients with prostate cancer and meticulous lymph node dissection. Eur Urol. 2002. 42:84–90.
20. Touijer K, Rabbani F, Otero JR, Secin FP, Eastham JA, Scardino PT, et al. Standard versus limited pelvic lymph node dissection for prostate cancer in patients with a predicted probability of nodal metastasis greater than 1%. J Urol. 2007. 178:120–124.
21. Mattei A, Fuechsel FG, Bhatta Dhar N, Warncke SH, Thalmann GN, Krause T, et al. The template of the primary lymphatic landing sites of the prostate should be revisited: results of a multimodality mapping study. Eur Urol. 2008. 53:118–125.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download