Abstract
Purpose
The aim of this study was to evaluate the effectiveness of simultaneous flexible ureteroscopic removal of stones (URS) for ureteral and ipsilateral renal stones and to analyze the predictive factors for renal stone-free status.
Materials and Methods
We retrospectively reviewed the records of patients who underwent simultaneous flexible URS of ureteral and ipsilateral renal stones from January 2010 to May 2012. All operations used a flexible ureteroscope. We identified 74 cases of retrograde intrarenal surgery and 74 ureteral stones (74 patients). Stone-free status was respectively defined as no visible stones and clinically insignificant residual stones <3 mm on a postoperative image study. Predictive factors for stone-free status were evaluated.
Results
The immediate postoperative renal stone-free rate was 70%, which increased to 83% at 1 month after surgery. The immediate postoperative ureteral stone-free rate was 100%. Among all renal stones, 15 (20.3%) were separately located in the renal pelvis, 11 (14.8%) in the upper calyx, 15 (20.3%) in the mid calyx, and 33 (44.6%) in the lower calyx. The mean cumulative stone burden was 92.22±105.75 mm2. In a multivariate analysis, cumulative stone burden <100 mm2 was a significant predictive factor for postoperative renal stone-free status after 1 month (p<0.01).
Go to : 
Ureteroscopy has been established as a minimally invasive modality for treating ureteral calculi, and ureteroscopic removal of stones (URS) results in a better chance for stone clearance with a single procedure, even for proximal ureteral stones sized >10 mm [1]. Moreover, advances in distal-tip deflection, improved scope durability, decreases in scope diameter, improved light diffusion, and extended field of vision and the advent of the holmium:yttrium-aluminium-garnet (YAG) laser have expanded the role of flexible ureteroscopy from a diagnostic to a therapeutic procedure similar to retrograde intrarenal surgery (RIRS). Flexible URS has become a safer and more established modality for treating any type of urinary stone, and its indications have been extended [2-4].
Multiple stones are found in 20% to 25% of patients with urolithiasis. In cases with multiple stones, 29% to 36% of patients have ureteral stones with renal stones simultaneously [5-8]. On the basis of a 40% to 50% stone-free rate (SFR) for extracorporeal shock wave lithotripsy (ESWL) in patients with multiple stones [6], questions are being raised about the effectiveness of ESWL for these patients. More advantages can be realized compared with ESWL if ureteral and renal stones can be managed simultaneously with advance ureteroscopic techniques including RIRS, although it may be a more invasive procedure. No study has investigated simultaneous treatment for ureteral and renal stones, and no established guidelines are available for treating ureteral and coexistent renal stones [1].
Our hypothesis was that the more advanced flexible URS would be a successful treatment option for selected patients with ureteral and renal stones. To test this hypothesis, we investigated the effectiveness of flexible URS for treating ureteral and ipsilateral renal stones by evaluating SFRs and associated complications. We further analyzed the predictive factors for renal stone-free status in our cases.
