Abstract
Purpose
The target of our work was to study several biochemical parameters in phospho-calcic and bone metabolism in blood and urine and the bone mineral density of women with recurrent calcium nephrolithiasis.
Materials and Methods
We conducted a cross-sectional study with a control group of 85 women divided into 3 groups: group 1 consisted of 25 women without a history of nephrolithiasis, group 2 consisted of 35 women with only one episode of calcium nephrolithiasis, and group 3 consisted of 25 women with a history of recurrent calcium nephrolithiasis. Blood and urine biochemical study was performed, including markers related to lithiasis, and a bone mineral density study was done by use of bone densitometry.
Results
Patients in group 3 showed statistically significantly elevated calciuria (15.4 mg/dL), fasting calcium/creatinine ratio (0.14), and 24-hour calcium/creatinine ratio (0.21) compared with groups 1 and 2. Moreover, this group of women with recurrent calcium nephrolithiasis had significantly elevated values of beta-crosslaps, a bone resorption marker, compared with groups 1 and 2 (p=0.000) and showed more bone mineral density loss than did these groups.
Nephrolithiasis is clinically more frequent during the third and fourth decades of life, and the most common composition of stones is calcium. There is a male predominance of incidence (ratio of 1.5-2 for men compared with women), and the first event occurs later in women. Likewise, recurrent episodes are more frequent in men than in women, with a ratio 1.5-1 (for men compared with women) [1]. Metabolic imbalances are thought to be more common in men with recurrent nephrolithiasis in terms of hypercalciuria and hypocitraturia [2,3], and an understanding of stone formation is important for knowing the diseases responsible for recurrent calcium nephrolithiasis [4]. One of the processes related to recurrent calcium nephrolithiasis is osteopenia/osteoporosis, which is described in 60% of patients diagnosed with idiopathic calcium lithiasis and hypercalciuria. It is also true that bone mineral density may be reduced in patients with calcium stones and without hypercalciuria [5]. This loss is measureable by bone densitometry, which allows us to classify patients in the following categories according to the T-score: normal (>-1), osteopenia (T-score between -1 and -2.5), osteoporosis (<-2.5), and established osteoporosis (<-2.5 and fracture) [6]. Another way to measure and indirectly diagnose bone mineral density loss is by markers of bone formation and resorption, which permit us to monitor and follow up patients after the establishment of an antiresorptive treatment [7].
The target of our work was to study the relationship between recurrent calcium nephrolithiasis and bone mineral density loss as well as to evaluate biochemical markers in the blood and urine of women with recurrent calcium nephrolithiasis.
This was a cross-sectional study with a control group. A total of 85 women were divided into three groups as follows: group 1 consisted of 25 women aged between 30 and 60 years without calcium nephrolithiasis, group 2 consisted of 35 women aged between 30 and 60 years with a history of only one episode of calcium nephrolithiasis, and group 3 consisted of 25 women aged between 30 and 60 years with recurrent calcium nephrolithiasis.
Women in group 1 were enlisted from among women who consulted the outpatient department of urology at the San Cecilio Hospital of Granada because of cystitis. Patients in groups 2 and 3 were enrolled from the Department of Urolithiasis and Endourology at the San Cecilio Hospital of Granada. The study was assessed and approved by the ethics committee of the hospital.
Imaging study was performed in all patients to diagnose calcium nephrolithiasis. The imaging included renal and bladder ultrasonography and conventional radiography with or without intravenous pyelography.
We considered recurrent calcium nephrolithiasis as two or more episodes of nephrolithiasis during 3 years or bilateral nephrolithiasis [7]. All patients included in our study maintained a balanced calcium diet (approximately 1,000 mg/d), which was controlled by anamnesis and dietary recommendations.
