Abstract
A 22-year-old young woman presented with dysuria and lower urinary tract symptoms that had persisted for 6 months. She was diagnosed with a tumor near the bladder neck. Transurethral resection was done under anaesthesia. The histopathological examination with immunohistochemical staining showed the tumor to be a low-grade leiomyosarcoma. Adjuvant chemoradiation was given, and the patient has been doing well for 12 months of follow-up. Nonurothelial tumors of the bladder are rare and consensus is lacking regarding their definitive treatment. Furthermore, little is known about the natural history and prognosis of this type of bladder sarcoma. We present a minimally invasive treatment for this relatively rare tumor in which bladder preservation was achieved with no evidence of local or distant recurrences during the follow-up to date.
Nonurothelial tumors of the bladder are rare and account for less than 5% of all bladder malignancies. More than 100 cases of leiomyosarcoma have been reported, which represent 0.1% of all nonurothelial tumors. Consensus is lacking regarding the definitive treatment of this type of bladder sarcoma, and little is known about its natural history and prognosis.
Herein we present the case of a young women in whom a low-grade leiomyosarcoma lying near the bladder neck was diagnosed. Transurethral resection followed by adjuvant chemoradiation was given. The patient has been doing well for 12 months of follow-up with no evidence of local or distant recurrences.
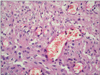
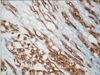
A 22-year-old young woman presented with dysuria and lower urinary tract symptoms (American Urological Association, 12) for 6 months. The results of her general physical examination were unremarkable. Her results on renal function tests, urinalysis, and urine culture sensitivity were within the normal limits. The bladder ultrasound revealed a single bladder mass approximately 2.9 cm×2.7 cm×3 cm in size near the bladder neck. The results of urine cytology for malignant cells were negative. A contrast-enhanced computed tomography (CT) scan showed a well-defined, homogeneous, enhancing endophytic soft tissue lesion near the bladder neck (Fig. 1). Transurethral resection of the bladder mass was done with the patient under general anaesthesia. The histopathological examination revealed a tumor composed of proliferated elongated or spindle-shaped cells disposed in bundles or fascicles or an interlacing pattern (Fig. 2). The cells enclosed ovoid nuclei and fair amounts of lightly stained cytoplasm. There were 3 to 4 mitoses per 10 high-power fields. The immunohistochemical staining showed that the whole specimen was strongly positive for muscle actin, strongly positive for desmin, and negative for pancytokeratin (Fig. 3). The results of the histopathology with immunohistochemical staining were consistent with a low-grade leiomyosarcoma. After consultation with medical and radiation oncologists, adjuvant sequential chemoradiation was done. Six cycles (21 days for each cycle) of ifosfamide and doxorubicin were administered. The therapeutic response was monitored by contrast-enhanced CT and cystoscopic examination, which showed a partial response. Next, external beam fractionated radiotherapy was given (total 60 Grays, 2 Grays/d, 5 days/wk). Postradiation contrast CT scan and cystoscopy revealed no evidence of local disease. The patient has been doing well for 12 months of follow-up, with no evidence of either local or distant recurrences.