Go to : 
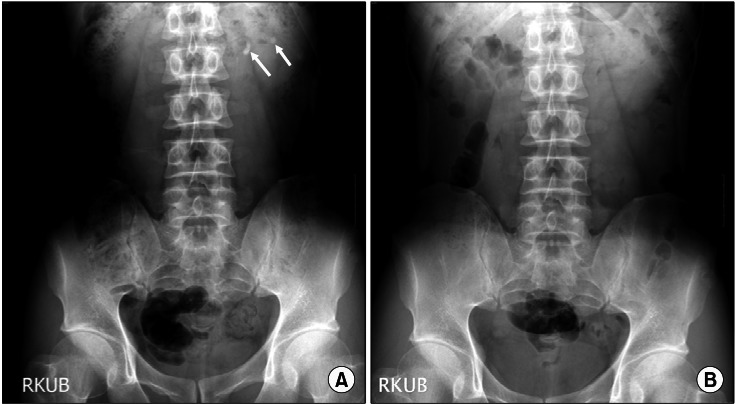
We performed a retrospective analysis of 74 patients who underwent flexible URS with RIRS for simultaneous treatment of ureteral calculi and ipsilateral renal stones from January 2010 to May 2012 (Fig. 1). All patients were examined by kidney-ureter-bladder abdominal radiography and abdominal computed tomography (CT). Patients with calyceal diverticular stones, a ureteral stricture, or medullary sponge kidneys were excluded from the analysis. Each patient was evaluated for stone number, stone size, stone location, laterality, operative time, SFR, and perioperative complications. Renal stone size was determined by calculating cumulative stone burden. Renal stone burden was defined as the two-dimensional area determined by multiplying the longest diameter by the perpendicular diameter of the stone [9]. In cases of multiple stones, the total stone burden (cumulative stone burden) was calculated as the sum of the burden of each stone. Renal stones with irregular shapes such as staghorn stones were divided into several subunits, and the burdens of each of the units were summed [8]. Stone locations were subdivided into four groups, including the upper calyx, mid calyx, lower calyx, and renal pelvis.
All surgeries were performed by one surgeon using a 7.5-Fr (Karl Storz, Tuttlingen, Germany) or an 8.4-Fr (Olympus America Inc., Center Valley, PA, USA) flexible ureteroscope. Patients were placed in the lithotomy position under general anesthesia. Cystoscopy was performed routinely before flexible ureteroscopy in all patients to place a hydrophilic guidewire into the renal pelvis. Retrograde pyelography by contrast-dye fluoroscopy was performed to identify urinary stones and the urinary tract. After the passage of a safety guidewire into the renal pelvis, a ureteral access sheath (9.5/11.5 or 12/14 Fr; Forté Ureteral Access Sheaths, Applied Medical Resources, Rancho Santa Margarita, CA, USA) was placed to facilitate extraction of stone fragments according to the location of the ureteral stone. Ureteral stones were fragmented with a holmium:YAG laser with a 365-µm fiber. Renal stone fragments were subjected to 200- or 365-µm fibers. Laser energy and pulse frequency were varied on the basis of stone volume. The settings were decreased once the residual mass became mobile to minimize kinetic forces and emphasize mechanical fragmentation. Fragmented stones were extracted by using a stone basket.
The entire collecting system was inspected by means of flexible URS to evaluate stone clearance, and a fluoroscopic examination with or without contrast dye was performed to identify the presence of radio-opaque lesions or filling defects at the end of the procedure. All patients were treated conservatively with antibiotics or prolonged placement of a 6.0-Fr double-J stent (Endo-Sof Double Pigtail Ureteral Stent; Cook Medical, Bloomington, IN, USA) in the ureter. After inserting the double-J stent, we pulled out the string through the urethra from the urinary bladder pigtail side and fixed it on the perineal area. We removed the stent from the patient after 1 week by pulling out the stent string. Postoperative follow-up radiographic studies including plain X-rays or nonenhanced CT scans were obtained at 1 day and 1 month after surgery. We evaluated the immediate and postoperative 1 month SFR, and we compared the SFR between immediately after the procedure and 1 month postoperatively according to location, size, and number by use of paired t-tests. Stone-free status was respectively defined as no visible stones and clinically insignificant residual stones <3 mm on a postoperative imaging study. We also investigated the complication rate of surgery and the axillary procedure.
