Abstract
Purpose
The objective was to determine predictive factors for premature discontinuation of docetaxel-based systemic chemotherapy in men with castration-resistant prostate cancer (CRPC).
Materials and Methods
We retrospectively reviewed the medical records of men who were treated with docetaxel-based systemic chemotherapy for CRPC in a single institution between May 2005 and April 2010. After being screened, 30 patients fit the eligibility criteria for inclusion in this study. Group 1 included 12 patients who were treated with five or fewer cycles of docetaxel chemotherapy for CRPC, and group 2 included 18 patients who were treated with six or more cycles of docetaxel chemotherapy for CRPC. The treatment consisted of 5 mg prednisolone twice daily and 75 mg/m2 docetaxel once every 3 weeks.
Results
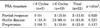
The median age was 72 years, and the median Eastern Cooperative Oncology Group (ECOG) performance status was 0. The median baseline prostate-specific antigen (PSA) level was 33.8 ng/mL. The median cycle of docetaxel-based chemotherapy was 5.8. Of 30 patients, 13 patients (48.2%) had a decline in PSA of >50% from baseline; 3 of 22 patients (13.6%) with measurable disease had achieved partial response on imaging. No differences in age, ECOG performance status, hemoglobin, serum creatinine, or PSA response were observed between the two groups. Body mass index was significantly lower (p=0.034) in group 1 (21.8 kg/m2) than in group 2 (23.6 kg/m2). Group 1 included more patients with prior systemic chemotherapy (p=0.039), and group 1 had a shorter overall survival rate (p=0.039).
In Korea, prostate cancer was the fifth most common cancer in men in 2008 (6,471 new cases) [1]. Metastatic prostate cancer is initially treated with androgen deprivation therapy, which produces a rapid decrease in bone pain and a decrease in prostate-specific antigen (PSA). However, most cases of prostate cancer progress to castration-resistant prostate cancer (CRPC) within a median of 18 to 24 months after castration [2]. Men with CRPC may experience symptomatic progression, which results in weight loss, fatigue, or pain from bone metastases, all of which can negatively affect quality of life. Two landmark trials (TAX327 and Southwest Oncology Group 9916) showed superior survival and pain palliation with the use of docetaxel-based regimens compared with mitoxantrone plus prednisolone [3,4].
The prognostic nomograms developed by several investigators use clinical information to predict overall survival in men with CRPC [5-7]. Of the prognostic factors, continuation of docetaxel and prednisolone is significantly associated with overall survival beyond progression. Several postchemotherapy factors were highly associated with postprogression su rvival in a multivariate analysis: the number of progression factors (including PSA, pain, or radiologic progression) and the number of cycles of docetaxel chemotherapy [8,9]. An increased duration of taxane chemotherapy improved locoregional control in patients with node-positive breast cancer [10]. In addition, molecularly targeted therapies with cytostatic properties and documented tolerability have the potential to be effective as maintenance therapy to maintain tumor regression after an initial response to chemotherapy in nonsmall cell lung cancer [11]. However, many patients with CRPC did not complete protocol docetaxel-based systemic chemotherapy because of drug-related adverse events or disease progression. The predictive factors for completing protocol docetaxel-based systemic chemotherapy in men with CRPC are poorly characterized. Therefore, we conducted a study to determine the predictive factors for premature discontinuation of docetaxel-based chemotherapy in Korean men with CRPC.
Between May 2005 and April 2010, 36 patients with CRPC were treated with docetaxel-based systemic chemotherapy at our institution. The patients' medical records were retrospectively reviewed to determine the predictive factors for premature discontinuation of docetaxel-based systemic chemotherapy in men with CRPC. Prostate adenocarcinoma was diagnosed in all patients by transrectal ultrasonography-guided prostate biopsy or transurethral resection of the prostate. All patients received combined androgen blockade, such as luteinizing hormone-releasing hormone agonist plus bicalutamide. CRPC was defined as three consecutive increases in PSA above the nadir with a castration level of serum testosterone, continued increase of PSA after antiandrogen withdrawal, or the existence of clear clinical or radiologic evidence of progression. The Eastern Cooperative Oncology Group performance status was 0 to 2. The mean number of docetaxel chemotherapy cycles was 5.8. Therefore, patients were divided into two groups: the first group consisted of patients who received less than six cycles of docetaxel-based systemic chemotherapy, whereas the second group consisted of patients who received six or more cycles of docetaxel-based systemic chemotherapy. This retrospective study was approved by the institutional review board.