Nonurothelial tumors of the bladder are rare and account for less than 5% of all bladder malignancies [1]. More than 100 cases of leiomyosarcoma have been reported, which represent 0.1% of all nonepithelial tumors [2]. Consensus is lacking regarding the definitive treatment of this type of bladder sarcoma, and little is known about its natural history and prognosis [2,3]. The most common clinical presentation is gross hematuria, which is reported in 81% of cases, followed by pollakiuria (28%) and dysuria (19%), respectively [3]. Our case presented in the early third decade of life with lower urinary tract symptoms and dysuria. There was no hematuria. The presentation in our case was at a relatively earlier age than in other cases [3-5]. Surgery with a tumor-free margin is the basic surgical principle for the treatment of leiomyosarcoma. Tumors of a high grade and advanced stage should be treated with radical cystectomy and urinary diversion. Partial cystectomy is reserved for tumors that present at an early stage and a low grade [4,5]. The best prognostic factor is the presence of tumor-free margins. In addition, local invasiveness, tumor size, and tumor grade are other important prognostic factors. The overall local recurrence rate of leiomyosarcoma is about 16%, and most recurrences are seen in the pelvis. Distant metastases are seen in the lungs, liver, bone, and brain. Although there is no general consensus on the treatment of leiomyosarcoma, minimally invasive approaches such as transurethral resection of the tumor and adjuvant chemoradiation are used for patients with small lesions. Long-term survival rates were shown to not differ significantly compared with those in cases who undergo more radical surgery. Partial cystectomy with sole resection of the mass, even when tumor-free margins are achieved, is just a palliative treatment [4,6,7]. The main treatment consists of radical cystectomy, including removal of the uterus, cervix, and vaginal cuff in women. The procedure should include wide resection margins with a 2 to 3 cm depth free from tumor invasion [8,9]. The role of adjuvant chemotherapy remains questionable. In case of metastatic disease, combination chemotherapy (doxorubicin, ifosfamide, cisplatinum, and docetaxel) should be given. In case of a positive surgical margin following surgical intervention, adjuvant radiotherapy should be advocated. Local recurrences should be treated by chemotherapy and/or external beam pelvic radiotherapy. Salvage therapy is ineffective, with a median survival of 20 months after surgery [10].
In the present case, we selected transurethral resection of the bladder tumor followed by sequential chemoradiation. The reasons for this choice were the small size and low grade of the tumor, the lack of radiological evidence of local or distant metastasis, and the location of the tumor near the bladder neck. The location of the tumor did not allow us to perform a partial cystectomy. The patient was young and unmarried and she did not agree to the radical surgery. We are also highlighting the fact that the minimally invasive modality is highly effective and can be adopted in young patients desiring bladder preservation.
Figures and Tables
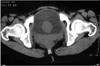 | FIG. 1Contrast computed tomography scan of the pelvis showing the bladder mass near the bladder neck. |
References
1. Dahm P, Gschwend JE. Malignant non-urothelial neoplasms of the urinary bladder: a review. Eur Urol. 2003. 44:672–681.
2. Berkmen F, Celebioglu AS. Adult genitourinary sarcomas: a report of seventeen cases and review of the literature. J Exp Clin Cancer Res. 1997. 16:45–48. +4.
3. Rosser CJ, Slaton JW, Izawa JI, Levy LB, Dinney CP. Clinical presentation and outcome of high-grade urinary bladder leiomyosarcoma in adults. Urology. 2003. 61:1151–1155.
4. Swartz DA, Johnson DE, Ayala AG, Watkins DL. Bladder leiomyosarcoma: a review of 10 cases with 5-year followup. J Urol. 1985. 133:200–202.
5. Ricciardi E, Maniglio P, Schimberni M, Moscarini M. A case of high-grade leiomyosarcoma of the bladder with delayed onset and very poor prognosis. World J Surg Oncol. 2010. 8:16.
6. De Berardinis E, Giulianelli R, Zarrelli G, De Santis C, Ginepri A, Gentile BC, et al. Leiomyosarcoma of urinary bladder: personal experience in 3 cases over a 10-year period. Arch Ital Urol Androl. 1997. 69:Suppl 1. 73–80.
7. Strander H, Turesson I, Cavallin-Stahl E. A systematic overview of radiation therapy effects in soft tissue sarcomas. Acta Oncol. 2003. 42:516–531.
8. Martin SA, Sears DL, Sebo TJ, Lohse CM, Cheville JC. Smooth muscle neoplasms of the urinary bladder: a clinicopathologic comparison of leiomyoma and leiomyosarcoma. Am J Surg Pathol. 2002. 26:292–300.
9. Dotan ZA, Tal R, Golijanin D, Snyder ME, Antonescu C, Brennan MF, et al. Adult genitourinary sarcoma: the 25-year Memorial Sloan-Kettering experience. J Urol. 2006. 176:2033–2038.
10. O'Sullivan B, Ward I, Catton C. Recent advances in radiotherapy for soft-tissue sarcoma. Curr Oncol Rep. 2003. 5:274–281.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download