Abstract
Purpose
To evaluate alterations in renal function after laparoscopic radical nephrectomy (LRN) and laparoscopic partial nephrectomy (LPN) for renal tumors.
Materials and Methods
From March 2008 to August 2011, we performed 175 cases of laparoscopic kidney resection. Among these, we excluded patients who received perioperative immunotherapy or target therapy and also patients with a preoperative estimated glomerular filtration rate (eGFR) <60 mL/min. A total of 32 patients undergoing LPN and 92 patients undergoing LRN were enrolled. We retrospectively reviewed the changes in eGFR (by the modification of diet in renal disease method) at the following time points: preoperative, postoperative 1 week, and postoperative 1, 3, 6, and 12 months.
Results
The mean warm ischemia time of the LPN group was 22 minutes (range, 0 to 47 minutes). Mean eGFR values (mL/min/1.73 m2) during postoperative week 1 and 1, 3, 6, and 12 months were 70.8, 71.5, 76.7, 76.0, and 75.3 in the LPN group and 52.1, 50.6, 52.8, 53.4, and 52.4 in the LRN group, respectively. One year after the operation, 6.3% (2 patients) of LPN patients and 68.5% (63 patients) of LRN patients had progressed to chronic renal insufficiency (eGFR<60 mL/min/1.73 m2).
Conclusions
Renal function recovered slightly after LPN and LRN and was maintained constantly after 3 months. However, renal function showed different patterns of decrease. Despite the concern for warm ischemia, LPN can preserve renal function better than can LRN. LPN should be considered for selected patients to prevent chronic renal insufficiency.
Traditionally, open radical nephrectomy is the standard treatment for renal tumors. However, nephron-sparing surgery (NSS) has increasingly been performed for T1 renal tumors owing to the ability of this technique to preserve renal function while resulting in equivalent oncologic outcomes [1]. After the first report on laparoscopic partial nephrectomy (LPN) by Winfield et al. [2] and McDougall et al. [3], the technique for laparoscopic renal surgery has gradually evolved. However, because of the technical difficulty of LPN, it has been performed in only selected cases by a few urologists. The main concern for LPN is disability owing to renal hypothermia, which is used for preservation of renal function in open partial nephrectomy (OPN). Laparoscopically, some novel approaches for renal hypothermia have been reported [4-6], but the application of renal hypothermia is difficult and most urologists still perform LPN with warm ischemia. In a few studies, OPN showed comparable oncological results with radical nephrectomy and superior long-term renal function to radical nephrectomy [1]. Although OPN has advantages for renal function preservation, there are few data comparing the recovery of renal function following laparoscopic partial and radical nephrectomy. The aim of this study was therefore to compare the recovery of renal function after LRN and LPN.
After obtaining Institutional Review Board approval, we retrospectively reviewed collected data for laparoscopic renal surgery. From March 2008 to August 2011, a total of 175 patients underwent laparoscopic kidney resection. Among these, we excluded patients who underwent laparoscopic nephroureterectomy, laparoscopic simple nephrectomy and received perioperative immunotherapy, or target therapy and also patients with preoperative chronic renal insufficiency (CRI).
All laparoscopic renal surgeries were performed by a single surgeon (TSK). All LPNs were performed via a transperitoneal approach. In brief, during control of the hilar vessels in LPN, mannitol (12.5 g) was administered, and the renal arteries were clamped by using a vessel loop and Hem-o-Lok clips en-loading. The renal veins were not clamped routinely. The renal mass was dissected by using cold 10 mm Metzenbaum scissors with approximately 5 mm safety margins. After tumor excision, the calyceal system, bleeders, and tumor bed were closed by using 3-0 Vicryl sutures. Thereafter, FloSeal (Baxter, Deerfield, IL, USA) and Surgicel bolsters were applied for bleeders, and the renal parenchyma was closed by using Vicryl 2-0 sutures (Ethicon Inc., Spmervile, NJ, USA). LRNs were performed transperitoneally except for four patients who were approached retroperitoneally owing to previous extensive abdominal surgery. Hilar vessels were controlled by using Hem-o-Lok clips (Weck Closure Systems, Research Triangle Park, NC, USA) or endovascular GIA staplers (Multifire Endo GIA30 stapler, Covidien, Dublin, Ireland).
