Abstract
Purpose
The aim of this study was to evaluate TMPRSS2:ERG fusion rates in tissue, urine, blood, and pubic hair samples in a cohort of patients with localized prostate cancer and to correlate these findings with various clinicopathological parameters.
Materials and Methods
A cohort of 40 patients undergoing radical prostatectomy for localized prostate cancer (RRP group) and 10 control patients undergoing prostate biopsy were enrolled between 2006 and 2008. Urine, pubic hair, and peripheral blood samples were obtained following prostatic massage before the needle biopsy or radical prostatectomy. Quantitative polymerase chain reaction analysis was performed on all collected samples.
Results
The patients' mean age was 62.4 (±5.5) years. We observed higher expressions of TMPRSS2:ERG fusion in tissue, urine, and blood samples from the RRP group than in samples from the control group. Overall, the fusion was present in urine samples of 23 RRP patients (57.5%). To predict high-stage cancer (>T3a), the Gleason score was the only significant factor in the logistic regression analysis (score, 10.579; p=0.001). Quantitative evaluation of the gene fusion in tissue (Pearson r=0.36, p=0.011) and urine (Pearson r=0.34, p=0.014) samples had a significant positive correlation with the preoperative prostate-specific antigen level.
Conclusions
Urine sediments collected after prostatic massage appear to be a feasible noninvasive method of detecting TMPRSS2:ERG fusion. The Gleason score is the only significant factor to predict high-stage cancer (>T3a). No correlation between TMPRSS2:ERG gene fusion status and tumor stage, Gleason grade, prostate-specific antigen level, or surgical margin status was observed.
Prostate cancer (PCa) is the most prevalent cancer in men and is the second leading cause of male cancer deaths [1]. Treatment options for patients with PCa are diverse owing to the heterogeneity of the disease, and this diversity necessitates proper stratification of patients according to risk. The validated tools we have for this purpose are the prostate-specific antigen (PSA) test and its derivatives, Gleason grade and disease stage, which are far from perfect.
The TMPRSS2:ERG gene fusion was first described in 2005 [2] as a PCa-specific biomarker, and it has been widely investigated as a new biomarker for PCa [3]. The TMPRSS2 (androgen-regulated transmembrane protease serine 2) gene codes for serine protease and is expressed in normal and malignant prostatic epithelium. ERG is a member of the ETS family of oncogenes, which act as transcriptional activators and inhibitors, usually controlled by phosphorylation. When fused with TMPRSS2, ERG comes under the control of androgens [3]. Recurrent TMPRSS2:ERG fusions are reported to be present in 50% of PCas from PSA-screened cohorts [4-7]. This genetic alteration has been studied by several groups with a focus on associated clinical and pathological parameters to assess clinical implications [8,9]. However, the results are inconsistent, with some authors indicating the presence of TMPRSS2:ERG fusion as a sign of bad prognosis in a cohort of men with localized PCa [5,10,11] and others suggesting favorable prognosis in PCa cell lines [12,13]. A very recent meta-analysis concluded that TMPRSS2:ERG fusion is associated with tumor stage at diagnosis but does not strongly predict biochemical recurrence or mortality in patients with localized PCa [14].
TMPRSS2:ERG fusion is also studied as a biomarker of PCa detected in urine (alone or in conjunction with PCA3) [15-17] and peripheral blood samples. Laxman et al. [18] reported a fusion rate of 42% in urine collected from PCa patients after a digital rectal exam (post-DRE urine), and Mao et al. [19] detected the fusion in blood samples in 10 of 15 patients with advanced PCa.
The aim of this study was to evaluate TMPRSS2:ERG fusion rates in not only prostate tissue but also post-DRE urine, blood, and pubic hair samples in a cohort of patients with localized PCa. We also investigated the correlation between various clinical and pathological parameters and the presence of the gene fusion in this patient population.
A cohort of 40 patients who were undergoing radical prostatectomy for localized PCa (RRP group) and 10 patients who proved to be free of PCa after saturation biopsy of the prostate for an elevated PSA at the Marmara University School of Medicine, Department of Urology, between 2006 and 2008 were enrolled. The inclusion criteria were as follows: 1) no history of previous PCa treatment, 2) no history of androgen deprivation therapy or chemotherapy before surgery, and 3) no evidence of metastasis (by radiological evaluation) at the time of diagnosis. All patients provided written informed consent after approval of the study by the local ethics committee.
Urine, pubic hair, and peripheral blood samples were obtained following prostatic massage before the needle biopsy or radical prostatectomy. Urine was collected in sterile urine culture specimen cups followed immediately by centrifugation of a minimum of 30 mL urine at 4,000 rpm for 15 minutes at 4℃. Samples were stored at -80℃ until RNA isolation [18]. A total of 3 pubic hair samples were obtained from each patient and immediately placed in the TriPure Isolation Reagent (Roche, Manheim, Germany). Peripheral blood samples were collected in tubes containing ethylenediaminetetraacetic acid, and all samples were stored at -80℃ until RNA isolation. Prostatic tissue samples were taken with an 18 G needle from men who underwent saturation biopsy and from surgical specimens after radical prostatectomy. Tissue cores were snap-frozen and stored at -80℃.
