Abstract
Purpose
The objective of this study was to retrospectively investigate postoperative infectious complications (PICs) in our early experience with holmium laser enucleation of the prostate (HoLEP) followed by mechanical morcellation for symptomatic benign prostatic hyperplasia.
Materials and Methods
A retrospective review was performed of the clinical data for 90 consecutive patients who underwent HoLEP at our institution between February 2008 and March 2011. All patients were evaluated for the emergence of PICs, including prophylactic antibiotic administration (PAA) and the influence of the kind or duration of PAA on PIC. The details of cases with PICs were also examined.
Results
The patients' mean age was 71 years (range, 50 to 95 years), and their mean prostate volume was 60 mL (range, 2 to 250 mL). There were 7 cases (7.78%) with PICs; in detail, 3 patients were diagnosed with prostatitis, 2 with pyelonephritis, and 2 with epididymitis. Three patients had positive urine cultures: 1 had Serratia marcescens/Proteus mirabilis, 1 had S. marcescens, and 1 had Klebsiella pneumonia; only one case had urological sepsis. Our statistical data showed no significant differences between 2 or fewer days and 3 or more days of PAA and PIC occurrence. There was also no significant effect on PIC occurrence of sulbactam/ampicillin compared with other antibiotics.
Lower urinary tract symptoms (LUTS) due to benign prostatic hyperplasia (BPH) are one of the most common diseases in elderly males [1]. Patients in general are prescribed an alpha-blocker first and then, if necessary, are treated by transurethral resection of the prostate (TURP) if not enough response to the alpha-blocker is shown [2]. TURP has been accepted as the gold standard for the surgical management of symptomatic BPH [3]. Even though several excellent alpha-blockers are in use, some patients with severe LUTS require surgical therapy. Our county's guidelines recommend surgical management for patients with BPH with repeated urinary retention or bladder stone formation [4]. Recently, surgical therapy has come to include methods thought to be relatively less invasive than TURP [5]. These new methods have resulted in lower morbidity and excellent improvements in voiding and storage symptoms [6]. For example, holmium laser enucleation of the prostate (HoLEP) has become a widespread and well-accepted treatment modality with excellent outcomes compared to other conventional treatment modalities such as TURP and open prostatectomy [7,8].
Because this surgical procedure is comparatively new, surgeons tend to concentrate on the completion of the surgery, and most previous reports regarding HoLEP have described the efficacy of the procedure for patients' urination. As a next step, surgeons need to consider whether this procedure can be performed safely with a comparatively lower rate of adverse events than TURP. This new technique should not only be less invasive and offer better efficacy for urination but also show a lower ratio of adverse events, especially in terms of postoperative infectious diseases [9].
In this study, we retrospectively examined the incidence of postoperative infectious complications (PICs) in our early experience with HoLEP for BPH with a particular focus on the kind and duration of prophylactic antibiotic administration (PAA).
A retrospective study was conducted in 90 patients complaining of LUTS who underwent HoLEP combined with morcellation at our institute between February 2008 and March 2011. All patients presented with LUTS due to BPH with or without overactive bladder.
Briefly, a modified 26-Fr continuous-flow resectoscope (Karl Storz GmbH & Co., Tuttlingen, Germany) was used for enucleation of the prostate. A 550-µm end-firing laser fiber (SlimLine 550; Lumenis Inc., Yoqneam, Israel) was engaged with an 80 W holmium:yttrium-aluminum-garnet laser (VersaPulse Select, Lumenis Inc., Yoqneam, Israel). Energy power was usually set at 72 to 80 W (1.8 to 2.4 J and 30 to 40 Hz) and at 0.2 J and 40 Hz for hemostasis. Continuous irrigation was applied with normal saline during enucleation and morcellation. Tissue morcellation was performed with a VersaCut morcellator (VersaCut system, Lumenis Inc.) through a 6-degree rectangular nephroscope (Karl Storz GmbH & Co.). During the transurethral procedure, the outer sheath was always in the urethra, because the resectoscope and nephroscope were exchangeable in the outer sheath. After completion of the morcellation, a urethral catheter was inserted for continuous bladder irrigation with normal saline.
PAA was given intravenously for all patients. The kind and the dosing duration of PAA were based on the physicians' discretion. PAA was as a rule started intravenously 30 minutes before surgery.
PICs were diagnosed according to the Centers for Disease Control and Prevention (CDC) guidelines [10]; in short, a PIC was defined as a febrile (body temperature ≥38℃) complication caused by a surgical procedure at a surgical site, such as urinary tract infection (UTI), that occurred within 30 days after surgery.
We analyzed the relationship between the emergence of PICs and the kind or duration of PAA. Statistical analysis was conducted with the JSTAT Java Virtual Machine Statistics Monitoring Tool with use of the chi-square test (Sun Microsystems Inc., Santa Clara, CA, USA). Statistical significance was established at p<0.05.
The baseline characteristics of the patients are summarized in Table 1. Median patient age was 72 years. Most patients had previously received an alpha-blocker. Forty percent of the patients had a history of urinary retention. Twenty-three (25.6%) had an indwelling catheter owing to urinary retention (Table 1).
