Abstract
Purpose
Urinary tract infection (UTI) is one of the most prevalent bacterial infections, and fluoroquinolone therapy is a well-known standard regimen for UTI. The prevalence and risk factor analysis of fluoroquinolone resistance in enterococcal UTIs are not well documented. The aim of this study was to evaluate the antimicrobial susceptibility and risk factors for ciprofloxacin resistance in Enterococcus faecalis strains isolated from patients with complicated UTI.
Materials and Methods
We evaluated 81 E. faecalis strains isolated from 81 male patients at a single teaching hospital over 3 years. The Vitek 2 automatic system was used for antimicrobial susceptibility analysis.
Results
Antimicrobial resistance rates were rare for ampicillin/sulbactam, imipenem, and vancomycin in E. faecalis. Forty-six percent of the E. faecalis strains were resistant to levofloxacin, 47% were resistant to ciprofloxacin, and 58% were resistant to norfloxacin. E. faecalis strains were highly resistant to erythromycin (92%) and ftetracycline (96%). The risk factor analysis revealed that age intervals, the underlying diseases, catheterization, and the number of admissions did not increase the risk of ciprofloxacin resistance, whereas patients with hospital-acquired infection (odds ratio [OR], 18.15; 95% confidence interval [CI], 3.46 to 95.13; p=0.001), patients who were treated in a urological department (OR, 6.15; 95% CI, 1.5 to 25.41; p=0.012), and patients who were transferred from health care centers (OR, 7.393; 95% CI, 1.32 to 41.22; p=0.023) had an increased risk of ciprofloxacin resistance compared with the matched controls.
Urinary tract infection (UTI) is one of the most prevalent infections worldwide. Traditionally, UTIs are classified into two groups: uncomplicated UTI and complicated UTI [1,2]. Each type of UTI has different clinical characteristics [1]. It is well known that Escherichia coli strains are the most prevalent pathogens in uncomplicated UTI [2]. Empirical fluoroquinolones have frequently been used to treat uncomplicated UTI, and the prognosis of the therapy is usually good [2]. However, patients diagnosed with a complicated UTI are often elderly, have devices such as urinary catheters, or have neurological or anatomical disorders resulting in voiding problems [1,3,4].
Because females have fewer underlying urinary tract diseases than do males, UTIs in younger females are generally considered to be uncomplicated UTIs [2]. Because old men are more likely to have underlying anatomical abnormalities in their genitourinary system, UTIs in this group are usually considered to be complicated UTIs [5,6]. For this reason, older males with a UTI should undergo urine culture and antimicrobial susceptibility testing.
Although E. coli is the most common pathogen in UTIs, the aforementioned conditions in complicated UTI together with the fact that these patients are often treated with antibiotics will increase the frequency of secondary pathogens such as Enterococcus faecalis [2,7-10]. Furthermore, the prevalence of multiple-drug-resistant enterococci has increased around the world [8,9]. Previous antimicrobial therapy, urological procedures, the use of urinary catheters, a history of recurrent UTI, and hospital stay have theoretically been considered as risk factors for developing enterococcal UTI [8,11,12].
Fluoroquinolones have a broad spectrum for gram-positive and gram-negative bacteria. They are also convenient for oral intake and have few side effects. Owing to these advantages, empirical treatment with fluoroquinolones has been a standard treatment for UTI in Korea [13]. Concurrently and perhaps consequently, UTIs due to fluoroquinolone-resistant bacterial strains have continued to increase at an alarming rate in Korea [10,13]. Furthermore, fluoroquinolones have been inappropriately or empirically used to treat E. faecalis-associated UTIs. For those reasons, the emergence of fluoroquinolone-resistant E. faecalis strains has recently been reported in several countries [9-14]. However, information on fluoroquinolone-resistant E. faecalis strains and risk factor analysis for resistance in complicated UTI isolates is scarce in Korea.