RNA was isolated from the samples by use of the TriPure Isolation Reagent according to the manufacturer's protocol (Roche, Mannheim, Germany). RT-PCR was performed by monitoring, in real time, the increase in fluorescence of the SYBR Green dye (Light Cycler-RNA Amplification Kit SYBR Green I, Roche) by using a Light Cycler Carousel-Based quantitative RT-PCR system (Roche) and a cytokine control commercial kit (Light Cycler Control Kit RNA, Roche).
All RNA obtained was reverse transcribed and denatured by use of random hexanucleotides according to the instructions from the manufacturer (Roche). Total mRNA was detected by use of the LightCycler Carousel-Based system. Quantitative RT-PCR was performed with published primers for TMPRSS2:ERGa as follows: CGCGGCAGGAAGCCTTA (sense) and TCCGTAGGCACACTCAAACAAC (antisense) [18]. RT-PCR conditions were as follows: reverse transcription, 10 minutes at 55℃; denaturation, 30 seconds at 95℃; annealing, 12 seconds at 55℃; extension, 15 seconds at 72℃ (45 cycles).
The amount of target gene fusion was determined relative to the housekeeping gene glyceraldehyde-3-phosphate dehydrogenase (GAPDH) by the comparative threshold cycle method (www.appliedbiosystems.com).
The quantitative PCR results of different samples were analyzed with the Mann-Whitney test according to subgroups of prognostic factors. Preoperative PSA levels and quantitative PCR results were analyzed with the Pearson correlation method. Logistic regression analysis was used to evaluate independent prognostic factors. All data analysis was conducted by using SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA).
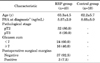
The mean age of the patients in the RRP group was 62.2 years (range, 43.0 to 78.0 years) and that of the control group was 63.3 years (range, 56.0 to 70.0 years). The clinicopathological characteristics of the patients are shown in Table 1.
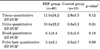
The quantitative RT-PCR results from four different samples (tissue, post-DRE urine, blood, and pubic hair) in the RRP and control groups are shown in Table 2. We observed higher expressions of the TMPRSS2:ERG fusion in tissue, post-DRE urine, and blood samples from the RRP group than in samples from the control group, but none of the differences was statistically significant. Overall, the fusion was present in post-DRE urine samples of 23 RRP patients (57.5%).
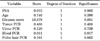
To predict high-stage cancer (>T3a), Gleason score was the only significant factor in the logistic regression analysis (score, 10.579; p=0.001). Preoperative PSA, PCR analysis, and age did not prove to be significant in this study (Table 3).
There was no correlation between gene expression in different samples and tumor stage, Gleason score, or surgical margin status (Table 4). Quantitative evaluation of the fusion gene in tissue (Pearson r=0.36, p=0.011) and post-DRE urine (Pearson r=0.34, p=0.014) samples had a significant positive correlation with preoperative PSA level, in contrast with peripheral blood and pubic hair samples.
The noninvasive detection of the TMPRSS2:ERG gene fusion in urine samples by use of quantitative PCR was first reported by Laxman et al. [18], who found a positive gene fusion rate of 42% in patients with localized PCa. Our study is unique in that all possible noninvasive detection methods were compared in the same patient cohort. We performed quantitative PCR analysis of the TMPRSS2:ERG gene fusion in easy-to-obtain patient samples such as blood, post-DRE urine, and pubic hair and compared these findings with findings from tissue samples.
Among several isoforms of the fusion gene, the TMPRSS2: ERGa isoform was used in this study. This is the most prevalent isoform, with a positivity rate of 85% to 95% among fusion-positive PCas [20].
The concentration of androgen receptors is shown to be higher in dermal papilla cells derived from androgen-dependent follicles, including the beard, moustache, pubic hair, and scrotal hair, than from elsewhere on human body, such as the scalp [21]. The rationale for analyzing pubic hair follicles in this study was to check whether this androgen-sensitive fusion gene could be detected from androgen-sensitive hair follicles in a cohort of PCa patients. We did not expect to detect the fusion gene in pubic hair follicles, but they served as an internal control in each group.
Our RT-PCR results identified higher copy numbers of the fusion gene in post-DRE urine and tissue samples than in blood and pubic hair samples in this cohort of RRP patients. Post-DRE urine and tissue samples yielded nearly 3.5 times higher levels than in the control group, whereas this difference was only 1.3 times in pubic hair samples (Table 2). Thus, we concluded that peripheral blood and pubic hair PCR analysis of TMPRSS2:ERG gene fusion seems to be suboptimal. According to our results, the samples obtained from urine after prostatic massage seemed to be as effective as direct tissue sampling.
