Abstract
Purpose
We compared the impact of prostate volume on oncological and functional outcomes 2 years after robot-assisted laparoscopic prostatectomy (RALP) and open radical retropubic prostatectomy (ORP).
Materials and Methods
Between 2003 and 2010, 253 consecutive patients who had undergone prostatectomy by a single surgeon were serially followed over 2 years postoperatively. RALP was performed on 77 patients and ORP on 176. The patients were divided into two subgroups according to prostate volume as measured by transrectal ultrasound: less than 40 g and 40 g or larger. Recoveries of potency and continence were checked serially by interview 1, 3, 6, 9, 12, and 24 months postoperatively.
Results
RALP was associated with less blood loss (ORP vs. RALP: 910 mL vs. 640 mL, p<0.001) but a longer operation time (150 minutes vs. 220 minutes, p<0.001) than was ORP. No statistically significant differences were found between the two groups for oncological outcomes, such as positive surgical margin (40% vs. 39%, p=0.911) or biochemical recurrence (12% vs. 7%, p=0.155). The overall functional outcomes showed no statistically significant differences at 2 years of follow-up (continence: 97% vs. 94%, p=0.103; potency: 51% vs. 56%, p=0.614). In the results of an inter-subgroup analysis, potency recovery was more rapid in patients who underwent RALP in a small-volume prostate than in those who underwent ORP in a small-volume prostate (3 months: 24% vs. 0%, p=0.005; 6 months: 36% vs. 10%, p=0.024). However, patients who underwent RALP in a large-volume prostate were less likely to recover continence than were patients who underwent ORP in a large-volume prostate (97% vs. 88%, p=0.025).
Prostate cancer (PCa) is the fastest growing cancer in Korea. According to the statistical data of the National Cancer Information Center, the incidence of PCa, 8.5 per 100,000 population in 1999, had increased to 23.1 by 2008 [1]. The annual growth rate, 13.5%, is the fastest of all cancers in Korea.
Radical prostatectomy (RP) is the standard treatment for patients with clinically localized PCa (cT1-T2) and is associated with a life expectancy of >10 years [2]. Whereas open radical retropubic prostatectomy (ORP) has been considered the gold standard for surgical treatment [3], minimally invasive procedures have been introduced with the intention of minimizing peri- and postoperative morbidities [4]. Despite the widespread use of robot-assisted laparoscopic prostatectomy (RALP) over the past decade, there are ongoing debates regarding the benefits of RALP compared with ORP [5]. Oncological controls in comparative studies have shown that RALP yields results similar to those of ORP [6]. Several comparative studies have evaluated the functional outcomes of RALP and ORP [7]. One recent study suggested that RALP results in no significant improvement in urological complications such as incontinence and erectile dysfunction [8]. However, not many studies have undertaken well-controlled, single-surgeon, direct comparisons of the outcomes of RALP and ORP.
There have in fact been some reports on the impact of prostate volume on surgical outcomes. In ORP, a large-volume prostate is associated with longer operation time and increased complications [9]. Patients with a small-volume prostate, meanwhile, have higher rates of biochemical recurrence (BCR) [10]. In RALP, a small-volume prostate is correlated with early return of potency [11]. However, there are few comparative reports on the impact of prostate volume on oncological and functional outcomes between the two types of surgery.
The aim of the present study was to investigate differences in oncological and functional outcomes according to prostate volume in patients with localized PCa who underwent ORP or RALP.
Between September 2003 and April 2010, 408 consecutive patients underwent single-surgeon RP for biopsy-confirmed PCa at Seoul National University Hospital. A total of 103 patients (25%) underwent RALP and 305 patients (75%) underwent ORP. Preliminarily, after approval from our Institutional Review Board, a total of 253 patients were included in this study. We initially selected 176 consecutive ORP and 77 RALP cases for clinically localized PCa (cT1-T2). The first 100 patients who had undergone ORP and the first 25 to undergo RALP were excluded from the analysis owing to the learning curve [3]. No patients in the study had undergone preoperative radiotherapy or neoadjuvant androgen deprivation therapy.
Postsurgery follow-up visits typically were scheduled at 3-month intervals for 1 year, and then semiannually for 1 year, and yearly thereafter. All the patients were followed up for at least 24 months. Patients within each surgical group were divided into two subgroups according to their prostate volume as measured by preoperative transrectal ultrasound: less than 40 g and 40 g or larger.