The antimicrobial resistance rate is dependent on various factors such as social and economic factors and the customs for antimicrobial prescription in each country [15-17]. Consequently, antimicrobial resistance rates vary among countries, with high rates in Asia-Pacific regions and low rates in westernized countries [15,16]. In addition, the etiology of UTIs and the antibiotic susceptibility of the causative uropathogens have been changing over the past years [15,16].
Because little is known about UTI with E. faecalis isolates in Korea, we evaluated antimicrobial resistance patterns in E. faecalis isolates and determined the risk factors for ciprofloxacin resistance in E. faecalis strains isolated from Korean men with complicated UTI.
Patients visited this hospital with very heterogeneous diseases. The main causes of patient visits were chronic care after trauma or neurological diseases or their sequelae. Some patients had chronic medical diseases, such as various cancers, diabetes mellitus, chronic renal failure, and malnutrition. The patients usually had multiple combined diseases for several years.
We defined UTI as an infection of the urinary tract with at least 104 colony-forming units of cultured bacteria and at least one UTI symptom, such as fever or urinary frequency, dysuria, or suprapubic tenderness [12,18]. Urine cultures were collected consecutively from patients in whom UTI was suspected at a single university hospital from January 2010 to November 2012. The minimal inhibitory concentration (MIC) ranges of all antimicrobials for E. faecalis strains were categorized according to the Clinical and Laboratory Standards Institute guideline, and the ciprofloxacin susceptibilities were defined as follows: sensitive, MICs of no more than 1 µg/mL; intermediate, MICs of 2 µg/mL; and resistant, MICs of no less than 8 µg/mL [10,12]. Antibiotic susceptibility testing was performed by use of an automated VITEK-2 machine (bioMérieux, Marcy-I'Etoile, France). We excluded all cases of urosepsis by E. faecalis strains, and only one specimen per male patient was included.
We evaluated the association between the ciprofloxacin-resistant E. faecalis strains and the suggested risk factors, such as the presence of underlying diseases (cancer, diabetes mellitus, and chronic renal failure), indwelling urethral catheter, admission history, treatment in a urological department, transfer from a health care center, and the type of infection (community-associated UTI or hospital-acquired UTI). The risk factor of "indwelling catheter" was defined as catheterization at the time of bacterial isolation. Admission history was defined as hospitalization for 1 day or more, and combined urologic diseases was defined as one or more consultations in the urological department to treat UTIs or lower urinary tract symptoms associated with urinary tract diseases. Transfer from a health care center was defined as direct transfer to this hospital from a health care center. Community-associated UTI and hospital-associated UTI were classified by the place of acquisition: hospital-acquired infections, which were detected 48 hours after hospital admission, and community-acquired infections, which were those that did not meet the criteria to be classified as a hospital-acquired infection [19].
During the study period, 81 E. faecalis strains isolated from 81 male patients were included in this study. The mean age of the patients was 69±13 years (range, 30 to 92 years).
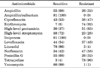
All 81 strains were sensitive to ampicillin/sulbactam and imipenem. Only one strain from the samples revealed resistance to vancomycin. The frequency of quinolone-sensitive E. faecalis was 54% for levofloxacin, 53% for ciprofloxacin, and 42% for norfloxacin, respectively. Sixty-five percent of strains revealed sensitivity to penicillin and penicillin G. Finally, the E. faecalis strains in our study were highly resistant to erythromycin (92%) and tetracycline (96%) (Table 1).
The risk factor analysis for ciprofloxacin-resistant E. faecalis strains is shown in Table 2. The mean ages of the patients with sensitive and resistant strains to ciprofloxacin were 70.88±14.2 and 67.29±13.99 years, respectively (p>0.05). The frequency of ciprofloxacin-resistant strains was significantly higher in patients treated in a urological department (p=0.015). Patients with hospital-associated UTI were significantly more likely to have ciprofloxacin resistance than were those with community-acquired UTI (p=0.000).
In addition, there was a significant correlation between ciprofloxacin resistance and previous admission history (p=0.007). However, we could not find any statistical significance between ciprofloxacin-resistant E. faecalis and the presence of underlying diseases (cancer, diabetes mellitus, or chronic renal failure). Furthermore, an indwelling urethral catheter and transfer from a health care center were not associated with increased ciprofloxacin resistance in this study (Table 2).