The inclusion criteria were women aged between 30 and 60 years without nephrolithiasis, with only one episode of nephrolithiasis, or with recurrent nephrolithiasis. The exclusion criteria were as follows: women younger than 30 years or older than 60 years; women with established bone disease; immobilized patients; women with noncalcium nephrolithiasis; women with tumor pathology; women receiving thiazide, sodium bicarbonate, bisphosphonates, calcium supplements, or vitamin D; and women with nephrocalcinosis, primary hyperparathyroidism, distal renal tubular acidosis, or other pathologies that were secondarily related to bone mineral density loss and nephrolithiasis.
A chemical analysis was performed of the composition of the stones of patients in groups 2 and 3. Biochemical analysis was conducted of the following variables in blood collected after the subjects had fasted for 8 hours: creatinine, urea, uric acid, calcium, phosphorus, alkaline phosphatase, parathyroid hormone (PTH), osteocalcin, beta-crosslaps, and vitamin D. Biochemical analysis of urine included fasting and 24-hour calcium/creatinine ratio, creatinine clearance, creatinine, calcium, phosphate, uric acid, oxalate, citrate, chlorine/phosphorus ratio, calcium/oxalate, and tubular reabsorption of phosphate. Bone densitometry was performed by use of a QDR 4500 (Hologic, Bedford, MA, USA), which uses dual-energy X-ray absorptiometry.
Unpaired, two-tailed Student's t-tests were applied to compare the mean values of quantitative variables, the Kolmogorov-Smirnov test was used to examine the normality of their distribution, and the Levene test was used to study the variance. The Mann-Whitney U test was used if the variables were not normally distributed. Qualitative variables were analyzed with the chi-square test or Fisher's exact test if at least one cell had an expected count <5. Correlations among variables were studied by using the Pearson coefficient or Spearman's methods if the variables were non-normally distributed. Levels of the studied parameters in the three groups were compared by use of the analysis of variance test for multiple variables. The total 85 women were also divided into two groups according to menopausal status (group A, nonmenopausal women; group B, menopausal women), and differences in levels of parameters between the two groups were determined by using Student's t-test. The proportion of patients without nephrolithiasis to that with only one episode and that with recurrent nephrolithiasis was compared by using the chi-square test, taking p<0.05 to indicate statistical significance. The SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA) was used for the data analyses.
The average age of the patients was 43.4 years in group 1, 40.3 years in group 2, and 46.3 years in group 3, with no statistically significant differences among the groups.
The calculi composition in groups 2 and 3 was as follows: 36% of stones composed of calcium oxalate-phosphate, 22% composed of calcium phosphate, 21% composed of calcium oxalate monohydrate, 10% composed of calcium oxalate dihydrate, and 11% composed of mixed calcium oxalate in group 2 and 45% of stones composed of calcium oxalate-phosphate, 15% composed of calcium phosphate, 14% composed of calcium oxalate monohydrate, 12% composed of calcium oxalate dihydrate, and 14% composed of mixed calcium oxalate in group 3. There were no significant differences between the groups.
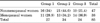
We observed statistically significant differences in blood biochemical parameters among the 3 groups: in levels of alkaline phosphatase (58.1 U/L in group 1, 59.8 U/L in group 2, and 78.9 U/L in group 3), intact PTH (PTHi; 43.7 pg/mL in group 1, 46.7 pg/mL in group 2, and 64.7 pg/mL in group 3), and beta-crosslaps (0.335 ng/mL in group 1, 0.326 ng/mL in group 2, and 0.519 ng/mL in group 3). These differences in bone metabolism among the three groups were evident in bone densitometry. There were statistically significant differences in the T-score of the hip, neck of femur, and lumbar spine. These are shown in Table 1.
In the urinary analysis, statistically significant differences were found among parameters related to calcium excretion, such as calciuria (10.1 mg/dL in group 1, 15.4 mg/dL in group 2, and 15.4 mg/dL in group 3; p=0.01), fasting calcium/creatinine ratio (0.08 in group 1, 0.11 in group 2, and 0.14 in group 3; p=0.000), and 24-hour calcium/creatinine ratio (0.14 in group 1, 0.18 in group 2, and 0.21 in group 3; p=0.01). In addition, citrate levels were significantly lower in group 3 than in groups 1 and 2 (Table 2).