The patients' general complications are shown in Table 2. Diabetes was seen in 19 patients (21.1%), heart disease in 17 (18.9%), and hypertension in 15 (16.7%). Urological cancer was seen in 3 patients (2 patients had bladder cancer and 1 renal cancer).
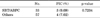
There were 18 patterns regarding the kind and duration of PAA; the details are shown in Table 3. The most frequently used PAA was sulbactam/ampicillin (SBT/ABPC; n=32, 35.6%), followed by cefazolin (n=18, 20.0%) and cefotiam (n=9, 10.0%).
We examined the influence of the kind or duration of dosing of PAA on PCC occurrence. Our statistical data showed that there were no significant differences between 2 or fewer days and 3 or more days of PAA dosing with regard to PIC occurrence. There were also no significant differences between SBT/ABPC, which was most frequently used in this study, and other antibiotics for PAA with regard to PIC occurrence (Tables 4, 5).
PIC was diagnosed in 7 cases, and the PAA of the cases was 3 SBT/ABPC, 2 tazobactam/piperacillin, 1 cefazolin, and 1 cefotiam (Table 4). The detailed outcomes are shown in Table 6. There were 3 cases of prostatitis, 2 cases of pyelonephritis, and 2 cases of epididymitis. One case was diagnosed as sepsis after prostatitis caused by Klebsiella pneumoniae and was cured by use of doripenem, cefazolin, and levofloxacin. In all, 2 cases of Serratia marcescens, 1 case of Proteus mirabilis, and 1 case of K. pneumonia were cultured, and these were quite different from the preoperative culture data shown above, which suggested that preoperative treatments might be effective (Table 6).
HoLEP for BPH has become widespread in the urological field and has recently been performed at many institutions [11]. HoLEP may involve less stress to patients [12] and should offer a lower rate of surgical site infection and postsurgical complications than open surgery or TURP. This is beneficial to patients and has supported the spread and acceptance of HoLEP [13]. This surgery has the benefit of less extensive injury to prostatic tissue than TURP [14]; thus, postsurgical local inflammation may not be as severe as with TURP [15]. Inflammation could be one risk factor for PICs, such as prostatitis [16], and therefore HoLEP may also be beneficial for suppressing PICs [17]. Basically, HoLEP is thought to cause the patients less stress in addition to having higher efficacy for LUTS [18]. However, the present study had 7 cases of PICs, and this ratio may be comparatively higher than in other reports [9]. There are several possible reasons for this; 1) Our 90 cases were performed by 7 surgeons including beginners with less than 5 cases of experience with HoLEP. Even though it is not clear whether there is a significant relationship between longer surgical time and a higher ratio of PIC occurrence, beginners or less-experienced surgeons take more time to accomplish the surgery than experienced surgeons [9], both to finish the surgical procedures such as enucleation or tissue morcellation and to avoid surgery-related adverse events. 2) PAA may not have included the most appropriate kind of antibiotics or duration of dosing. This is because the CDC guidelines and Japanese guidelines recommend that first-generation cephalosporins be administered every 2 to 3 hours during surgery and that penicillins, first-generation or second-generation cephalosporins, and aminoglycosides be administered within 72 hours in TURP, respectively [19].
In addition, discrepancies may exist between PAA performance and guideline recommendations in individual cases. This is because, for instance, the Japanese guideline recommends first-generation or second-generation cephalosporins, penicillins, and aminoglycosides for TURP as mentioned above but has not yet established guidelines for HoLEP [19]. Our most often used PAA is SBT/ABPC and the duration of dosing is recommended to be within 72 hours. However, our cases tended to have a longer duration of dosing with a higher ratio of PIC occurrence than in other reports [20], even in preoperative nonpyuria cases. Our statistical data showed that PIC occurrence did not depend on the kind or duration of PAA, which suggests that we may be able to shorten the duration of PAA, which may lead to the control of unnecessary antibiotic use.
Regarding causative bacteria, the PIC cases included 2 cases of S. marcescens, 1 case of P. mirabilis, and 1 case of K. pneumonia. Other reports showed Escherichia coli to be the representative causative bacteria [21]. Our comparatively broader spectrum PAA than recommended in guidelines or other reports, or preoperative intervention against preoperative pyuria cases, might have accounted for this difference.
We would like to emphasize the study limitations. This was a retrospective study and the number of cases was not enough for making definitive conclusions. Second, some of our cases were performed by surgeons who were less experienced with HoLEP and showed a comparatively higher ratio of PIC. Third, our PAA duration of dosing tended to be longer and the kind of antibiotics tended to be broad spectrum, which could lead to the emergence and spread of resistant strains [22]. Future studies should be performed to address these problems.
Figures and Tables
TABLE 3
Prophylactic antibiotic administration (PAA) and postoperative infectious complication (PIC)

TABLE 4
Comparison between 2 or less days and 3 or more days or prophylactic antibiotic administration in postoperative infectious complication (PIC)

ACKNOWLEDGMENTS
We thank Gary Mawyer, MFA, for English editing and Dr. Minori Matsumoto for taking care of patients.