We analyzed trends for the risk of ciprofloxacin resistance in E. faecalis by performing multivariate analysis (Table 3). Age intervals, the presence of underlying diseases, catheterization, and the number of admissions did not increase ciprofloxacin resistance. However, hospital-acquired E. faecalis strains were significantly more likely to be ciprofloxacin resistant than were community-acquired E. faecalis strains (odds ratio [OR], 18.15; 95% confidence interval [CI], 3.46 to 95.13; p=0.001). Furthermore, patients treated in a urological department had an increased risk of ciprofloxacin resistance (OR, 6.15; 95% CI, 1.5 to 25.41; p=0.012), and patients transferred from a health care center also had an increased risk of ciprofloxacin resistance (OR, 7.39; 95% CI, 1.32 to 41.22; p=0.023).
It is generally known that E. coli are the most common pathogen in both complicated and uncomplicated UTI [9,10]. However, other bacteria, such as Enterococcus species, Pseudomonas aeruginosa, and Candida species, are more common in complicated UTI than in uncomplicated UTI. Among the Enterococcus species, the E. faecalis strains are found more frequently in urine from patients with complicated UTI than are the E. faecium strains [9,10].
E. faecalis is a gram-positive, commensal bacterium inhabiting the human gastrointestinal tract [20]. Like other commensal species, E. faecalis can cause life-threatening infections in humans in the nosocomial environment, in which naturally high levels of antibiotic resistance are found [20,21]. These bacteria frequently colonize the urinary tract and cause UTI.
The prevalence of enterococcal UTIs has been increasing around the world [22]. However, to our knowledge, very few studies have focused on E. faecalis strains isolated from UTIs, even though these organisms are the second most common cause of both uncomplicated and complicated UTIs [9,10].
The E. faecalis strains in this study were highly sensitive to ampicillin/sulbactam, imipenem, vancomycin, and linezolid. Because of their extremely broad-spectrum activity and collateral damage, their side effects, and concern over the appearance of carbapenem-resistant bacteria, we should reserve these antimicrobials for severe or life-threatening infection. Consequently, we should abide by the policy of formulary restriction and preauthorization strategies to use these antimicrobials.
Ampicillin/sulbactam or amoxicillin/clavulanate is a combination of the common penicillin-derived antibiotics and an inhibitor of bacterial beta-lactamase [23]. Ampicillin/sulbactam is likely to become increasingly important for the treatment of E. faecalis-associated UTIs as long as no emergence of resistance is reported. In addition, we think these antimicrobials can be recommended for treating fluoroquinolone-resistant E. faecalis strains associated from patients with UTI in Korea.
Lee et al. [10] insisted that ampicillin revealed high drug sensitivity for E. faecalis strains from both uncomplicated and complicated UTIs. But only limited E. faecalis strains showed sensitivity to penicillin and penicillin G in this study. Our data are also supported by Sibel et al. [21], who reported that only 45.5% of E. faecalis strains had ampicillin sensitivity. Even though we do not know the exact reason for the discrepancy, some technical problems in data handling may be involved.
The frequency of quinolone-sensitive E. faecalis strains was 54% for levofloxacin, 53% for ciprofloxacin, and 42% for norfloxacin, respectively. The antimicrobial-resistance pattern was similar between levofloxacin and ciprofloxacin in this study; only one ciprofloxacin-resistant E. faecalis strain showed levofloxacin sensitivity (Table 1). Norfloxacin showed the lowest sensitivity among the quinolone family members. This result suggests that fluoroquinolones are not a good initial or an adequate antimicrobial for complicated UTI in men.