The oncological outcomes were assessed as positive surgical margin (PSM) and 24 month BCR rates. PSMs were defined as tumor cells reaching the inked surface of the specimen. BCR was defined as two consecutive prostate-specific antigen (PSA) measurements ≥0.2 ng/mL. The functional outcomes were assessed as continence and potency. Urinary continence was defined as the absence of any urinary leakage or the use of only one security pad. Potency was defined as spontaneous erectile function satisfactory for intercourse or with the use of phosphodiesterase-5 inhibitors on demand. Preoperative erectile function was assessed by use of a validated questionnaire, the International Index of Erectile Function-5 (IIEF-5). We evaluated postoperative potency in all patients who had been potent before surgery, defined as an IIEF-5 score of ≥12, and who had undergone a bilateral or unilateral nerve-sparing procedure. Postoperative potency was determined at each follow-up by means of a detailed surgeon-conducted interview.
ORP was performed by modified Walsh anatomical retropubic RP. RALP was performed by the transperitoneal antegrade approach with the use of the da Vinci Robot System (Intuitive Surgical Inc., Sunnyvale, CA, USA). The choice of surgical approach accorded with patient preference after discussion of the risks, benefits, and alternatives with the patient's physician. In both groups, a uni- or bilateral nerve-sparing procedure was performed if clinically indicated by patient age, preoperative erectile function, and oncological parameters.
The baseline characteristics of the patients were summarized as the mean standard deviation for continuous variables and frequencies or as percentages for categorical variables. The RALP and ORP groups were compared by using the Student's t-test (continuous factors) and Pearson chi-square test (categorical factors). Kaplan-Meier survival curves were compared across techniques by using the log-rank test for up to 24 months of follow-up. In all of the tests, p<0.05 was taken to indicate statistical significance. A statistical analysis was performed with the SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA).
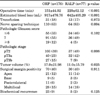
The mean patient age was 67.0±6.76 years, and the median body mass index was 24.0±2.67 kg/m2. The mean preoperative PSA level was 7.4±17.74 ng/mL. The mean preoperative transrectal ultrasound prostate volume was 42±17.92 mL. As for the patients' clinical stages, 171 cases (68%) were stage I and 82 cases (32%) were stage II. The preoperative baseline clinicopathological demographics of the ORP and RALP groups were comparable (Table 1).
Surgical and pathological parameters in the two groups are compared in Table 2. The mean operation time was significantly shorter in the ORP group (151 minutes vs. 220 minutes, p<0.001), whereas the mean estimated blood loss was significantly less in the RALP group (917 mL vs. 642 mL, p<0.001). The transfusion rate was not significantly different (18% vs. 17%, p=0.873). The number of patients who had undergone a nerve-sparing procedure (unilateral or bilateral) was significantly higher in the RALP group (63% vs. 83%, p=0.004). The pathological stages were very similar in each group, with 53% of patients with organ-confined disease in the ORP group compared with 54% in the RALP group. However, there was a significant difference in the proportion of patients with a pathologic Gleason score; the proportion was more favorable in the RALP group (p=0.008). The most common location of a PSM in the two groups was at the apex.
PSMs were encountered less often with RALP than with ORP, but without statistical significance (42% vs. 38%, p=0.394). The 2-year BCR-free survival rates were 88% (154 of 176) in ORP and 94% (72 of 77) in RALP patients during the follow-up period. A log-rank test showed no statistical difference between the two groups (p=0.140) within 2 years of follow-up (Fig. 1).
After ORP, urinary continence had been regained in 55% of patients at 1 month, 80% at 3 months, 92% at 6 months, 95% at 9 months, 96% at 12 months, and 98% at 24 months. The corresponding RALP recovery rates were 38%, 71%, 84%, 88%, 94%, and 95% (Fig. 2). After adjustment for age, operation type was not found to significantly affect postoperative urinary continence recovery (p=0.058).
Of the 177 patients who underwent ORP, 55 (31%) were potent preoperatively, compared with 41 of the 77 patients (53%) who underwent RALP. In the ORP group, nerve-sparing status was bilateral in 47 (85%) and unilateral in 8 patients (15%); the corresponding numbers in the RALP group were 33 (81%) and 8 (19%), respectively. In the subset of potent patients, 28 of 55 (51%) treated with ORP and 23 of 41 (56%) treated with RALP were potent at the 2-year follow-up. The recovery rates after ORP were 2% at 1 month, 6% at 3 months, 15% at 6 months, 22% at 9 months, 40% at 12 months, and 51% at 24 months; after RALP, they were 0%, 17%, 29%, 29%, 54%, and 56%, respectively (Fig. 2). After adjustment for age and nerve-sparing status, the recovery of sexual function was comparable between the ORP and RALP groups throughout the follow-up period (p=0.418).