The pretreatment evaluation included a complete medical history, a physical examination, a complete blood cell count, serum chemistry tests, a serum PSA measurement, a chest X-ray, computed tomography of the abdomen and pelvis, and a bone scan. Patients received 75 mg/m2 of docetaxel every 3 weeks and 5 mg of prednisolone twice daily. A physical examination, complete blood cell count, serum PSA measurement, and serum chemistry tests were performed every 3 weeks. Radiologic evaluations were performed every three cycles. Docetaxel-based systemic chemotherapy was continued until disease progression, unacceptable drug-related toxicities, or clinically significant concomitant disease.
All patients were evaluated for PSA response, measurable disease response, time to PSA progression, and overall survival. PSA response was evaluated according to the guidelines of the PSA working group [12]. PSA response was defined as a reduction from baseline of at least 50%. PSA progression was defined as an increase from baseline. Stable disease was defined as a decrease in PSA that did not reach PSA response criteria. Objective response was evaluated according to the Response Evaluation Criteria of Solid Tumors (RECIST) [13]. The start time of time to progression was the day on which treatment was initiated. Overall survival was defined as the time between the first docetaxel administration and death.
Adverse events were classified according to the Common Toxicity Criteria of the National Cancer Institute (version 2.0). If grade 3 or 4 hematologic or nonhematologic toxicity was observed during treatment, the docetaxel dose was adjusted to 75% of the original dose.
The clinico-pathological data were compared between the two groups. The Mann-Whitney U test was used for continuous parameters, and Fisher's exact test was used for categorical parameters to compare responses between groups. The time to progression and the overall survival curve were calculated by using the Kaplan-Meier method with the log-rank test. The results were considered significant at a p-value of <0.05. All statistical analyses were performed using the SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA).
A total of 30 patients were included in this study; the median age was 72 years, and the median performance status was 0. Six patients were excluded in this study because of incomplete clinic-pathological data and follow-up loss. The median pretreatment PSA level in the patients was 33.8 ng/mL, and the median Gleason score was 8. Twenty-two patients were chemo-naive, whereas the other eight patients were previously treated with chemotherapy. Prior chemotherapy regimens included mitoxantrone (six patients), estramustine (two patients), and paclitaxel plus etoposide (one patient). Three patients received external beam radiation therapy prior to docetaxel-based systemic chemotherapy (Table 1). The mean number of docetaxel chemotherapy cycles was 5.8. The docetaxel dose was adjusted to 75% of the original dose in five patients because of hematologic toxicities. Disease progression was the most common reason for discontinuation of chemotherapy (23 of 30 patients), followed by treatment-related toxicity determined by a physician (4 patients), and treatment refusal for toxicity (3 patients). Statistically significant differences in body mass index (BMI), prior systemic chemotherapy, and overall survival were noted. Men who continued six cycles of docetaxel chemotherapy had a low rate of prior systemic chemotherapy and a higher BMI.
Twenty-seven patients were assessable for PSA response, and 13 patients (48.2%) showed a confirmed partial PSA response. The PSA response rate was higher (p=0.013) in group 2 (11.1%) than in group 1 (66.7%) (Table 2). Twenty-two patients had measurable disease according to RECIST. Overall, 3 patients (13.6%) showed a partial response, and 14 patients (63.6%) showed stable disease according to RECIST. The measurable disease response rates did not differ between the two groups (0% compared with 15.8%, p=0.629) (Table 3).