We divided the 85 patients according to menopausal status into group A (nonmenopausal) and group B (menopausal). We observed statistically significant differences in terms of body mass index (24.7 in group A, 28.7 in group B; p=0.000) and biochemical blood parameters. Specifically, uric acid, alkaline phosphatase, and PTHi were higher in group B. We also found statistically significant differences in levels of uric acid excretion and fasting and 24-hour calcium/creatinine ratios, which were higher in group B, whereas tubular reabsorption of phosphate was slightly but significant lower in group B than in group A (Table 3). As shown in Table 4, no significant differences in nephrolithiasis were found between menopausal and nonmenopausal patients (p=0.212).
We observed a positive linear relationship between beta-crosslaps and the fasting calcium/creatinine ratio (r=0.359, p=0.001), between beta-crosslaps and osteocalcin (r=0.448, p=0.0001), and between PTH and the fasting and 24-hour calcium/creatinine ratio (r=0.345, p=0.002, and r=0.365, p=0.001, respectively).
Around 70% of patients with one episode of calcium nephrolithiasis experience a relapse during the first 10 years. Thus, this population must be closely followed and, even after this first episode, be evaluated with a complete metabolic study because the rule is recurrence [8,9]. Some authors defend that metabolic study and analysis of stone are important for determining different profiles of lithogenic risk, which allows for adequate treatment to be based on risk [10]. In this sense, there are several articles about metabolic alterations in patients with nephrolithiasis and assessment of these according to age and sex. Lancina Martin et al. [1] published in 2002 that women with calcium stone disease have hypercalciuria as the most frequent metabolic disorder and absorptive disorder as the most common of these, although resorptive hypercalciuria was more prevalent in women than in men with a statistically significant difference. Those authors described a calcium/creatinine ratio in this group of women of 0.17, which is similar to the value we obtained in our group of women with recurrent calcium nephrolithiasis, both fasting and 24-hour (0.14 and 0.21, respectively). Meanwhile, Yagisawa et al. [2] published a similar study that showed that urinary calcium excretion is the determining factor of the appearance of recurrent nephrolithiasis, a fact with which we agree. We showed in our study that calciuria and the fasting and 24-hour calcium/creatinine ratio were significantly higher in the group with recurrent calcium nephrolithiasis. As Spivacow et al. [11] and Vella et al. [12] remind us in their work, monitoring patients by serial metabolic study is very important, because 50% of these patients are going to show metabolic alterations along years of evolution of stone disease. A relationship between these metabolic changes and bone metabolism has been established, and in some cases, bone mineral loss is directly connected with nephrolithiasis, with the second being a consequence of the first. Up to 60% of patients with calcium nephrolithiasis show hypercalciuria, and many of them also show bone mineral density loss, which could be caused by diet or by changes in the balance of bone formation and resorption [5,13]. We demonstrated a close relationship between recurrent nephrolithiasis and bone mineral density loss, because bone mineral density loss was significantly higher in group 3 than in groups 1 and 2. In addition, we showed a significant increase in beta-crosslaps, a bone resorption marker, in group 3. Although there were no significant differences in calciuria between groups 2 and 3, bone resorption was increased in group 3. This may have been due to decreased calcium intake in these women, which would result in hypocalcemia, increased PTH, and increased bone resorption without an excessive increase in calciuria to maintain serum calcium values. Tsuji et al. [14] observed that stone-former patients with hypercalciuria suffer from greater bone mineral density loss than do normocalciuric patients, especially when patients are more than 40 years old, which is likely related to menopause. In this sense, after dividing our study group according to menopause (menopausal and nonmenopausal women), we only found differences in bone density loss of the lumbar spine (p=0.033), although these patients did have differences in bone density of the femoral neck that were close to being statistically significant (p=0.07). However, we did not find a higher incidence of recurrent nephrolithiasis in menopausal patients (p=0.212). Giannini et al. [15] observed that postmenopausal women with osteoporosis show hypercalciuria that is directly related to lumbar spine mineral density loss and recommend analysis of calciuria in these patients. Moreover, a higher incidence of bone fractures has been observed in patients with nephrolithiasis who were treated with thiazide, which decreases urinary calcium excretion and seems to prevent these fractures.