After the operation, most patients were assessed by physical examination, chest X-ray, and eGFR at postoperative 1 week, 1 month, 3 months, 6 months, and 12 months, and abdominal computed tomography was assessed at 6 and 12 months. We evaluated renal function by eGFR by using the abbreviated modification of diet in renal disease equation. CRI was defined by eGFR <60 mL/min/1.73 m2.
The LPN and LRN groups were compared regarding perioperative renal function and surgical and clinical variables. We used the Student's t-test for continuous variables and Fisher's exact test for categorical variables. We performed simple and multiple regression analysis for predicting eGFR. All statistical analyses were performed by using PASW ver. 18.0 (IBM Co., Armonk, NY, USA) with a two-sided test, and p-values<0.05 were considered statistically significant.
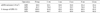
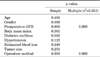
Among the 175 patients who underwent laparoscopic kidney resection, a total of 32 patients undergoing LPN and 92 patients undergoing LRN were enrolled. The characteristics of the patients are summarized in Table 1. The mean age, sex, body mass index (BMI), prevalence of hypertension, and prevalence of diabetes mellitus were similar between the two groups. However, the preoperative mean radiologically evaluated renal tumor size was significantly smaller in the LPN group (3.3 cm vs. 4.1 cm, p<0.001). Mean operating time and estimated blood loss were not significantly different between the two groups. The mean warm ischemia time (WIT) of the LPN group was 22 minutes (range, 0 to 47 minutes). Overall, 90.6% and 97.8% of tumors were malignant in the LPN and LRN groups, respectively. Three benign tumors in the LPN group were angiomyolipomas, and two benign tumors in the LRN group were oncocytomas. Fig. 1 and Table 2 show the changes in perioperative renal function. The mean preoperative eGFR (mL/min/1.73 m2) was 81.7 in the LPN group and 80.3 in the LRN group. The mean eGFR (mL/min/1.73 m2) at postoperative 1 week, 1 month, 3 months, 6 months, and 12 months was 70.8, 71.5, 76.7, 76.0, and 75.3 in the LPN group and 52.1, 50.6, 52.8, 53.4, and 52.4 in the LRN group, respectively. At postoperative 1 year, 6.3% (2 patients) in the LPN group and 68.5% (63 patients) in the LRN group had progressed to CRI. However, no patients in either group required dialysis. In multiple linear regression analysis, preoperative eGFR and operation method (LRN or LPN) were significant factors predicting postoperative eGFR (Table 3).
Recently, the application of NSS for small renal tumors has expanded owing to increased use of abdominal imaging studies. Despite the concerns that existed regarding oncological outcomes in the early era of NSS, it was shown that NSS produces excellent oncological results with minimal complication rates [1]. With the development of laparoscopic instrumentation and techniques, indications for LPN have expanded. During mass excision and renal parenchymal reconstruction, surgeons have to clamp the hilar vessels to achieve a clear operation field to ensure minimal blood loss and accurate laparoscopic suturing. In the case of OPN, cold ischemia with ice slush can be used to minimize ischemic renal damage. However, effective cold ischemia is very difficult to achieve during a laparoscopic approach. LPN with WIT has been allowed despite the risk for deterioration of renal function. There are several risk factors for deterioration of renal function in LPN, such as renal volume reduction, tumor location, patient age, longer WIT, and preoperative eGFR, and among these, the factor modifiable by the laparoscopic technique is WIT [7-12]. Bhayani et al. [13] reported that WIT, up to 55 minutes, did not influence renal function by postoperative 6 months. In contrast, Thompson et al. [14] studied the comparison of warm ischemia versus no ischemia in LPN for a solitary kidney, and they concluded that warm ischemia in a solitary kidney is associated with the development of new-onset CRI. Recently, the cutoff of WIT has received much attention. Thompson et al. [8] reported that partial nephrectomy with a WIT of greater than 25 minutes was significantly associated with CRI. Funahashi et al. [15] and Porpiglia at al. [16] also reported that when the WIT was greater than 25 minutes, postoperative effective renal plasma flow was significantly decreased. In the present study, the mean WIT was 22 minutes, and we had difficulty in determining a cutoff for the WIT because of the small sample size and because only two patients reached CRI at 1 year postoperatively. These two patients had normal preoperative eGFR and no history of smoking, hypertension, or diabetes mellitus. Their resected masses were 2.5 cm and 3.0 cm, and their WIT values were 25 minutes and 33 minutes, respectively. In the LRN group of the present study, 68.5% of the patients had an eGFR under 60 mL/min/1.73 m2; therefore, despite the risk of a prolonged WIT, LPN resulted in superior renal function upon follow-up.