References
1. Lee SH, Chung BH, Kim CS, Lee HM, Kim CI, Yoo TK, et al. Survey on benign prostatic hyperplasia distribution and treatment patterns for men with lower urinary tract symptoms visiting urologists at general hospitals in Korea: a prospective, non-controlled, observational cohort study. Urology. 2012. 79:1379–1384.
2. Hong KP, Byun YJ, Yoon H, Park YY, Chung WS. Prospective factor analysis of alpha blocker monotherapy failure in benign prostatic hyperplasia. Korean J Urol. 2010. 51:488–491.
3. Furuya R, Ogura H, Furuya S, Masumori N. Study of patients with symptomatic benign prostatic hyperplasia who underwent transurethral resection of the prostate after ineffective alpha-1 blocker treatment by non-urologists. Hinyokika Kiyo. 2006. 52:95–98.
4. Homma Y, Gotoh M, Yokoyama O, Masumori N, Kawauchi A, Yamanishi T, et al. Outline of JUA clinical guidelines for benign prostatic hyperplasia. Int J Urol. 2011. 18:741–756.
5. Lee NG, Xue H, Lerner LB. Trends and attitudes in surgical management of benign prostatic hyperplasia. Can J Urol. 2012. 19:6170–6175.
6. Berardinelli F, Hinh P, Wang R. Minimally invasive surgery in the management of benign prostatic hyperplasia. Minerva Urol Nefrol. 2009. 61:269–289.
7. Eltabey MA, Sherif H, Hussein AA. Holmium laser enucleation versus transurethral resection of the prostate. Can J Urol. 2010. 17:5447–5452.
8. Kelly DC, Das A. Holmium laser enucleation of the prostate technique for benign prostatic hyperplasia. Can J Urol. 2012. 19:6131–6134.
9. Hwang JC, Park SM, Lee JB. Holmium laser enucleation of the prostate for benign prostatic hyperplasia: effectiveness, safety, and overcoming of the learning curve. Korean J Urol. 2010. 51:619–624.
10. Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 1999. 27:97–132.
11. Bae J, Choo M, Park JH, Oh JK, Paick JS, Oh SJ. Holmium laser enucleation of prostate for benign prostatic hyperplasia: seoul national university hospital experience. Int Neurourol J. 2011. 15:29–34.
12. Zhao CB, Li JC, Yuan PQ, Hong YQ, Lu B, Zhao SC. A meta-analysis of holmium laser enucleation of the prostate for benign prostatic hyperplasia. Zhonghua Nan Ke Xue. 2011. 17:1112–1120.
13. Suardi N, Gallina A, Salonia A, Briganti A, Cestari A, Guazzoni G, et al. Open prostatectomy and the evolution of HoLEP in the management of benign prostatic hyperplasia. Minerva Urol Nefrol. 2009. 61:301–308.
14. Montorsi F, Naspro R, Salonia A, Suardi N, Briganti A, Zanoni M, et al. Holmium laser enucleation versus transurethral resection of the prostate: results from a 2-center prospective randomized trial in patients with obstructive benign prostatic hyperplasia. J Urol. 2008. 179:5 Suppl. S87–S90.
15. Shah HN, Mahajan AP, Hegde SS, Bansal MB. Peri-operative complications of holmium laser enucleation of the prostate: experience in the first 280 patients, and a review of literature. BJU Int. 2007. 100:94–101.
16. Knopf HJ, Funke PJ. Significance of bacterial prostatic colonization for nosocomial urinary tract infections after transurethral prostate resection. Urologe A. 2000. 39:432–435.
17. Kuo RL, Paterson RF, Siqueira TM Jr, Watkins SL, Simmons GR, Steele RE, et al. Holmium laser enucleation of the prostate: morbidity in a series of 206 patients. Urology. 2003. 62:59–63.
18. Djavan B, Eckersberger E, Handl MJ, Brandner R, Sadri H, Lepor H. Durability and retreatment rates of minimal invasive treatments of benign prostatic hyperplasia: a cross-analysis of the literature. Can J Urol. 2010. 17:5249–5254.
19. Matsumoto T, Kiyota H, Matsukawa M, Yasuda M, Arakawa S, Monden K, et al. Japanese guidelines for prevention of perioperative infections in urological field. Int J Urol. 2007. 14:890–909.
20. Raz R, Almog D, Elhanan G, Shental J. The use of ceftriaxone in the prevention of urinary tract infection in patients undergoing transurethral resection of the prostate (TUR-P). Infection. 1994. 22:347–349.
21. Grabe M, Forsgren A, Hellsten S. Species distribution and antibiotic sensitivity of bacteria isolated pre- and postoperatively from patients undergoing transurethral prostatic resection. Scand J Urol Nephrol. 1984. 18:187–192.
22. Guyot A, Barrett SP, Threlfall EJ, Hampton MD, Cheasty T. Molecular epidemiology of multi-resistant Escherichia coli. J Hosp Infect. 1999. 43:39–48.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download