We analyzed predictive factors for renal SFR. In the univariate analysis, the statistical significance of indications for surgery and variables associated with stone characteristics (sex, age, laterality, and number, etc.) in relation to the immediate and 1-month postoperative SFRs were evaluated by using the chi-square test. Multivariate analysis with logistic regression was performed to identify the combined influence of these variables. Data were analyzed by using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA). A p<0.05 was considered statistically significant.
Go to : 
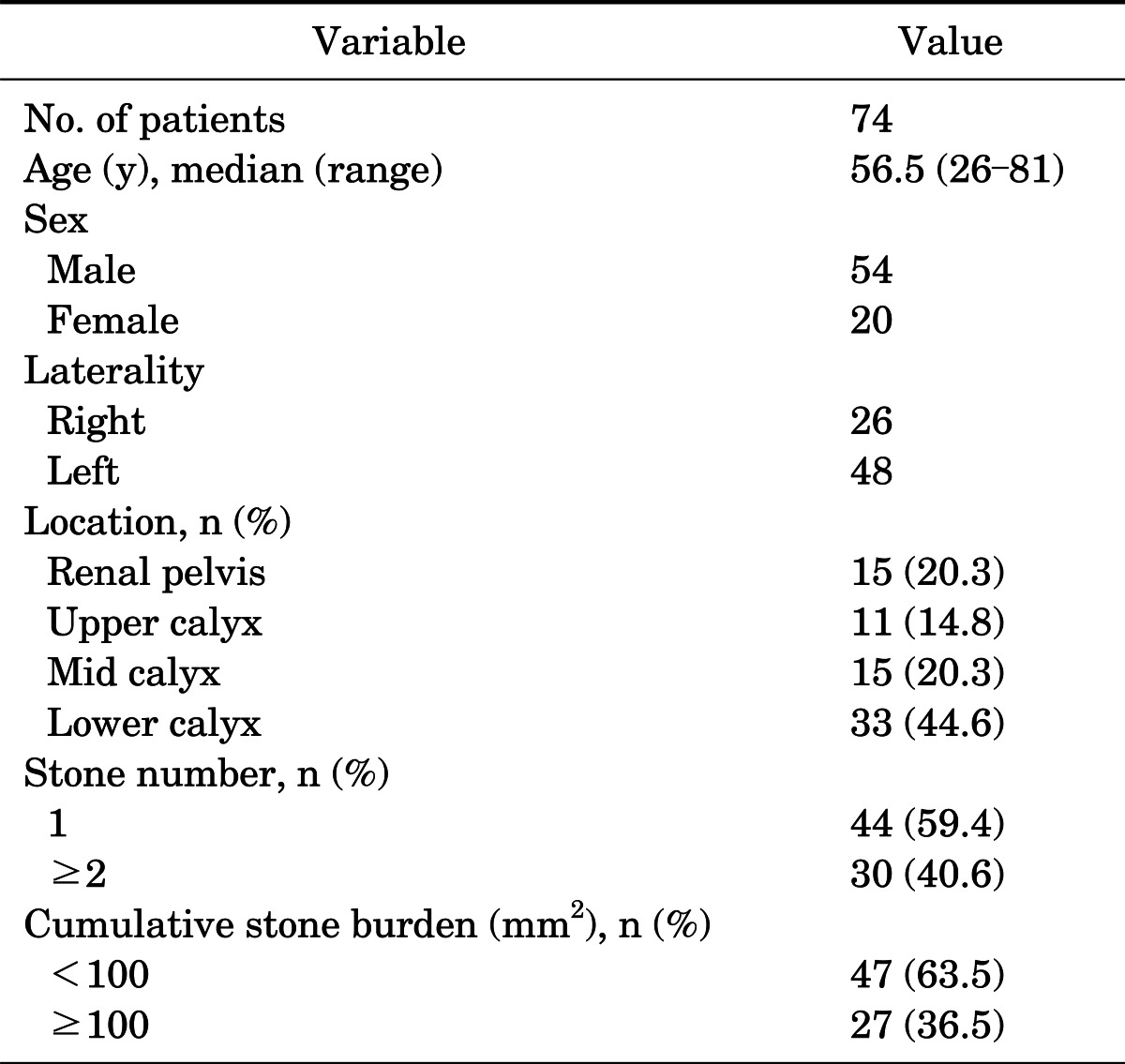
Seventy-four cases of flexible URS with RIRS divided by stone location were identified in this retrospective analysis. Table 1 lists the patient demographics and the baseline characteristics of the renal stones. We included 54 men and 20 women (mean age, 56.5 years; range, 26 to 81 years). The 74 ureteral stones included 46 upper ureteral stones (62.2%), 10 mid ureteral stones (13.5%), and 18 lower ureteral stones (24.3%). Forty-four patients (59.4%) had a single renal stone, and 30 (40.6%) had two or more renal stones. In our study, multiple stones were in same location. Among all renal stones, 15 (20.3%) were separately located in the renal pelvis, 11 (14.8%) in the upper calyx, 15 (20.3%) in the mid calyx, and 33 (44.6%) in the lower calyx. The mean cumulative stone burden was 92.22±105.75 mm2, with 47 cases (63.5%) with a cumulative burden of <100 mm2, 17 cases (23.0%) with a cumulative burden of ≥100 and <200 mm2, and 10 cases (13.5%) with a cumulative burden of ≥200 mm2. The median operation time (calculated from the time of cystoscope insertion to completion of stent placement) was 106 minutes (range, 60 to 200 minutes). The overall immediate postoperative renal SFR was 70%, which increased to 83.8% at 1 month after surgery. The postoperative ureteral SFR was 100% in all cases.
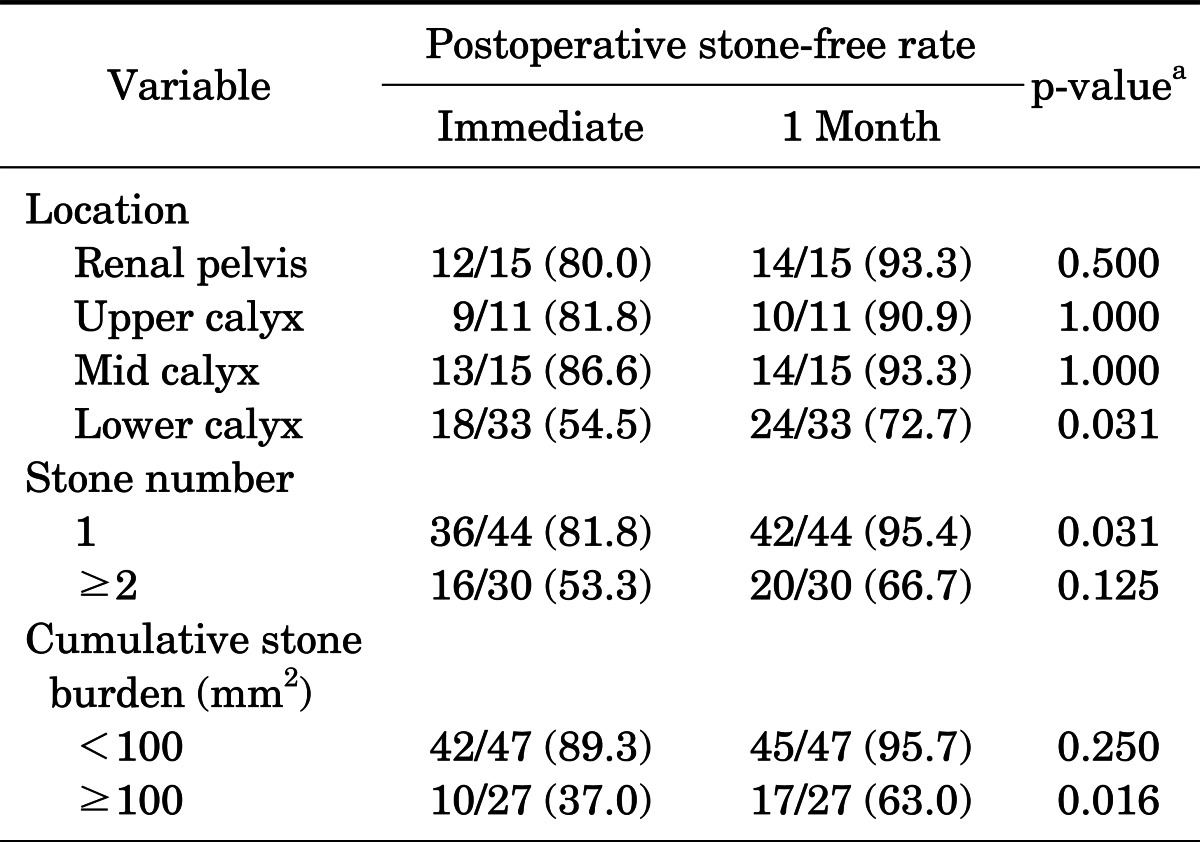
Renal SFRs according to the variables analyzed are listed in Table 2. SFRs in all groups increased after 1 month compared with the immediate SFRs. When renal stone locations were subdivided into the renal pelvis, upper calyx, mid calyx, and lower calyx, the immediate SFRs of each group were 80.0%, 81.8%, 86.8%, and 54.5%, respectively. After 1 month, the SFRs in each group were 93.3%, 90.9%, 93.3%, and 72.7%, respectively. The SFR of the lower calyceal location increased significantly after 1 month (p=0.031) but the differences in the SFRs of the other locations were not significant. The SFRs of all groups increased after 1 month for stone numbers of 1 and ≥2 (p=0.031 and p=0.125, respectively). We divided cumulative stone burden (mm2) into groups of <100 and ≥100 to compare the immediate and 1-month SFRs. The SFR of the ≥100 group increased from 37.0% to 63.0% after 1 month (p=0.016), whereas the SFR of the <100 group increased from 89.3% to 95.7% after 1 month without statistical significance.
