Abstract
Malacoplakia is a chronic inflammatory disease. The disease mainly affects the urinary bladder, although involvement of extravesical sites is increasingly being documented. Most frequently involved is the urinary tract, particularly the urinary bladder, although the testis, epididymis, lungs, bone, colon, prostate, female genital organs, and retroperitoneum can also be involved. Here we report the case of a 61-year-old man with a scrotal mass with histology that was specific for malacoplakia of the epididymis. The histologic workup demonstrated extensive involvement of the epididymis by diffuse infiltrates of large histiocytes with eosinophilic granular cytoplasm and numerous Michaelis-Gutmann bodies, which were diagnostic of malakoplakia. This is the first case of epididymal malacoplakia in our country and the first case of epididymal malacoplakia without concurrent involvement of the testis. There have been few reports of this condition worldwide.
Malakoplakia is an uncommon but distinctive type of chronic granulomatous inflammation that is characterized histologically by the presence of sheets of histiocytes with granular cytoplasm (von Hansemann cells) admixed with intracellular and extracellular basophilic laminated inclusions (Michaelis-Gutmann bodies). There have been five reports of this condition in Korea [1]. The present case, however, is the first case of epididymal malacoplakia without concurrent involvement of the testis. Approximately 75% of cases of malacoplakia are located in the genitourinary system. Although the exact etiology of malakoplakia remains poorly understood, it is commonly associated with microbial infections and states of diminished immune response [2]. Here we report an unusual case of malakoplakia that involved the epididymis in a 61-year-old man with a scrotal mass.
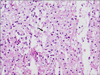
A 61-year-old man presented with a painful mass of his left epididymis for several months. He had no fever or history of trauma. The measured values of hematological parameters and urine indexes were within the normal range. Urine culture did not reveal any growth. Ultrasonography of the left epididymis revealed a mass lesion of mixed echotexture in the epididymal tail (Fig. 1). The patient underwent epididymectomy. Histopathology showed an epididymal mass comprising sheets of histiocytes with granular eosinophilic cytoplasm (Fig. 2) admixed with neutrophils, lymphocytes, and plasma cells. Many of the histiocytes contained small round to oval targetoid structures that were morphologically consistent with Michaelis-Gutmann bodies. These histologic findings were characteristic of malakoplakia. The patient's postoperative recovery was uneventful and the surgical outcome has been satisfactory for 8 months.
Malakoplakia, derived from the Greek adjective malakos (soft) and plaka (plaque), was first described in 1902 by Michaelis and Gutmann and was clearly explained by McClue in his review [3]. Epididymal malakoplakia was first described in 1968 by Green [4], and there have been five reports of this condition in Korea [1].
Malakoplakia, which typically involves the urinary tract, is an uncommon form of chronic inflammation caused by chronic infections and characterized by accumulation of macrophages [5]. It has also been found in various sites such as the gastrointestinal tract, pancreas, liver, lymph nodes, skin, respiratory tract, adrenal gland, vagina, and brain [2].
Definitive diagnosis of the lesion can be made by histopathologic examination. Malacoplakia is characterized histologically by the presence of Michaelis-Gutmann bodies contained within von Hansemann macrophages. This likely represents phagolysosomes that contain partially digested bacterial debris. Malacoplakia typically occurs in immunocompromised patients who experience recurrent Escherichia coli urinary tract infections [6]. Extensive sectioning may be required to look for the classic Michaelis-Gutmann bodies. Special stains such as periodic acid Schiff and von Kossa for calcium can be particularly helpful in highlighting the Michaelis-Gutmann bodies when these are obscured within dense lymphohistiocytic infiltrate.
The etiology of malakoplakia has not been fully elucidated. It is commonly associated with microbial infections and states of diminished immune response. Frequent association of bladder malakoplakia with urinary tract infection suggests an infectious etiologic agent. Coliform bacteria, particularly E. coli, have been isolated from the involved sites of genitourinary malakoplakia in more than two-thirds of patients [2]. Another potential contributing factor to the development of malakoplakia is an impaired immune response. In a review by Long and Althausen [5], approximately 40% of malakoplakia cases that did not involve the urinary tract were associated with immunosuppression [3]. The ability of phagocytes to completely digest bacteria is impaired in malakoplakia, which is thought to be related to low levels of intracellular cyclic guanosine monophosphate (cGMP) and diminished release of b-glucuronidase. This would explain the successful treatment of a case with the cholinergic agonist bethanechol chloride, which acts by increasing the levels of cGMP [7,8].
The treatment options for malakoplakia include two main approaches: the administration of antibiotics and surgical excision, depending on the site and extent of involvement. Antibiotics that can penetrate the cell membrane and concentrate in macrophages are associated with a high cure rate. Treatment with trimethoprim-sulfamethoxazole may be helpful because of the ability of trimethoprim to enhance the killing of viable undigested microorganisms inside malakoplakic macrophages. Also, because ciprofloxacin penetrates well into macrophages, this drug has been found to be particularly useful in patients with advanced malakoplakia [9]. In addition to these agents, bethanechol is believed to enhance phagocytic bactericidal activity by increasing cGMP levels [8]. If conservative treatment fails to control and diminish the malakoplakia, which is the most likely situation according to most investigators, surgical resection is needed. Close follow-up of these patients is needed because multiple locations can be affected. In our case, our preoperative differential diagnosis was an epididymal mass caused by chronic epididymitis. Considering the involvement of the epididymis in our patient, who had no fever and negative results on urinalysis and urine culture, excision of the epididymal mass was the best option without antibiotic therapy, and this treatment led to a satisfactory outcome.
Figures and Tables
References
1. Park KW, Seo IY, Rim JS. Vesical malacoplakia misdiagnosed as urachal cancer. Korean J Urol. 2002. 43:177–179.
2. Yousef GM, Naghibi B, Hamodat MM. Malakoplakia outside the urinary tract. Arch Pathol Lab Med. 2007. 131:297–300.
3. McClure J. Malakoplakia. J Pathol. 1983. 140:275–330.
4. Green WO Jr. Malacoplakia of the epididymis (without testicular involvement): the first reported case. Arch Pathol. 1968. 86:438–441.
5. Long JP Jr, Althausen AF. Malacoplakia: a 25-year experience with a review of the literature. J Urol. 1989. 141:1328–1331.
6. Sulman A, Goldman H. Malacoplakia presenting as a large bladder mass. Urology. 2002. 60:163.
7. Abdou NI, NaPombejara C, Sagawa A, Ragland C, Stechschulte DJ, Nilsson U, et al. Malakoplakia: evidence for monocyte lysosomal abnormality correctable by cholinergic agonist in vitro and in vivo. N Engl J Med. 1977. 297:1413–1419.
8. Stanton MJ, Lynch JH, Maxted WC, Chun BK. Malacoplakia of the bladder: a case report of resolution with bethanechol, trimethoprim-sulfamethoxazole and ascorbic acid. J Urol. 1983. 130:1174–1175.
9. van Furth R, van't Wout JW, Wertheimer PA, Zwartendijk J. Ciprofloxacin for treatment of malakoplakia. Lancet. 1992. 339:148–149.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download