This article has been corrected. See "Corrigendum: Acknowledgments. Effect of Photoselective Vaporization Prostatectomy on Lower Urinary Tract Symptoms in Benign Prostatic Hyperplasia With or Without Intravesical Prostatic Protrusion" in Volume 54 on page 415.
Abstract
Purpose
Intravesical protrusion of the prostate (IPP) can affect voiding. We evaluated the improvement in lower urinary tract symptoms and patient satisfaction after laser prostate photovaporization in benign prostatic hyperplasia (BPH) patients with or without IPP.
Materials and Methods
This prospective study included 134 patients who underwent GreenLight HPS laser photoselective vaporization prostatectomy (PVP) between January 2010 and July 2011 patient. Preoperative IPP was evaluated by using the retroflexed view from flexible cystoscopy. evaluation included complete medical history, International Prostate Symptom Scores (IPSS), maximum flow rate (Qmax), postvoid residual (PVR), serum prostate-specific antigen (PSA), and transrectal ultrasonogram. Changes from baseline in Qmax, PVR, total IPSS, and IPSS subscores (voiding and storage) were analyzed at postoperative months 1, 3, and 6.
Results
The patients' mean age was 66.6±7.8 years. Mean serum PSA and prostate volume were 1.7±1.5 ng/mL and 42.9±16.7 g, respectively. No significant differences existed between the IPP and no IPP groups in preoperative prostate volume, total IPSS, PSA, or lasing time and energy. The mean follow-up duration was 6.2±1.9 months. IPP patients showed significant improvements in total IPSS and voiding subscores at months 1 and 3. Improvements in the quality of life score and storage subscore were not significantly different between the groups. Qmax was significantly improved at 6 months postoperatively in the IPP group versus the no IPP group.
Recent studies have concentrated on prostatic configuration rather than overall prostatic volume in the etiology of bladder outlet obstruction (BOO). Several authors consider intravesical prostatic protrusion (IPP) to be a useful parameter in predicting BOO [1,2]. A higher IPP grade is associated with a higher risk of clinical progression in benign prostatic hyperplasia (BPH). Thus, resolving IPP may improve the outcome of BPH management [3]. Even if IPP is a useful predictor of clinical progression in BPH, IPP measured by abdominal ultrasound (US) is operator-dependent, which limits its broad reproducibility [4]. Flexible cystoscopy is a more invasive technique than is abdominal US; however, cystoscopy can more precisely evaluate urethral abnormalities, including bladder outlet compression. Therefore, we assessed the effectiveness of laser PVP on BPH that was evaluated by flexible cystoscopy and compared clinical outcomes between BPH patients with IPP and those without IPP.
Our university's Institutional Review Board approved this study. We enrolled 134 patients who underwent Green-Light HPS laser photoselective vaporization prostatectomy (PVP) at our institution between January 2010 and July 2011. The urethral and bladder neck anatomical configurations of the patients were evaluated by flexible cystoscopy before surgery. Patients received a minimum of 3 months of medical therapy before surgery and were not satisfied with their medical therapy. Patients received an initial baseline evaluation that included a transrectal ultrasound (TRUS) and had maximum flow rate (Qmax), postvoid residual (PVR) volume, and serum prostate-specific antigen (PSA) levels measured. Patients were also administered the International Prostate Symptom Score (IPSS) questionnaire. A lack of satisfaction with medical therapy was defined as changes from baseline in the IPSS and quality of life (QoL) scores of less than 3 and 1 points, respectively. We used the GreenLight HPS 120 W laser (American Medical Systems, Minnetonka, MN, USA) to perform the PVP procedure. Postoperatively, all patients were assessed with the IPSS and for Qmax and PVR at 1, 3, and 6 months after the operation. Exclusion criteria were current use of medications known to affect bladder function (i.e., anticholinergics), severe symptoms necessitating immediate medical or surgical intervention, complications potentially related to lower urinary tract symptoms (e.g., PSA level over 10 ng/mL, residual volumes over 200 mL, bladder stones, hematuria, and urinary retention), and an inability to speak and understand Korean. We also excluded individuals with a medical history of prostate or bladder surgery, pelvic radiotherapy, uncontrolled diabetes, dementia, any type of voiding dysfunction secondary to an underlying neurological disease, or any condition compromising mobility.