Fluoroquinolone-based empirical therapy has been a standard treatment for UTI around the world [13]. Even though we may easily obtain information about antimicrobial resistance patterns from the large amounts of data on fluoroquinolone-resistant E. coli in uncomplicated UTI [10,13,24], information on fluoroquinolone-resistant E. faecalis strains and a risk factor analysis for fluoroquinolone resistance from complicated UTI isolates are scarce in Korea. We can estimate the risk factors for fluoroquinolone-resistant E. faecalis strains from the well-known risk factors for fluoroquinolone-resistant E. coli strains in uncomplicated UTI. Previous antimicrobial therapy, urological procedures, the use of urinary catheters, a history of recurrent UTI, and hospital stay have been considered as risk factors for developing fluoroquinolone-resistant UTI strains [10,25-27].
Because ciprofloxacin is the prototype fluoroquinolone and the antimicrobial resistance pattern between levofloxacin and ciprofloxacin is similar, we analyzed risk factors for ciprofloxacin resistance in E. faecalis strains isolated from men with complicated UTIs.
Age interval, the presence of underlying diseases, cauterization, and the number of admissions did not increase the ciprofloxacin resistance in this study. There are inconsistent data for the association between fluoroquinolone-resistant E. faecalis strains and the number of admissions. Rattanaumpawan et al. [27] reported that a previous hospitalization within 2 weeks is a risk factor for fluoroquinolone resistance, whereas Yasufuku et al. [12] reported that previous hospitalization is not a risk factor. We think that the difference in these studies may result from different patient characteristics. It has been generally accepted that catheterization or keeping a urethral catheter for voiding difficulty may be an important risk factor for fluoroquinolone resistance [25]. We determined that having an indwelling urethral catheter was not an important risk factor for fluoroquinolone resistance. Our result is also supported by other reports [12,28].
Hospital-acquired E. faecalis infection is significantly more likely to have antimicrobial resistance than community-acquired E. faecalis infection [19,29,30]. Hospital-acquired infection is an infection in which the development is favored by a hospital environment. The suggested mechanisms for fluoroquinolone resistance in hospitals may be the patient's poor state of health, the use of invasive devices, and the recent use of fluoroquinolones or other types of antimicrobials [30,31]. Because the presence of underlying diseases and an indwelling catheter were not important risk factors for fluoroquinolone resistance in this study, we think that the recent use of antimicrobials may be an important risk factor for obtaining fluoroquinolone-resistant strains [28].
Previous treatment in a urological department increased the risk of ciprofloxacin resistance. Patients who visited the urological department in this hospital were treated because of benign prostatic hypertrophy, urethral stricture, prostate cancer, neurogenic bladder, and bladder stones. We do not know why the patients showed high rates of fluoroquinolone resistance. Further prospective studies may be required.
The patients transferred from health care centers also had an increased risk of ciprofloxacin resistance. Health care centers are usually health care institutions that engage in providing long-term medical treatment for a wide variety of medical conditions. Patients are admitted to health care centers because of dementia, disability after cerebral vascular accident or traffic accident, and long-standing incurable diseases. The patients in health care centers may have risk factors for acquiring antimicrobial-resistant strains from other patients in the same health care center or from inappropriate handling by medical staff or assistants [28,30]. Owing to a lack of surveillance data, little is known about the resistance rates in health care centers in Korea. In the future, whenever patient care is provided in health care centers, adherence to infection prevention guidelines is needed.
This study had some limitations. At first, we defined UTI by E. faecalis as an infection with at least 104 colony-forming units of cultured bacteria and at least one UTI symptom, such as fever or urinary frequency, dysuria, or suprapubic tenderness. It was very difficult to differentiate the symptoms of benign prostatic hypertrophy or overactive bladder from those of true UTI [18]. Because many patients with an indwelling urethral catheter complained of suprapubic tenderness or lower abdominal pain, the rate of true UTI by E. faecalis strains can be overestimated. In addition, because some chronically ill patients cannot exactly express their UTI symptoms, the rate of true UTI by E. faecalis strains can be underestimated. For those reasons, a well-designed prospective study is needed in the future. Another limitation is that we did not evaluate previous antimicrobial use in the patients studied. It is generally accepted that previous use of fluoroquinolones or other antibiotics is significantly related to fluoroquinolone resistance [12,13,26,28]. Whereas we could retrieve the history of previous antimicrobial prescriptions in the same hospital, we could not get accurate prescription data from other hospitals or general doctors or health care centers.