Park et al. [17] reported that renal function in patients who underwent LPN under the pneumoperitoneal condition was similar to that of patients who underwent OPN. Adamy et al. [18] reported that renal function 6 months post-LPN was slightly increased compared with postoperative 2 months and was then maintained at a constant level. Our study also showed that the renal function at 3 months post-LPN was slightly increased compared with postoperative 1 month and was then maintained at a constant increased state up to postoperative 1 year. This pattern of renal function change is similar in LRN (Fig. 1); however, decreasing renal function was greater than in LPN, and 68.5% of LRN patients had decreased renal function, with eGFR values under 60 mL/min/1.73 m2.
Zorn et al. [19] studied the effects on long-term serum creatinine after LPN. They reported that about 36.4% of LRN patients developed CRI (serum creatinine above 1.5 mg/dL), whereas none in the LPN group developed CRI. This was the first report making a comparative study of renal function after LPN and LRN. Despite several limitations, such as the lack of use of eGFR and the retrospective nature of the study, this result may encourage laparoscopic urologists to perform LPN. Another study by the same group demonstrated that LPN in T1b renal tumors also had a benefit for renal function compared with LRN (30.3% vs. 55.7%, estimated creatinine clearance under 60 mL) [20]. Although the mean WIT was relatively longer (34 minutes) in T1b renal tumors, long-term renal function was better than in LRN. Thus, if technically feasible, even in the case of a large renal mass, LPN can benefit renal function compared with LRN. The present study did have several limitations. The sample size of the study was small, it was a nonrandomized single-institute study, and we did not use a renal scan for renal function assessment.
Long-term renal function was maintained constantly at postoperative 3 months in both the LPN and LRN groups. However, renal function after the operation showed different patterns of decrease. Regarding progression to CRI, LPN with WIT has advantages over LRN. Laparoscopic urologists should consider performing LPN to prevent CRI in selected patients.
Figures and Tables
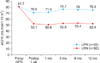 | FIG. 1The change of estimated glomerular filtration rate (eGFR) after renal surgery. LPN, laparoscopic partial nephrectomy; LRN, laparoscopic radical nephrectomy; Preop, preoperative. |
References
1. Herr HW. Partial nephrectomy for unilateral renal carcinoma and a normal contralateral kidney: 10-year followup. J Urol. 1999. 161:33–34.
2. Winfield HN, Donovan JF, Godet AS, Clayman RV. Laparoscopic partial nephrectomy: initial case report for benign disease. J Endourol. 1993. 7:521–526.
3. McDougall EM, Clayman RV, Anderson K. Laparoscopic wedge resection of a renal tumor: initial experience. J Laparoendosc Surg. 1993. 3:577–581.
4. Gill IS, Abreu SC, Desai MM, Steinberg AP, Ramani AP, Ng C, et al. Laparoscopic ice slush renal hypothermia for partial nephrectomy: the initial experience. J Urol. 2003. 170:52–56.