Nowadays, bone densitometry is considered the gold standard for the diagnosis of osteoporosis [1,16], but recent research has highlighted that measuring bone formation and resorption markers could improve diagnosis. Several lines of research have shown that bone markers are increased even in the premenopausal period without evident changes in bone mineral density loss as shown by densitometry [5]. These markers could be useful for diagnosis; in fact, we highlighted in our study that alkaline phosphatase and beta-crosslaps were significantly higher in group 3 (patients with recurrent calcium nephrolithiasis), which was the group of women with higher bone mineral density loss. Although it is not written in guides, these markers could be used for monitoring patients with osteopenia/osteoporosis who are treated with antiresorptive therapy [17,18].
As we have observed, an accurate assessment of the metabolic factors that trigger stone disease will help us to take steps in prevention or treatment and in managing the stabilization of stone disease and bone mineral density. Tiselius [19] established a group of preventive recommendations about eating habits that decrease disease relapse . If we specifically refer to hypercalciuria, treatment with thiazide has shown efficacy in these patients [20,21], and if the patients also show associated bone mineral density loss, they can profit from monotherapy or combined treatment with bisphosphonates [22,23].
We have shown a relationship between increased urinary calcium and bone mineral density loss. In a cross-sectional study, it is difficult to establish causality. As a hypothesis for future studies, we can establish that the loss of calcium by the kidneys produces hypocalcemia, which is corrected by an increase in PTHi with a consequent increase in bone resorption. However, hypercalciuria due to renal calcium loss is rare and it is more logical to think that a decrease in calcium intake results in hypocalcemia and increased bone resorption mediated by PTH. It will be important to address these two hypotheses in future studies of patients with prolonged follow-up.
Women with recurrent calcium nephrolithiasis show bone mineral density loss that is revealed by the presence of high calciuria, as in fasting and 24-hour urine. Moreover, these patients show higher levels of beta-crosslaps, a bone resorption marker that is related to higher fasting calciuria levels and higher bone mineral density loss. Accurate diagnosis is very important to make treatment and monitoring easier in these patients.
Figures and Tables
References
1. Lancina Martin JA, Rodriguez-Rivera Garcia J, Novas Castro S, Rodriguez Gomez I, Fernandez Rosado E, Alvarez Castelo L, et al. Metabolic risk factors in calcium urolithiasis according to gender and age of the patients. Actas Urol Esp. 2002. 26:111–120.
2. Yagisawa T, Hayashi T, Yoshida A, Kobayashi C, Okuda H, Ishikawa N, et al. Comparison of metabolic risk factors in patients with recurrent urolithiasis stratified according to age and gender. Eur Urol. 2000. 38:297–301.
3. Konstantinova OV, Ianenko EK, Dzeranov NK. Recurrence-free and recurrent urolithiasis: metabolic differences. Urologiia. 1999. (5):8–9.
4. Menditto VG, Milanese G, Muzzonigro G. Metaphylaxis of urolithiasis. Arch Ital Urol Androl. 2009. 81:32–39.
5. Caudarella R, Vescini F, Buffa A, La Manna G, Stefoni S. Osteoporosis and urolithiasis. Urol Int. 2004. 72:Suppl 1. 17–19.
6. Kanis JA, McCloskey EV, Johansson H, Oden A, Melton LJ 3rd, Khaltaev N. A reference standard for the description of osteoporosis. Bone. 2008. 42:467–475.
7. Arrabal-Polo MA, Arrabal-Martin M, de Haro-Munoz T, Poyatos-Andujar A, Palæo-Yago F, Zuluaga-Gomez A. Biochemical determinants of severe lithogenic activity in patients with idiopathic calcium nephrolithiasis. Urology. 2012. 79:48–54.