Median progression-free survival was 6.5 months (range, 0 to 22 months), and median overall survival was 12 months (range, 2 to 30 months). The median time to PSA progression did not differ between the two groups. The median overall survival times were 6 months (range, 2 to 29 months) for men who did not complete six cycles of docetaxel chemotherapy and 13 months (range, 9 to 30 months) for men who completed six cycles of docetaxel chemotherapy (p=0.039) (Fig. 1). Five patients experienced grade 3 or higher neutropenia.
In this retrospective analysis of single-institution data from Korea, we observed that men with prolonged docetaxel-based systemic chemotherapy have longer survival times than do men with discontinuation-protocol docetaxel-based systemic chemotherapy (13 compared with 6 months). Furthermore, men with prior systemic chemotherapy and a lower BMI (21.8 compared with 23.6 kg/m2) tend to stop protocol docetaxel-based systemic chemotherapy.
The US Food and Drug Administration (FDA) approved docetaxel for first-line chemotherapy with progressive CRPC based on two trials that demonstrated an improvement in overall survival [3,4]. Although docetaxel plus prednisone extended survival compared with mitoxantrone, the overall benefit was modest; most patients experienced disease progression within 7 months. The TROPIC trial, a phase 3 trial that compared cabazitaxel and prednisone with mitoxantrone plus prednisone for patients with CRPC who had progressed after first-line docetaxel, led to FDA approval of cabazitaxel as postdocetaxel therapy for CRPC in 2010 [14]. With the development of multiple novel agents in current development in this second-line setting, there is a renewed interest in understanding and characterizing the prognostic factors for survival. Several prognostic nomograms exist for men with metastatic CRPC who are undergoing systemic docetaxel-based systemic chemotherapy [5-8]. The multivariate model designed by Armstrong et al. [5] is based on a single trial (TAX 327) conducted in men who received the current systemic standard of care. The prognostic factors included liver metastasis, the number of metastasis sites, pain, performance status, PSA doubling time, PSA, tumor grade, alkaline phosphatase, and serum hemoglobin level. Halabi et al. [15] investigated the predictive factors of overall survival in men with metastatic CRPC by analyzing nine Cancer and Leukemia Group B trials. The predictive factors of overall survival include any progression at 3 months, age, performance status, BMI, Gleason score, serum hemoglobin, race, prior radiotherapy, serum alkaline phosphatase, PSA, and lactase dehydrogenase. Armstrong et al. [8] evaluated predictors of overall survival following progression after systemic chemotherapy in men with CRPC in their TAX327 trial. They found that several prechemotherapy factors remained highly associated with postprogression survival: significant baseline pain, Karnofsky performance status, alkaline phosphatase, number of sites of metastatic disease, liver metastases, hemoglobin, and time since diagnosis. They also found that several postchemotherapy factors were highly associated with postprogression survival in a multivariate analysis: number of progression factors (PSA, pain, or radiologic progression), whether progression occurred during first-line chemotherapy administration, and the number of cycles of chemotherapy. In this study, lower BMIs and prior chemotherapy were predictive factors for premature discontinuation of docetaxel-based systemic chemotherapy in men. Pond et al. [9] suggested that an increased duration of docetaxel improved survival, until 10 cycles, in their sub-analysis of TAX 327. An increased duration of taxane chemotherapy also improved locoregional control in patients with node-positive breast cancer [10].