In a recently published multicenter prospective study evaluating post-DRE urine TMPRSS2:ERG fusion status and urine PCA3 as a diagnostic adjunct to increase the accuracy of serum PSA testing, TMPRSS2:ERG fusion was found to be a significant predictor of biopsy Gleason score and clinical tumor stage [22]. Those authors confirmed the diagnostic (increase in the sensitivity of ERSPC [European Randomized Study of Screening for Prostate Cancer] risk calculator) and prognostic value of TMPRSS2:ERG fusion positivity in patients undergoing prostate biopsy. Although the present study was not designed to test the diagnostic accuracy of TMPRSS2:ERG, we observed a significant positive correlation between preoperative PSA levels and TMPRSS2:ERG fusion gene transcription in tissue and post-DRE urine. A similar correlation was reported in the literature previously [20]. Thus, post-DRE urine TMPRSS2:ERG could be a valuable biomarker to combine with serum PSA to predict clinically significant disease in PCa patients.
Unlike the previous studies [11,20,23,24] and a recent meta-analysis [14], our study could not confirm the association of the TMPRSS2:ERG fusion gene with more advanced disease. The only significant predictor among age, PSA, and the presence of gene fusion in different samples to predict high-stage cancer was the Gleason score. This was possibly due to the limited number of radical prostatectomy patients and even more limited number of pathologic >pT3a (n=8) patients involved. This represents the major limitation of this study.
Previously, TMPRSS2:ERG fusion was reported to significantly predict Gleason score and clinical tumor stage in a subcohort of patients with PSA <10 [22]. Although our PCa group comprised mostly patients who had PSA <10 (34/40), we did not find a similar association. Further prospective, high-volume studies are needed to describe the prognostic role of TMPRSS:ERG2 fusion status in different subcohorts of patients with PCa.
It was previously hypothesized that the fusion gene is present in the very early stages of PCa and it is possible to detect the fusion gene in tissue samples of patients with benign prostatic hyperplasia [25]. We also report very low expression of TMPRSS2:ERG fusion transcripts in tissue samples of biopsy-negative patients (n=10). This could be explained by either false-negative biopsies or the presence of the fusion gene in the very early stages of PCa.
In summary, our results indicated the absence of a significant correlation between TMPRSS2:ERG gene fusion status and tumor stage, Gleason grade, PSA level, and surgical margin status, although our study had limitations in patient number and follow-up time. PSA levels had a significant positive correlation with post-DRE urine and tissue transcript numbers. Thus, post-DRE urine sediments after prostatic massage appear to be a feasible noninvasive alternative in detection of the fusion. Gleason score was the only significant factor for predicting high-stage cancer (>T3a) in this study.
Figures and Tables
References
1. Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010. 60:277–300.
2. Tomlins SA, Rhodes DR, Perner S, Dhanasekaran SM, Mehra R, Sun XW, et al. Recurrent fusion of TMPRSS2 and ETS transcription factor genes in prostate cancer. Science. 2005. 310:644–648.
3. Killick E, Bancroft E, Kote-Jarai Z, Eeles R. Beyond prostate-specific antigen: future biomarkers for the early detection and management of prostate cancer. Clin Oncol (R Coll Radiol). 2012. 24:545–555.
4. Kumar-Sinha C, Tomlins SA, Chinnaiyan AM. Recurrent gene fusions in prostate cancer. Nat Rev Cancer. 2008. 8:497–511.
5. Perner S, Demichelis F, Beroukhim R, Schmidt FH, Mosquera JM, Setlur S, et al. TMPRSS2:ERG fusion-associated deletions provide insight into the heterogeneity of prostate cancer. Cancer Res. 2006. 66:8337–8341.
6. Clark J, Merson S, Jhavar S, Flohr P, Edwards S, Foster CS, et al. Diversity of TMPRSS2-ERG fusion transcripts in the human prostate. Oncogene. 2007. 26:2667–2673.
7. Shah RB, Chinnaiyan AM. The discovery of common recurrent transmembrane protease serine 2 (TMPRSS2)-erythroblastosis virus E26 transforming sequence (ETS) gene fusions in prostate cancer: significance and clinical implications. Adv Anat Pathol. 2009. 16:145–153.
8. Fine SW, Gopalan A, Leversha MA, Al-Ahmadie HA, Tickoo SK, Zhou Q, et al. TMPRSS2-ERG gene fusion is associated with low Gleason scores and not with high-grade morphological features. Mod Pathol. 2010. 23:1325–1333.