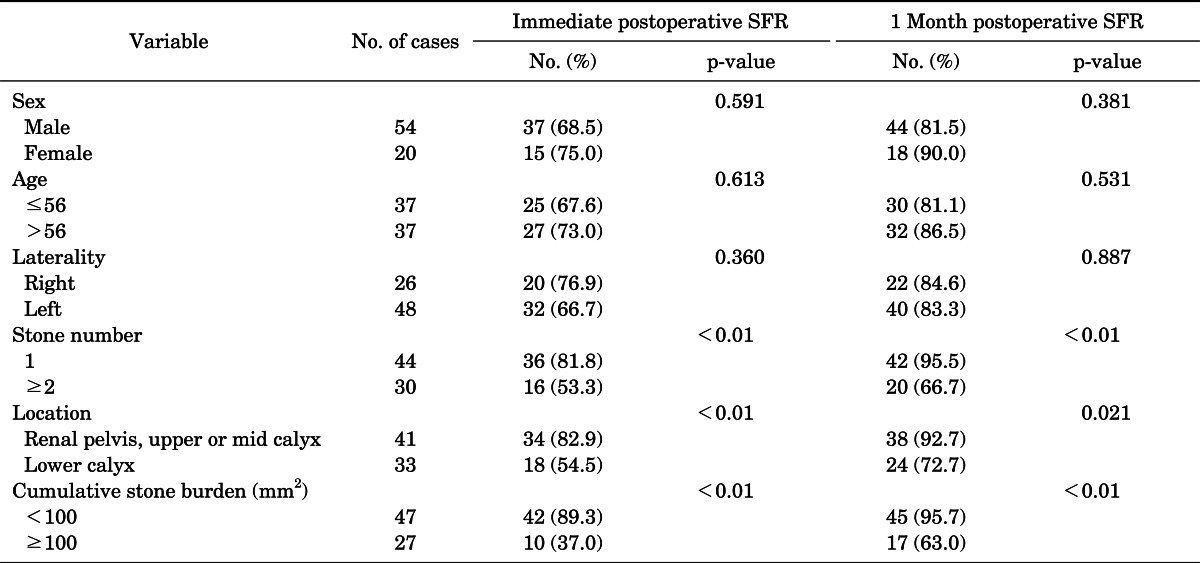
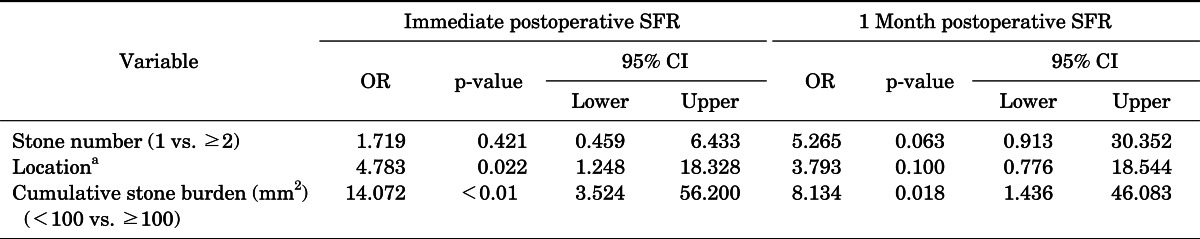
The univariate analysis of postoperative SFRs on the basis of the variables analyzed is shown in Table 3. The SFR according to cumulative stone burden was 89.3% in the <100 mm2 group when compared with the corresponding decrease (37.0%) in the ≥100 mm2 group (p<0.01). The SFR was significantly lower for stones located in the lower calyx than for stones located elsewhere (54.5% vs. 82.9%, respectively, p<0.01). The significant variables identified in the univariate analysis (the factors for which both the immediate and the 1-month SFR were p<0.05) were included in the multivariate analysis. In the multivariate analysis, stone location in the renal pelvis, upper calyx, or mid calyx (odds ratio [OR], 4.783; p=0.022) and cumulative stone burden <100 mm2 (OR, 14.072; p<0.01) were significant predictive factors for immediate renal SFR, whereas stone location in the renal pelvis, upper calyx, or mid calyx after 1 month was not significant (p=0.100) (Table 4).
No major intraoperative complications including ureteral perforation were identified. Three minor complications (5.2%) occurred, including two cases (3.4%) of febrile urinary tract infection and one case (1.7%) of postoperative paralytic ileus. These patients were successfully treated conservatively. None of the patients had a transfusion or subcapsular hematoma. We performed no additional procedures for double-J stent removal because the double-J stent string was removed easily. This did not require a cystoscopic procedure. After 1 month, 12 cases had residual renal stones. Two patients who had stones larger than 4 mm decided to undergo additional ESWL and the stones were completely destroyed. The other cases were concluded under close observation.
Go to : 
Since its appearance at the beginning of the 1980s [10], ESWL has been the least invasive and the most widely used treatment for renal and ureteral stones, even for acute conditions [11]. The possible advantages of ESWL for managing urinary stones are patient acceptance, short convalescence, and the lack of an anesthesia requirement during the procedure. Flexible ureteroscopes and their working devices have rapidly improved over the past several years. URS has equivalent or superior results to SWL for renal and ureteral stones [12]. The advantage of a flexible ureteroscope is that it can reach all parts of the urinary tract including the kidney. Our study evaluated the efficacy of a flexible ureteroscope for treating urinary stones.
We found that the SFRs of lower calyx stones and of large stones increased significantly after 1 month compared with the immediate SFR. This finding indicates that stone fragments were passed during the month, particularly from the lower calyx, as a result of anatomical specificity, and that the large stones were passed as a result of the small fragments produced by the holmium:YAG laser. Small stone fragments that could not be captured by a stone basket were left and took time to spontaneously pass; thus, we believe that the exact SFR may be 1 month after surgery, particularly for lower calyx and large stones.