We found a high rate of fluoroquinolone-resistant E. faecalis in urine from men with complicated UTI. We should characterize the bacterial strains isolated from men with UTIs. In the case of UTI from E. faecalis strains, fluoroquinolone is no longer recommended in Korea.
In addition, hospital-acquired UTI, previous treatment in a urological department, and transfer from a health care center are important risk factors for fluoroquinolone-resistant E. faecalis. We should carefully evaluate the patients with these risk factors for fluoroquinolone-resistant E. faecalis strains and treat them with appropriate antimicrobials such as ampicillin/sulbactam or amoxicillin/clavulanate.
Figures and Tables
TABLE 1
Antimicrobial sensitivity of Enterococcus faecalis strains isolated from male patients with urinary tract infections
References
1. Johansen TE, Botto H, Cek M, Grabe M, Tenke P, Wagenlehner FM, et al. Critical review of current definitions of urinary tract infections and proposal of an EAU/ESIU classification system. Int J Antimicrob Agents. 2011. 38:Suppl. 64–70.
2. Wagenlehner FM, Weidner W, Naber KG. An update on uncomplicated urinary tract infections in women. Curr Opin Urol. 2009. 19:368–374.
3. Hsueh PR, Hoban DJ, Carmeli Y, Chen SY, Desikan S, Alejandria M, et al. Consensus review of the epidemiology and appropriate antimicrobial therapy of complicated urinary tract infections in Asia-Pacific region. J Infect. 2011. 63:114–123.
4. Neal DE Jr. Complicated urinary tract infections. Urol Clin North Am. 2008. 35:13–22. v
5. Drekonja DM, Rector TS, Cutting A, Johnson JR. Urinary tract infection in male veterans: treatment patterns and outcomes. JAMA Intern Med. 2013. 173:62–68.
6. Orenstein R, Wong ES. Urinary tract infections in adults. Am Fam Physician. 1999. 59:1225–1234. 1237
7. Stamm WE, Hooton TM. Management of urinary tract infections in adults. N Engl J Med. 1993. 329:1328–1334.
8. Sood S, Malhotra M, Das BK, Kapil A. Enterococcal infections & antimicrobial resistance. Indian J Med Res. 2008. 128:111–121.
9. Matsumoto T, Hamasuna R, Ishikawa K, Takahashi S, Yasuda M, Hayami H, et al. Nationwide survey of antibacterial activity against clinical isolates from urinary tract infections in Japan (2008). Int J Antimicrob Agents. 2011. 37:210–218.
10. Lee SJ, Lee DS, Choe HS, Shim BS, Kim CS, Kim ME, et al. Antimicrobial resistance in community-acquired urinary tract infections: results from the Korean Antimicrobial Resistance Monitoring System. J Infect Chemother. 2011. 17:440–446.
11. Huycke MM, Sahm DF, Gilmore MS. Multiple-drug resistant enterococci: the nature of the problem and an agenda for the future. Emerg Infect Dis. 1998. 4:239–249.
12. Yasufuku T, Shigemura K, Shirakawa T, Matsumoto M, Nakano Y, Tanaka K, et al. Mechanisms of and risk factors for fluoroquinolone resistance in clinical Enterococcus faecalis isolates from patients with urinary tract infections. J Clin Microbiol. 2011. 49:3912–3916.
13. Lee G, Cho YH, Shim BS, Lee SD. Risk factors for antimicrobial resistance among the Escherichia coli strains isolated from Korean patients with acute uncomplicated cystitis: a prospective and nationwide study. J Korean Med Sci. 2010. 25:1205–1209.
14. Ishikawa K, Matsumoto T, Yasuda M, Uehara S, Muratani T, Yagisawa M, et al. The nationwide study of bacterial pathogens associated with urinary tract infections conducted by the Japanese Society of Chemotherapy. J Infect Chemother. 2011. 17:126–138.
15. Goossens H, Ferech M, Vander Stichele R, Elseviers M. ESAC Project Group. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet. 2005. 365:579–587.