Although the continuation of systemic chemotherapy is associated with overall survival in men with CRPC, the predictive factors for premature discontinuation of docetaxel-based systemic chemotherapy are not well understood. In this study, men with prior systemic chemotherapy and a lower BMI tended to discontinue docetaxel chemotherapy. The correlation between BMI and outcomes for patients with prostate cancer is both complex and not well understood. Several studies have shown that obesity increases the prostate cancer recurrence rate and disease progression in men with prostate cancer [16-20]. Su et al. [16] observed a positive association between obesity and aggressive prostate cancer in white Americans (odds ratio, 1.42). In a study of 3,169 men who underwent radical prostatectomy, Amling et al. [17] reported that an elevated BMI was associated with a greater frequency of adverse pathological outcomes. Freedland et al. [18] used the SEARCH database to assess the correlation between obesity and time to biochemical progression in 1,106 men who underwent radical prostatectomy. On multivariate analysis, the hazard ratio for biochemical progression was 2.09 for patients with a BMI indicating moderate to severe obesity compared with men who had a normal BMI. Moreover, Strom et al. [19] observed a similar correlation between obesity and biochemical failure and clinical disease progression in 939 men treated with external beam radiation. In a Korean study, BMI was closely correlated with failure from hormone treatment after androgen deprivation therapy, and BMI was also correlated with biochemical failures after radical prostatectomy [20]. In contrast with these studies, Halabi et al. [21] observed that obesity appears to have a protective effect against overall mortality and prostate cancer-specific mortality in patients with CRPC. They hypothesized that, in a population of men with advanced prostate cancer, a lower BMI may reflect cancer cachexia and may serve as a surrogate of more aggressive disease, leading to more rapid disease progression or less effective treatment. Alternatively, obese men may have higher protein and calorie reserves, which allows them to withstand the cachexia-producing effects of advancing CRPC. In this study, men with lower BMIs completed shorter cycles of docetaxel chemotherapy. Men with prior systemic chemotherapy may have lower BMIs because of the adverse effects of systemic chemotherapy. Alternatively, men with lower BMIs may have more advanced disease and cachexia states; therefore, the adverse events of docetaxel may occur easily. This result suggests that a lower BMI is associated with discontinuation of docetaxel chemotherapy in men with CRPC. These results contrast with data reported for men with localized, hormone-sensitive disease, in whom obesity is an adverse risk factor for a variety of clinical outcomes.
This study had several limitations. First, this study was retrospective in nature. Second, the cohort was very small and heterogeneous and consisted of both chemo-naive and secondary-chemotherapy patients. Because the cohort was very small, we were unable to perform a multivariate analysis to determine predictive factors for premature discontinuation of docetaxel-based systemic chemotherapy. Third, overall median survival was lower despite the good performance status of the patients, which may have resulted from the median Gleason score of 8, which is higher than that in most series. Despite these limitations, men with a lower BMI and prior chemotherapy have greater disease progression and therefore tend to discontinue docetaxel-based systemic chemotherapy. However, a well-designed large cohort study is needed to confirm these results.
The results of our study show that prior systemic chemotherapy and a lower BMI are associated with premature discontinuation of docetaxel-based systemic chemotherapy in patients with CRPC. Continuation of docetaxel-based chemotherapy is associated with longer overall survival in patients with CRPC. However, a large cohort prospective study is needed to confirm these results.
Figures and Tables
FIG. 1
Progression-free survival (A) and overall survival (B) according to the completion of docetaxel-based systemic chemotherapy. PSA, prostate-specific antigen.

References
1. National Cancer Center. Annual report of the cancer statistics in Korea in 2008 [Internet]. 2010. cited 2012 Apr 1. Goyang: National Cancer Center;Available from: http://ncc.re.kr/manage/manage03_033_view.jsp?bbsnum=189&hSelSearch=&hTxtKeyword=¤t_page=1&cd=.
2. de Wit R. Chemotherapy in hormone-refractory prostate cancer. BJU Int. 2008. 101:Suppl 2. 11–15.
3. Tannock IF, de Wit R, Berry WR, Horti J, Pluzanska A, Chi KN, et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med. 2004. 351:1502–1512.
4. Petrylak DP, Tangen CM, Hussain MH, Lara PN Jr, Jones JA, Taplin ME, et al. Docetaxel and estramustine compared with mitoxantrone and prednisone for advanced refractory prostate cancer. N Engl J Med. 2004. 351:1513–1520.
5. Armstrong AJ, Garrett-Mayer ES, Yang YC, de Wit R, Tannock IF, Eisenberger M. A contemporary prognostic nomogram for men with hormone-refractory metastatic prostate cancer: a TAX327 study analysis. Clin Cancer Res. 2007. 13:6396–6403.
6. Halabi S, Small EJ, Kantoff PW, Kattan MW, Kaplan EB, Dawson NA, et al. Prognostic model for predicting survival in men with hormone-refractory metastatic prostate cancer. J Clin Oncol. 2003. 21:1232–1237.