The overall ureteral SFR with the use of flexible URS was 100% in our study. Although there were insufficient data to compare flexible and rigid URS for proximal ureteral stones statistically, favorable SFRs have been reported using flexible URS (87%) compared with rigid or semirigid URS (77%) [13]. Cohen et al. [14] reported a 97% (31/32) SFR for flexible URS of proximal ureteral stones. Our study supports that the use of flexible URS for ureteral stones is a reliable treatment choice. The overall renal SFR after 1 month was 83.8%, which was similar to that of previous RIRS studies [15,16]. We conducted URS with RIRS; thus, ureteral stone treatment did not affect the renal SFR. Lim at el. [8] reported no significant correlation between the renal SFR and the presence of combined ureteral stones. However, the average operation time in the present study was 106 minutes, which is longer than in previously published RIRS series [4,17,18]. We hypothesize that this was because of the time taken for ureteral stone and renal treatment and that these operative times may be more acceptable compared with repeat ESWL.
Similar to other studies, we observed that larger stone size was associated with a lower SFR (SFR of ≥100 was 63.0%, or 17/27, after 1 month) [8,19]. This is a major disadvantage of RIRS in that multiple procedures may be required to clear a large stone. Takazawa et al. [20] reported successful outcomes from RIRS for renal stones ≥2 cm, including SFRs for preoperative stone sizes of 2 to ≤4 cm and >4 cm of 100% (14/14) and 67% (4/6), respectively. We believe that the SFR will probably continue to improve as the distribution of and further technical improvements in flexible URS continue.
In our study, regardless of the size and location of ureteral stones, the immediate SFR of ureteral stones was 100%. Therefore, we evaluated the size of renal stones, excluding ureteral stones. We analyzed the predictive factors for renal stone-free status in our cases. Larger stones ≥100 mm2 were an independent predictive factor of the SFR both immediately after and at 1 month after surgery. Resorlu et al. [19] published a scoring system predicting the SFR after RIRS. They reported that larger stones are a significant predictive factor of the SFR in RIRS. Additionally, Ito et al. [21] reported that in a univariate analysis, larger stones were a predictive factor of the SFR in RIRS. We think that this may have originated from technical difficulties with larger stones and the prolonged time to treat small stones. However, many studies have reported that larger stones can be removed by RIRS with more advanced techniques and instruments, and our SFR has been increasing according to increased surgical skill (data not shown) [14,20]. Therefore, if we evaluate predictive factors after we gain a larger surgical volume, we believe that we will overcome the difficulties with these larger stones.