8. Amaro CR, Goldberg J, Amaro JL, Padovani CR. Metabolic assessment in patients with urinary lithiasis. Int Braz J Urol. 2005. 31:29–33.
9. Marangella M, Vitale C, Bagnis C, Bruno M, Ramello A. Idiopathic calcium nephrolithiasis. Nephron. 1999. 81:Suppl 1. 38–44.
10. Areses Trapote R, Urbieta Garagorri MA, Ubetagoyena Arrieta M, Mingo Monge T, Arruebarrena Lizarraga D. Evaluation of renal stone disease: metabolic study. An Pediatr (Barc). 2004. 61:418–427.
11. Spivacow FR, del Valle EE, Zancheta JR. Renal lithiasis. Biochemical changes in the follow-up. Medicina (B Aires). 2006. 66:201–205.
12. Vella M, Karydi M, Coraci G, Oriti R, Melloni D. Pathophysiology and clinical aspects of urinary lithiasis. Urol Int. 2007. 79:Suppl 1. 26–31.
13. Caudarella R, Vescini F, Buffa A, Sinicropi G, Rizzoli E, La Manna G, et al. Bone mass loss in calcium stone disease: focus on hypercalciuria and metabolic factors. J Nephrol. 2003. 16:260–266.
14. Tsuji H, Umekawa T, Kurita T, Uemura H, Iguchi M, Kin K, et al. Analysis of bone mineral density in urolithiasis patients. Int J Urol. 2005. 12:335–339.
15. Giannini S, Nobile M, Dalle Carbonare L, Lodetti MG, Sella S, Vittadello G, et al. Hypercalciuria is a common and important finding in postmenopausal women with osteoporosis. Eur J Endocrinol. 2003. 149:209–213.
16. Enrique CT. Osteoporosis: consideraciones diagnosticas y terapéuticas. Rev Med Hered. 2004. 15:101–107.
17. Bonnick SL, Shulman L. Monitoring osteoporosis therapy: bone mineral density, bone turnover markers, or both? Am J Med. 2006. 119:4 Suppl 1. S25–S31.
18. Kim SW, Park DJ, Park KS, Kim SY, Cho BY, Lee HK, et al. Early changes in biochemical markers of bone turnover predict bone mineral density response to antiresorptive therapy in Korean postmenopausal women with osteoporosis. Endocr J. 2005. 52:667–674.
19. Tiselius HG. Advisory Board of European Urolithiasis Research and EAU Health Care Office Working Party for Lithiasis. Possibilities for preventing recurrent calcium stone formation: principles for the metabolic evaluation of patients with calcium stone disease. BJU Int. 2001. 88:158–168.
20. Arrabal-Martin M, Fernandez-Rodriguez A, Arrabal-Polo MA, Garcia-Ruiz MJ, Zuluaga-Gomez A. Extracorporeal renal lithotripsy: evolution of residual lithiasis treated with thiazides. Urology. 2006. 68:956–959.
21. Legroux-Gerot I, Catanzariti L, Marchandise X, Duquesnoy B, Cortet B. Bone mineral density changes in hypercalciuretic osteoporotic men treated with thiazide diuretics. Joint Bone Spine. 2004. 71:51–55.
22. Arrabal Martin M, Diaz de la Guardia FV, Jimenez Pacheco A, Lopez Leon V, Arrabal Polo MA, Zuluaga Gomez A. The treatment of renal lithiasis with biphosphonates. Arch Esp Urol. 2007. 60:745–754.
23. Giusti A, Barone A, Pioli G, Girasole G, Siccardi V, Palummeri E, et al. Alendronate and indapamide alone or in combination in the management of hypercalciuria associated with osteoporosis: a randomized controlled trial of two drugs and three treatments. Nephrol Dial Transplant. 2009. 24:1472–1477.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download