The major aims of BPH treatment are relief of patient symptoms, improvement of QoL, and alteration of disease progression. Patients with mild symptoms (i.e., IPSS≤7) that are not extremely bothersome are considered candidates for watchful waiting and were excluded from this study. In patients with moderate to severe (IPSS≥8) or bothersome symptoms, we prescribed α-blockers. We also administered 5-α-reductase inhibitors to patients whose prostate volume calculated by TRUS was greater than 30 mL. Anticholinergics were not used before PVP in enrolled patients. Other medical treatments were similar to those of the European Association of Urology guidelines for BPH [5,6]. All enrolled patients received medications for more than 3 months before surgery.
Cystoscopy (Olympus CYF-4 flexible cystoscope, 14 Fr; Olympus Europa Holding GmbH, Hamburg, Germany) was performed by one of two physicians (CDY and DHL, with 2 years of experience each) with the patient in the lithotomy position. Urethral and bladder structures were inspected conventionally except for the bladder neck, which was viewed in a retroflex position. We defined IPP as an intravesical protrusion of the prostate median lobe of more than 5 mm in diameter. The 14 Fr flexible cystoscope had a 4.7-mm diameter endoscope; therefore, we compared protruding masses by using the endoscope. Patients were subsequently assigned to either the IPP group or the no IPP group for comparison of surgical outcomes.
All men underwent PVP treatment under general or spinal anesthesia in accordance with surgeon and patient preferences. All patients received broad-spectrum antibiotics preoperatively and postoperatively. The perioperative data collected included procedure duration, irrigation volume, and length of hospital stay. During PVP, the total energy used, the number of fibers, and the eventual use of electrical coagulation or resection were also assessed. All patients were discharged after a PVR assessment following catheter removal.
The PVP technique was performed by a surgeon (SHL) with 3 years of experience, and in most instances the procedure required using only 60 W of power. The prostate lateral lobes were vaporized bilaterally at first. After creating the working space from the bladder neck to the verumontanum, the power setting was increased to 80 W, 100 W, and finally 120 W to widen the cavity. The middle lobe, if present, was vaporized after completing the lateral lobe ablation. To control bleeding when it occurred, the coagulation mode setting was used, wherein the power was reduced to 20 to 30 W and the laser beam was directed around, rather than directly at, the bleeding vessel. The fiber was introduced through a Karl Storz 23 Fr continuous flow cystoscope. Normal saline (0.9% sodium chloride solution) was used for irrigation. A 20 Fr three-way Foley catheter was inserted without irrigation in most cases.
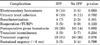
Parametric numeric data (Fig. 1, comparison of IPP and no IPP groups at each follow-up period; Fig. 2, comparison of two groups at each period) were compared by using the t-test, and nonparametric data (Table 1, comparison of complications) were analyzed by using the Wilcoxon signed-rank test. A p-value<0.05 was considered significant. Data were presented either as mean±standard deviation or mean±standard deviation (range). To compare each follow-up month's data with the baseline data, the data were analyzed by using repeated-measures analysis of variance. Calculations were performed by using SAS ver. 9.1 (SAS Institute Inc, Cary, NC, USA).
The mean patient age was 66.6±7.8 years. The mean serum PSA level and prostate volume were 1.7±1.5 ng/mL and 42.9±16.7 mL, respectively. There were no significant differences between the IPP and no IPP groups in terms of preoperative characteristics such as prostate volume, total IPSS, and PSA levels. There were also no significant differences between these two patient groups in lasing time (IPP, 29±14.3 months; no IPP, 24±15.4 months), lasing energy (IPP, 787±92.3 kJ; no IPP, 653±155 kJ), or hospital stay (IPP, 2.4±1.7 days; no IPP, 2.8±1.8 days; Table 2). The mean follow-up duration was 6.2±1.9 months.