The number of renal stones (single vs. multiple) in our series was significant in the univariate analysis but was not a predictor of the SFR in the multivariate logistic regression analysis. Resorlu et al. [19] reported that stone number is a significant predictive factor of the SFR in RIRS. Additionally, Ito et al. [21] also reported that stone number is a predictive factor of the SFR in RIRS in a univariate analysis. However, their multivariate logistic regression analysis was not significant. We think that the reason we did not find significance in the multivariate analysis was a result of the technical advantage of flexible URS, and further evaluation with a larger number of patients is needed. Furthermore, stone location in the lower calyx was significant for immediate SFR in the multivariate logistic regression analysis but was not significant after 1 month. We suggest that stone location in the lower calyx is not a predictive factor when SFR is evaluated 1 month after the operation. Stone location in the lower calyx was a significant predictive factor of the SFR in other studies [8,22]. It is believed that lower calyx stones are more difficult to treat than are stones located in other kidney regions because of technical difficulties in accessing them. We excluded patients with anatomical abnormalities. We suggest that this difference was mainly attributable to two causes. First, there have been improvements in the flexible ureteroscope, its working devices, and surgeon operation skill. Second, stones may need time to pass from the urinary tract. Therefore, we believe that stone location is not a predictive factor for URS with RIRS.
No increased complication rate was observed in the present study, although ureteral and renal stones were operated on simultaneously. Only three minor complications occurred (5.2%). Other studies reported complication rates of 4.6% to 7.7% following RIRS including multiple stones [15,16,23]. The present results further reinforce that simultaneous URS is a favorable option for multiple stones at experienced institutions. We removed the double-J stent by using the string pulling method as described in the Methods in all of our cases. This procedure is less painful than removal through a cystoscope and eliminates the adverse effects of a cystoscopic procedure.
Under the current health insurance system in Korea, the payment for simultaneous endoscopic treatment for ureteral and ipsilateral renal stones has advantages, because major and minor surgeries are considered. In these cases, renal stone treatments are minor surgery, and payment for operating on these stones is reduced by half. In this respect, if patients choose surgical interventions in our specific cases, they will benefit from cost-effectiveness.
Several limitations should be discussed. Our results are based on a relatively small sample size and this was a retrospective review. Because of the retrospective design, confounding factors and measurement bias cannot be reduced as much as they could be in a prospective, randomized study. Another limitation of this study was the involvement of only a single medical center. Additional studies from multiple centers are thus warranted.
Go to : 
References
1. Turk C, Knoll T, Petrik A, Sarica K, Straub M, Seitz C. Guidelines on urolithiasis. 2012 update [Internet]. Arnhem: European Association of Urology;cited 2013 Jan 10. Available from: http://www.uroweb.org/gls/pdf/20_Urolithiasis_LR%20March%2013%202012.pdf.
2. Prabhakar M. Retrograde ureteroscopic intrarenal surgery for large (1.6-3.5 cm) upper ureteric/renal calculus. Indian J Urol. 2010; 26:46–49. PMID: 20535284.