5. Landman J, Venkatesh R, Lee D, Vanlangendonck R, Morissey K, Andriole GL, et al. Renal hypothermia achieved by retrograde endoscopic cold saline perfusion: technique and initial clinical application. Urology. 2003. 61:1023–1025.
6. Janetschek G, Abdelmaksoud A, Bagheri F, Al-Zahrani H, Leeb K, Gschwendtner M. Laparoscopic partial nephrectomy in cold ischemia: renal artery perfusion. J Urol. 2004. 171:68–71.
7. Shikanov S, Lifshitz D, Chan AA, Okhunov Z, Ordonez MA, Wheat JC, et al. Impact of ischemia on renal function after laparoscopic partial nephrectomy: a multicenter study. J Urol. 2010. 183:1714–1718.
8. Thompson RH, Lane BR, Lohse CM, Leibovich BC, Fergany A, Frank I, et al. Renal function after partial nephrectomy: effect of warm ischemia relative to quantity and quality of preserved kidney. Urology. 2012. 79:356–360.
9. Choi JD, Park JW, Lee SY, Jeong BC, Jeon SS, Lee HM, et al. Does prolonged warm ischemia after partial nephrectomy under pneumoperitoneum cause irreversible damage to the affected kidney? J Urol. 2012. 187:802–806.
10. Song C, Bang JK, Park HK, Ahn H. Factors influencing renal function reduction after partial nephrectomy. J Urol. 2009. 181:48–53.
11. Simmons MN, Fergany AF, Campbell SC. Effect of parenchymal volume preservation on kidney function after partial nephrectomy. J Urol. 2011. 186:405–410.
12. Simmons MN, Hillyer SP, Lee BH, Fergany AF, Kaouk J, Campbell SC. Functional recovery after partial nephrectomy: effects of volume loss and ischemic injury. J Urol. 2012. 187:1667–1673.
13. Bhayani SB, Rha KH, Pinto PA, Ong AM, Allaf ME, Trock BJ, et al. Laparoscopic partial nephrectomy: effect of warm ischemia on serum creatinine. J Urol. 2004. 172(4 Pt 1):1264–1266.
14. Thompson RH, Lane BR, Lohse CM, Leibovich BC, Fergany A, Frank I, et al. Comparison of warm ischemia versus no ischemia during partial nephrectomy on a solitary kidney. Eur Urol. 2010. 58:331–336.
15. Funahashi Y, Hattori R, Yamamoto T, Sassa N, Fujita T, Gotoh M. Effect of warm ischemia on renal function during partial nephrectomy: assessment with new 99mTc-mercaptoacetyltriglycine scintigraphy parameter. Urology. 2012. 79:160–164.
16. Porpiglia F, Fiori C, Bertolo R, Angusti T, Piccoli GB, Podio V, et al. The effects of warm ischaemia time on renal function after laparoscopic partial nephrectomy in patients with normal contralateral kidney. World J Urol. 2012. 30:257–263.
17. Park H, Byun SS, Kim HH, Lee SB, Kwon TG, Jeon SH, et al. Comparison of laparoscopic and open partial nephrectomies in t1a renal cell carcinoma: a Korean multicenter experience. Korean J Urol. 2010. 51:467–471.
18. Adamy A, Favaretto RL, Nogueira L, Savage C, Russo P, Coleman J, et al. Recovery of renal function after open and laparoscopic partial nephrectomy. Eur Urol. 2010. 58:596–601.
19. Zorn KC, Gong EM, Orvieto MA, Gofrit ON, Mikhail AA, Msezane LP, et al. Comparison of laparoscopic radical and partial nephrectomy: effects on long-term serum creatinine. Urology. 2007. 69:1035–1040.
20. Deklaj T, Lifshitz DA, Shikanov SA, Katz MH, Zorn KC, Shalhav AL. Laparoscopic radical versus laparoscopic partial nephrectomy for clinical T1bN0M0 renal tumors: comparison of perioperative, pathological, and functional outcomes. J Endourol. 2010. 24:1603–1607.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download