After the operation, there were statistically significant differences compared with preoperative values in IPSS, Qmax, PVR, and QoL in both groups at the 1-, 3-, and 6-month follow-ups. The IPP group showed significant improvements in total IPSS and voiding subscores at postoperative months 1 and 3 (Table 1). However, improvement in the QoL score and storage subscore was not significantly different between the IPP and no IPP groups (Figs. 1-3). The Qmax was significantly improved at postoperative month 6 in the IPP group (+7.8 mL/s) compared with the no IPP group (+6.0 mL/s) (Fig. 4).
Operative complications and their frequencies are listed in Table 3. Intraoperative bleeding required electrocautery in nine IPP patients and three no IPP patients, and there was a similar trend for bleeding from the protruding median lobe in both patient groups. Postoperative gross hematuria presented in 16 (26%) IPP patients and in 10 (14%) no IPP patients. Four of the 16 IPP patients required recatheterization for bladder irrigation, whereas 2 of the 10 no IPP patients required recatheterization. However, the frequencies of all surgical complications were not significantly different between the two patient groups.
When using flexible cystoscopy for visualization, the bladder should be moderately filled owing to the necessity for sufficient space within which to bend the cystoscope. Therefore, we believe that IPP detection by cystoscopy is less influenced by the degree of bladder filling than is IPP evaluation via US [7]. We demonstrated here that PVP was an effective therapy for BPH patients with or without IPP. Improvement of the IPSS obstructive subscore was much higher in the IPP group than in the no IPP group during early (<3 months) postoperative follow-up. However, the superiority of the improvement in the IPP group was not sustained at a relatively late period (postoperative month 6). This might be because the elimination of a protruding mass in the bladder neck may have a greater effect on early improvement of voiding symptoms than the release of luminal compression of the prostatic urethra. Therefore, patients with IPP experience early improvement because of the elimination of IPP. According to a long-term study [8], significant improvement of obstructive symptoms after PVP was shown at months 1 and 6. Relatively more symptoms of discomfort were noted in patients with IPP than in those without IPP.
Despite the significantly lower preoperative Qmax in the IPP group, PVP resulted in marked improvement in both groups, with flow rates at the 6 months follow-up even greater in the IPP group than in the no IPP group. This finding might be due to delayed degradation of luminal compressed tissue. However, this possibility should be confirmed with further large-scale controlled studies.
Several studies have investigated the prevalence of IPP in BPH. Chia et al. [1] showed a positive correlation between IPP and BOO. They graded IPP in enrolled patients by using US and correlated these findings with urine pressure flow studies. The results showed that a higher grade of IPP correlated with a higher BOO index. Keqin et al. [9] also reported that IPP was a useful predictor of BOO and of detrusor muscle function. Lee et al. [3] argued that a higher IPP grade is associated with a higher risk of clinical progression of BPH. In that retrospective analysis of 259 men, IPP was graded as 1 (up to 5 mm protrusion), 2 (5 to 10 mm), or 3 (greater than 10 mm). With the use of predefined definitions of disease progression, including a deterioration of four points on the IPSS or an increased PVR of greater than 100 mL, the odds ratio of disease progression of a grade 3 protrusion was significantly higher than that of a grade 2 protrusion. Mariappan et al. [10] reported that a BPH trial without catheterization is more likely to fail in patients with an IPP larger than 10 mm.
Most prior studies, including those cited here, evaluated IPP by using abdominal US because of its noninvasive ability to identify intravesical anatomy. However, abdominal US has limited reliability in finding IPP and is highly operator-dependent. The degree of bladder filling also affects the accurate evaluation of IPP by use of US. Reliability is best when viewing a comfortably full bladder (-200 mL). When the bladder is overdistended (>400 mL), the prostate recedes below the pubic symphysis and is difficult to image correctly by US. In contrast, too little urine in the bladder (i.e., <100 mL) tends to result in overestimation of IPP [7]. Therefore, US findings tend to be subjective rather than definitive because of the difficulty of standardizing US procedures and the variability in patient bladder status.