3. Bozkurt OF, Resorlu B, Yildiz Y, Can CE, Unsal A. Retrograde intrarenal surgery versus percutaneous nephrolithotomy in the management of lower-pole renal stones with a diameter of 15 to 20 mm. J Endourol. 2011; 25:1131–1135. PMID: 21657824.
4. Breda A, Ogunyemi O, Leppert JT, Lam JS, Schulam PG. Flexible ureteroscopy and laser lithotripsy for single intrarenal stones 2 cm or greater-is this the new frontier? J Urol. 2008; 179:981–984. PMID: 18207179.

5. Kanao K, Nakashima J, Nakagawa K, Asakura H, Miyajima A, Oya M, et al. Preoperative nomograms for predicting stone-free rate after extracorporeal shock wave lithotripsy. J Urol. 2006; 176(4 Pt 1):1453–1456. PMID: 16952658.

6. Abe T, Akakura K, Kawaguchi M, Ueda T, Ichikawa T, Ito H, et al. Outcomes of shockwave lithotripsy for upper urinary-tract stones: a large-scale study at a single institution. J Endourol. 2005; 19:768–773. PMID: 16190825.

7. Abdel-Khalek M, Sheir KZ, Mokhtar AA, Eraky I, Kenawy M, Bazeed M. Prediction of success rate after extracorporeal shock-wave lithotripsy of renal stones: a multivariate analysis model. Scand J Urol Nephrol. 2004; 38:161–167. PMID: 15204407.
8. Lim SH, Jeong BC, Seo SI, Jeon SS, Han DH. Treatment outcomes of retrograde intrarenal surgery for renal stones and predictive factors of stone-free. Korean J Urol. 2010; 51:777–782. PMID: 21165199.