16. Hoban DJ, Lascols C, Nicolle LE, Badal R, Bouchillon S, Hackel M, et al. Antimicrobial susceptibility of Enterobacteriaceae, including molecular characterization of extended-spectrum beta-lactamase-producing species, in urinary tract isolates from hospitalized patients in North America and Europe: results from the SMART study 2009-2010. Diagn Microbiol Infect Dis. 2012. 74:62–67.
17. Huang CC, Chen YS, Toh HS, Lee YL, Liu YM, Ho CM, et al. Impact of revised CLSI breakpoints for susceptibility to third-generation cephalosporins and carbapenems among Enterobacteriaceae isolates in the Asia-Pacific region: results from the Study for Monitoring Antimicrobial Resistance Trends (SMART), 2002-2010. Int J Antimicrob Agents. 2012. 40:Suppl. S4–S10.
18. Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008. 36:309–332.
19. Peleg AY, Hooper DC. Hospital-acquired infections due to gram-negative bacteria. N Engl J Med. 2010. 362:1804–1813.
20. Sava IG, Heikens E, Huebner J. Pathogenesis and immunity in enterococcal infections. Clin Microbiol Infect. 2010. 16:533–540.
21. Sibel AK, Koroglu M, Muharrem AK. The evaluation of antimicrobial susceptibility of urine enterococci with the Vitek 2 automated system in eastern Turkey. Southeast Asian J Trop Med Public Health. 2012. 43:986–991.
22. Morrison AJ Jr, Wenzel RP. Nosocomial urinary tract infections due to enterococcus. Ten year's experience at a university hospital. Arch Intern Med. 1986. 146:1549–1551.
23. Adam D. Beta-lactam/beta-lactamase inhibitor combinations in empiric management of pediatric infections. J Int Med Res. 2002. 30:Suppl 1. 10A–19A.
24. Lautenbach E, Metlay JP, Mao X, Han X, Fishman NO, Bilker WB, et al. The prevalence of fluoroquinolone resistance mechanisms in colonizing Escherichia coli isolates recovered from hospitalized patients. Clin Infect Dis. 2010. 51:280–285.
25. Smithson A, Chico C, Ramos J, Netto C, Sanchez M, Ruiz J, et al. Prevalence and risk factors for quinolone resistance among Escherichia coli strains isolated from males with community febrile urinary tract infection. Eur J Clin Microbiol Infect Dis. 2012. 31:423–430.
26. van der Starre WE, van Nieuwkoop C, Paltansing S, van't Wout JW, Groeneveld GH, Becker MJ, et al. Risk factors for fluoroquinolone-resistant Escherichia coli in adults with community-onset febrile urinary tract infection. J Antimicrob Chemother. 2011. 66:650–656.
27. Rattanaumpawan P, Tolomeo P, Bilker WB, Fishman NO, Lautenbach E. Risk factors for fluoroquinolone resistance in Enterococcus urinary tract infections in hospitalized patients. Epidemiol Infect. 2011. 139:955–961.
28. Roghmann MC, Wallin MT, Gorman PH, Johnson JA. Prevalence and natural history of colonization with fluoroquinolone-resistant gram-negative bacilli in community-dwelling people with spinal cord dysfunction. Arch Phys Med Rehabil. 2006. 87:1305–1309.
29. Klare I, Konstabel C, Mueller-Bertling S, Werner G, Strommenger B, Kettlitz C, et al. Spread of ampicillin/vancomycin-resistant Enterococcus faecium of the epidemic-virulent clonal complex-17 carrying the genes esp and hyl in German hospitals. Eur J Clin Microbiol Infect Dis. 2005. 24:815–825.
30. Klare I, Konstabel C, Badstubner D, Werner G, Witte W. Occurrence and spread of antibiotic resistances in Enterococcus faecium. Int J Food Microbiol. 2003. 88:269–290.
31. Puhto T, Ylipalosaari P, Ohtonen P, Syrjala H. Point prevalence and risk factors for healthcare-associated infections in primary healthcare wards. Infection. 2011. 39:217–223.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download