Flexible cystoscopy is a reliable procedure for evaluation of the whole urethra and bladder at the same time. Although flexible cystoscopy is more invasive than US, some researchers have reported various methods for minimizing patient pain during the procedure, such as viewing the monitor and increasing hydrostatic pressure (the "bag squeeze" technique) [11,12]. Abdominal US is a noninvasive modality for the identification of vesical anatomy during optimal bladder filling. However, abdominal US cannot directly identify infravesical anatomical obstructions such as urethral obstruction or the degree of "kissing" of the prostate lateral lobes. Therefore, US can initially be useful in evaluating a patient with voiding difficulty, but this method is not ideal for following up patients who do not improve with optimal medical management for obstructive symptoms.
The PVP procedure is an effective treatment modality to manage a moderately enlarged prostate. Alexis et al reported that PVP was effective for long-term (12-month) improvement of obstruction secondary to BPH in 139 patients who had a mean prostate mass of 54.6 g [13]. Lukacs et al. [14] reported the superiority of PVP over transurethral resection of the prostate (TURP) in reducing the length of hospital stay and in improving uroflowmetry parameters. Complication rates were comparable between PVP and TURP in this multicenter prospective trial. On the basis of their meta-analysis results, Zhang et al. [15] reported that PVP and TURP provide comparable functional improvements, including lowering the IPSS and increasing the Qmax, at the 6-, 12-, and 24 months follow-ups. Korean researchers have confirmed that PVP is an effective modality for removing obstructive prostate tissue, including a protruding median lobe [16].
Long-term medical therapy for BPH has shown good efficacy and evidence of decreasing disease progression in several studies, including the MTOPS, ALTESS, CombAT, and ALF-ONE trials. However, in real clinical practice, some BPH patients are unresponsive after several months of medical treatment and require reevaluation and individually tailored disease management [17,18]. Therefore, to identify patients who require surgical correction for BPH, early evaluation of the status of the urethra and bladder by use of accurate and reliable diagnostic methods, such as flexible cystoscopy, is needed. Additionally, flexible cystoscopy is less invasive and causes less patient discomfort than does conventional rigid cystoscopy. When appropriate medical therapy over a period of months does not result in symptom improvement in BPH patients, we recommend flexible cystoscopy to confirm whether lateral lobe "kissing" or median lobe protrusion exists, which would be indications for surgical correction.
A limitation of this study is that we did not investigate the effect of more than 3 months of sustained medical therapy on BPH patients with IPP. To confirm the superiority of early intervention with flexible cystoscopy and PVP, comparative studies with extended medical therapy should be performed.
The PVP procedure resulted in significant improvement in obstructive symptoms in BPH patients, regardless of whether IPP was present. We recommend that medically nonresponsive BPH patients be reevaluated by use of flexible cystoscopy to accurately identify the cause of an obstruction in the prostatic urethra.
Figures and Tables
 | FIG. 1Changes in the total International Prostate Symptom Score (IPSS) score with time in the intravesical prostatic protrusion (IPP) and no IPP groups. a:Significant difference between the IPP and no IPP groups, p<0.05. |
 | FIG. 2Changes in the voiding subscore with time in the intravesical prostatic protrusion (IPP) and no IPP groups. a:Significant difference between the IPP and no IPP groups, p<0.05. |
 | FIG. 3Changes in the storage subscore with time in the intravesical prostatic protrusion (IPP) and no IPP groups. |
 | FIG. 4Improved maximal uroflow rate for up to 6 months after photoselective vaporization of the prostate. Qmax, maximum flow rate. a:Significant difference between the intravesical prostatic protrusion (IPP) and no IPP groups (t-test); p=0.821 at month 1, p=0.558 at month 3, p=0.047 at month 6. |
References
1. Chia SJ, Heng CT, Chan SP, Foo KT. Correlation of intravesical prostatic protrusion with bladder outlet obstruction. BJU Int. 2003. 91:371–374.
2. Doo CK, Uh HS. Anatomic configuration of prostate obtained by noninvasive ultrasonography can predict clinical voiding parameters for determining BOO in men with LUTS. Urology. 2009. 73:232–236.