9. Sung YM, Choo SW, Jeon SS, Shin SW, Park KB, Do YS. The "mini-perc" technique of percutaneous nephrolithotomy with a 14-Fr peel-away sheath: 3-year results in 72 patients. Korean J Radiol. 2006; 7:50–56. PMID: 16549956.

10. Chaussy C, Schuller J, Schmiedt E, Brandl H, Jocham D, Liedl B. Extracorporeal shock-wave lithotripsy (ESWL) for treatment of urolithiasis. Urology. 1984; 23(5 Spec No):59–66. PMID: 6719681.

11. Ghalayini IF, Al-Ghazo MA, Khader YS. Evaluation of emergency extracorporeal shock wave lithotripsy for obstructing ureteral stones. Int Braz J Urol. 2008; 34:433–440. PMID: 18778494.

12. Galvin DJ, Pearle MS. The contemporary management of renal and ureteric calculi. BJU Int. 2006; 98:1283–1288. PMID: 17125486.

13. Preminger GM, Tiselius HG, Assimos DG, Alken P, Buck AC, Gallucci M, et al. 2007 Guideline for the management of ureteral calculi. Eur Urol. 2007; 52:1610–1631. PMID: 18074433.

14. Cohen J, Cohen S, Grasso M. Ureteropyeloscopic treatment of large, complex intrarenal and proximal ureteral calculi. BJU Int. 2013; 111(3 Pt B):E127–E131. PMID: 22757752.

15. Takazawa R, Kitayama S, Tsujii T. Single-session ureteroscopy with holmium laser lithotripsy for multiple stones. Int J Urol. 2012; 19:1118–1121. PMID: 22853010.

16. Breda A, Ogunyemi O, Leppert JT, Schulam PG. Flexible ureteroscopy and laser lithotripsy for multiple unilateral intrarenal stones. Eur Urol. 2009; 55:1190–1196. PMID: 18571315.

17. Akman T, Binbay M, Ozgor F, Ugurlu M, Tekinarslan E, Kezer C, et al. Comparison of percutaneous nephrolithotomy and retrograde flexible nephrolithotripsy for the management of 2-4 cm stones: a matched-pair analysis. BJU Int. 2012; 109:1384–1389. PMID: 22093679.
18. El-Anany FG, Hammouda HM, Maghraby HA, Elakkad MA. Retrograde ureteropyeloscopic holmium laser lithotripsy for large renal calculi. BJU Int. 2001; 88:850–853. PMID: 11851601.

19. Resorlu B, Unsal A, Gulec H, Oztuna D. A new scoring system for predicting stone-free rate after retrograde intrarenal surgery: the "resorlu-unsal stone score". Urology. 2012; 80:512–518. PMID: 22840867.

20. Takazawa R, Kitayama S, Tsujii T. Successful outcome of flexible ureteroscopy with holmium laser lithotripsy for renal stones 2 cm or greater. Int J Urol. 2012; 19:264–267. PMID: 22145599.
21. Ito H, Kawahara T, Terao H, Ogawa T, Yao M, Kubota Y, et al. The most reliable preoperative assessment of renal stone burden as a predictor of stone-free status after flexible ureteroscopy with holmium laser lithotripsy: a single-center experience. Urology. 2012; 80:524–528. PMID: 22658621.

22. Stav K, Cooper A, Zisman A, Leibovici D, Lindner A, Siegel YI. Retrograde intrarenal lithotripsy outcome after failure of shock wave lithotripsy. J Urol. 2003; 170(6 Pt 1):2198–2201. PMID: 14634378.

23. Buob D, Hazan M, Homs S, Matignon M, Mansour H, Audard V, et al. Intrarenal IFN-γ mRNA expression differentiates clinical and subclinical glomerulitis in renal transplant recipients. Transplantation. 2011; 92:170–175. PMID: 21546865.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download