9. Barwick BG, Abramovitz M, Kodani M, Moreno CS, Nam R, Tang W, et al. Prostate cancer genes associated with TMPRSS2-ERG gene fusion and prognostic of biochemical recurrence in multiple cohorts. Br J Cancer. 2010. 102:570–576.
10. Demichelis F, Fall K, Perner S, Andren O, Schmidt F, Setlur SR, et al. TMPRSS2:ERG gene fusion associated with lethal prostate cancer in a watchful waiting cohort. Oncogene. 2007. 26:4596–4599.
11. Rajput AB, Miller MA, De Luca A, Boyd N, Leung S, Hurtado-Coll A, et al. Frequency of the TMPRSS2:ERG gene fusion is increased in moderate to poorly differentiated prostate cancers. J Clin Pathol. 2007. 60:1238–1243.
12. Hermans KG, Boormans JL, Gasi D, van Leenders GJ, Jenster G, Verhagen PC, et al. Overexpression of prostate-specific TMPRSS2(exon 0)-ERG fusion transcripts corresponds with favorable prognosis of prostate cancer. Clin Cancer Res. 2009. 15:6398–6403.
13. Saramäki OR, Harjula AE, Martikainen PM, Vessella RL, Tammela TL, Visakorpi T. TMPRSS2:ERG rearrangement is an independent marker of good prognosis in prostate cancer [abstract 730]. Eur Urol Suppl. 2008. 7:253.
14. Pettersson A, Graff RE, Bauer SR, Pitt MJ, Lis RT, Stack EC, et al. The TMPRSS2:ERG rearrangement, ERG expression, and prostate cancer outcomes: a cohort study and meta-analysis. Cancer Epidemiol Biomarkers Prev. 2012. 21:1497–1509.
15. Salagierski M, Schalken JA. Molecular diagnosis of prostate cancer: PCA3 and TMPRSS2:ERG gene fusion. J Urol. 2012. 187:795–801.
16. Young A, Palanisamy N, Siddiqui J, Wood DP, Wei JT, Chinnaiyan AM, et al. Correlation of urine TMPRSS2:ERG and PCA3 to ERG+ and total prostate cancer burden. Am J Clin Pathol. 2012. 138:685–696.
17. Tomlins SA, Aubin SM, Siddiqui J, Lonigro RJ, Sefton-Miller L, Miick S, et al. Urine TMPRSS2:ERG fusion transcript stratifies prostate cancer risk in men with elevated serum PSA. Sci Transl Med. 2011. 3:94ra72.
18. Laxman B, Tomlins SA, Mehra R, Morris DS, Wang L, Helgeson BE, et al. Noninvasive detection of TMPRSS2:ERG fusion transcripts in the urine of men with prostate cancer. Neoplasia. 2006. 8:885–888.
19. Mao X, Shaw G, James SY, Purkis P, Kudahetti SC, Tsigani T, et al. Detection of TMPRSS2:ERG fusion gene in circulating prostate cancer cells. Asian J Androl. 2008. 10:467–473.
20. Rostad K, Hellwinkel OJ, Haukaas SA, Halvorsen OJ, Oyan AM, Haese A, et al. TMPRSS2:ERG fusion transcripts in urine from prostate cancer patients correlate with a less favorable prognosis. APMIS. 2009. 117:575–582.
21. Randall VA, Thornton MJ, Messenger AG. Cultured dermal papilla cells from androgen-dependent human hair follicles (e.g. beard) contain more androgen receptors than those from non-balding areas of scalp. J Endocrinol. 1992. 133:141–147.
22. Leyten GH, Hessels D, Jannink SA, Smit FP, de Jong H, Cornel EB, et al. Prospective multicentre evaluation of PCA3 and TMPRSS2-ERG gene fusions as diagnostic and prognostic urinary biomarkers for prostate cancer. Eur Urol. 2012. 11. 15. [Epub].http://dx.doi.org/10.1016/j.eururo.2012.11.014.
23. Attard G, Clark J, Ambroisine L, Fisher G, Kovacs G, Flohr P, et al. Duplication of the fusion of TMPRSS2 to ERG sequences identifies fatal human prostate cancer. Oncogene. 2008. 27:253–263.
24. Wang J, Cai Y, Ren C, Ittmann M. Expression of variant TMPRSS2/ERG fusion messenger RNAs is associated with aggressive prostate cancer. Cancer Res. 2006. 66:8347–8351.
25. Velaeti S, Kalogeropoulos T, Karaolidis T, Dimitriadis E, Kontogianni-Katsarou K, Savvani A, et al. Detection of TMPRSS2-ERG fusion gene in benign prostate hyperplasia. Eur Urol Suppl. 2009. 8:614.
26. Lee K, Chae JY, Kwak C, Ku JH, Moon KC. TMPRSS2-ERG gene fusion and clinicopathologic characteristics of Korean prostate cancer patients. Urology. 2010. 76:1268.e7–1268.e13.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download