7. Smaletz O, Scher HI, Small EJ, Verbel DA, McMillan A, Regan K, et al. Nomogram for overall survival of patients with progressive metastatic prostate cancer after castration. J Clin Oncol. 2002. 20:3972–3982.
8. Armstrong AJ, Garrett-Mayer E, de Wit R, Tannock I, Eisenberger M. Prediction of survival following first-line chemotherapy in men with castration-resistant metastatic prostate cancer. Clin Cancer Res. 2010. 16:203–211.
9. Pond GR, Armstrong AJ, Wood BA, Brookes M, Leopold L, Berry WR, et al. Evaluating the value of number of cycles of docetaxel and prednisone in men with metastatic castration-resistant prostate cancer. Eur Urol. 2012. 61:363–369.
10. Albert JM, Buzdar AU, Guzman R, Allen PK, Strom EA, Perkins GH, et al. Prospective randomized trial of 5-fluorouracil, doxorubicin, and cyclophosphamide (FAC) versus paclitaxel and FAC (TFAC) in patients with operable breast cancer: impact of taxane chemotherapy on locoregional control. Breast Cancer Res Treat. 2011. 128:421–427.
11. Mok TS, Ramalingam SS. Maintenance therapy in nonsmall-cell lung cancer: a new treatment paradigm. Cancer. 2009. 115:5143–5154.
12. Scher HI, Eisenberger M, D'Amico AV, Halabi S, Small EJ, Morris M, et al. Eligibility and outcomes reporting guidelines for clinical trials for patients in the state of a rising prostate-specific antigen: recommendations from the Prostate-Specific Antigen Working Group. J Clin Oncol. 2004. 22:537–556.
13. Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, et al. European Organization for Research and Treatment of Cancer. National Cancer Institute of the United States. National Cancer Institute of Canada. New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst. 2000. 92:205–216.
14. de Bono JS, Oudard S, Ozguroglu M, Hansen S, Machiels JP, Kocak I, et al. Prednisone plus cabazitaxel or mitoxantrone for metastatic castration-resistant prostate cancer progressing after docetaxel treatment: a randomised open-label trial. Lancet. 2010. 376:1147–1154.
15. Halabi S, Vogelzang NJ, Ou SS, Owzar K, Archer L, Small EJ. Progression-free survival as a predictor of overall survival in men with castrate-resistant prostate cancer. J Clin Oncol. 2009. 27:2766–2771.
16. Su LJ, Arab L, Steck SE, Fontham ET, Schroeder JC, Bensen JT, et al. Obesity and prostate cancer aggressiveness among African and Caucasian Americans in a population-based study. Cancer Epidemiol Biomarkers Prev. 2011. 20:844–853.
17. Amling CL, Riffenburgh RH, Sun L, Moul JW, Lance RS, Kusuda L, et al. Pathologic variables and recurrence rates as related to obesity and race in men with prostate cancer undergoing radical prostatectomy. J Clin Oncol. 2004. 22:439–445.
18. Freedland SJ, Aronson WJ, Kane CJ, Presti JC Jr, Amling CL, Elashoff D, et al. Impact of obesity on biochemical control after radical prostatectomy for clinically localized prostate cancer: a report by the Shared Equal Access Regional Cancer Hospital database study group. J Clin Oncol. 2004. 22:446–453.
19. Strom SS, Kamat AM, Gruschkus SK, Gu Y, Wen S, Cheung MR, et al. Influence of obesity on biochemical and clinical failure after external-beam radiotherapy for localized prostate cancer. Cancer. 2006. 107:631–639.
20. Kang SG, Yoon CY, Yoon DK. Obesity is an independent predictor of biochemical failure following radical prostatectomy and androgen deprivation therapy (ADT) for prostate cancer. Korean J Urol. 2005. 46:1262–1267.
21. Halabi S, Ou SS, Vogelzang NJ, Small EJ. Inverse correlation between body mass index and clinical outcomes in men with advanced castration-recurrent prostate cancer. Cancer. 2007. 110:1478–1484.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download