3. Lee LS, Sim HG, Lim KB, Wang D, Foo KT. Intravesical prostatic protrusion predicts clinical progression of benign prostatic enlargement in patients receiving medical treatment. Int J Urol. 2010. 17:69–74.
4. Kaplan SA. Re: intravesical prostatic protrusion predicts clinical progression of benign prostatic enlargement in patients receiving medical treatment. J Urol. 2011. 185:1386–1387.
5. Madersbacher S, Alivizatos G, Nordling J, Sanz CR, Emberton M, de la Rosette JJ. EAU 2004 guidelines on assessment, therapy and follow-up of men with lower urinary tract symptoms suggestive of benign prostatic obstruction (BPH guidelines). Eur Urol. 2004. 46:547–554.
6. Novara G, Galfano A, Gardi M, Ficarra V, Boccon-Gibod L, Artibani W. Critical review of guidelines for BPH diagnosis and treatment strategy. Eur Urol Suppl. 2006. 5:418–429.
7. Yuen JS, Ngiap JT, Cheng CW, Foo KT. Effects of bladder volume on transabdominal ultrasound measurements of intravesical prostatic protrusion and volume. Int J Urol. 2002. 9:225–229.
8. Kang SH, Choi YS, Kim SJ, Cho HJ, Hong SH, Lee JY, et al. Long-term follow-up results of photoselective vaporization of the prostate with the 120 W Greenlight HPS laser for treatment of benign prostatic hyperplasia. Korean J Urol. 2011. 52:260–264.
9. Keqin Z, Zhishun X, Jing Z, Haixin W, Dongqing Z, Benkang S. Clinical significance of intravesical prostatic protrusion in patients with benign prostatic enlargement. Urology. 2007. 70:1096–1099.
10. Mariappan P, Brown DJ, McNeill AS. Intravesical prostatic protrusion is better than prostate volume in predicting the outcome of trial without catheter in white men presenting with acute urinary retention: a prospective clinical study. J Urol. 2007. 178:573–577.
11. Patel AR, Jones JS, Angie S, Babineau D. Office based flexible cystoscopy may be less painful for men allowed to view the procedure. J Urol. 2007. 177:1843–1845.
12. Gunendran T, Briggs RH, Wemyss-Holden GD, Neilson D. Does increasing hydrostatic pressure ("bag squeeze") during flexible cystoscopy improve patient comfort: a randomized, controlled study. Urology. 2008. 72:255–258.
13. Te AE, Malloy TR, Stein BS, Ulchaker JC, Nseyo UO, Hai MA, et al. Photoselective vaporization of the prostate for the treatment of benign prostatic hyperplasia: 12-month results from the first United States multicenter prospective trial. J Urol. 2004. 172(4 Pt 1):1404–1408.
14. Lukacs B, Loeffler J, Bruyere F, Blanchet P, Gelet A, Coloby P, et al. Photoselective vaporization of the prostate with GreenLight 120-W laser compared with monopolar transurethral resection of the prostate: a multicenter randomized controlled trial. Eur Urol. 2012. 61:1165–1173.
15. Zhang X, Geng J, Zheng J, Peng B, Che J, Liang C. Photoselective vaporization versus transurethral resection of the prostate for benign prostatic hyperplasia: a meta-analysis. J Endourol. 2012. 26:1109–1117.
16. Kim HS, Cho MC, Ku JH, Kim SW, Paick JS. The efficacy and safety of photoselective vaporization of the prostate with a potassium-titanyl-phosphate laser for symptomatic benign prostatic hyperplasia according to prostate size: 2-year surgical outcomes. Korean J Urol. 2010. 51:330–336.
17. Roehrborn CG. BPH progression: concept and key learning from MTOPS, ALTESS, COMBAT, and ALF-ONE. BJU Int. 2008. 101:Suppl 3. 17–21.
18. Emberton M, Fitzpatrick JM, Rees J. Risk stratification for benign prostatic hyperplasia (BPH) treatment. BJU Int. 2011. 107:876–880.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download