In the subgroup analysis for which patients were classified according to prostate volume into small (<40 g) and large (≥40 g) volume groups, in the ORP small-volume subgroup, the potency rates were 0% at 1 month, 0% at 3 months, 10% at 6 months, 21% at 9 months, 35% at 12 months, and 55% at 24 months. In the RALP small-volume subgroup, they were 0%, 24%, 36%, 36%, 56%, and 60%, respectively (Fig. 3). RALP was associated with quick potency recovery in the small-volume subgroup (p=0.020). Between the two small-volume subgroups, there was no significant difference in the time to continence or oncological outcomes. Within the large-volume subgroups, patients who had undergone RALP were less likely to become continent than were those who had undergone ORP (p=0.048). In the ORP large-volume subgroup, the continence rates were 57% at 1 month, 77% at 3 months, 91% at 6 months, 95% at 9 months, 95% at 12 months, and 97% at 24 months. In the RALP large-volume subgroup, they were 31%, 56%, 75%, 81%, 88%, and 91%, respectively (Fig. 4). Between the two large-volume subgroups, there was no significant difference in the recovery of sexual function or oncological outcomes.
In the present study we compared the surgical, oncological, and functional outcomes of ORP and RALP. Whereas the study was not randomized, its main strengths were the single-center and single-surgeon setting; the use of a validated questionnaire to evaluate preoperative erectile function, specifically, the IIEF-5; and the inclusion of consecutive patients. The same protocols for preoperative diagnosis and staging evaluation of PCa, perioperative treatment, pathological evaluation, and surgical approaches were adopted for both study groups, and the follow-up periods were sufficiently long for evaluation of functional outcomes. Another strength of the methodology was the comparability of the baseline clinicopathologic characteristics between the two groups.
Oncological outcomes did not differ significantly between the two groups. BCR and PSM are the two commonly used indexes for assessment of oncological outcomes following RP [3]. In the present study, the PSM rates were similar in the two groups, and consistent with other, prior series. The reported incidences of PSM ranged from 11% to 37% after ORP and from 9.6% to 26% after RALP [12]. Although more nerve-sparing procedures were performed in the RALP group, the technique did not significantly increase the incidence of adverse outcomes. The difference in the short-term BCR rates between the two groups was not statistically significant. Schroeck et al. [13] and Krambeck et al. [14] also reported similar BCR rates for RALP and ORP groups at short follow-ups of 1 and 3 years, respectively. Sooriakumaran et al. [15] recently reported that biochemical-free survival after RALP was 84.8% at a median follow-up of 6.3 years. Long-term outcome data on PSA progression are not yet available for RALP, owing to the relatively short history of their availability [16]. Further follow-up is required to determine long-term oncological outcomes such as disease-specific death and overall survival.
In the present study, the recovery of erectile function was more rapid in RALP patients with small-volume prostates. We found a significant advantage of RALP over ORP for those who had small-volume prostates at the 3- and 6-month follow-up, particularly for preoperatively potent patients (IIEF-5≥12) undergoing unilateral or bilateral neurovascular bundle sparing. Our postoperative potency rates were 24% after RALP and 0% after ORP at the 3-month follow-up (p=0.007), and 36% and 10% at the 6-month (p=0.026), respectively. However, there was no difference in potency rates between the RALP and ORP small-volume groups at 12 months (56% vs. 35%, p=0.095) or 24 months (60% vs. 55%, p=0.468) postoperatively. Neither was there any statistical difference in recovery of erectile function between the two large-volume groups. Tewari et al. [5] reported that patients after RALP had a more rapid return of erection: 50% at a mean follow-up of 180 days versus 440 days after ORP. Rocco et al. [17] reported a significant RALP advantage over ORP for patients, particularly younger patients, who had undergone a nerve-sparing procedure at 3, 6, and 12 months postoperatively. However, Krambeck et al. [14] reported no significant difference in potency rate at the 1-year follow-up. This early return of erectile function could be attributed to preservation of potency with minimized damage to the neurovascular bundles, better magnified visualization, precise anatomical dissection, reduced blood loss, or improved anatomical-reconstruction ability by use of robotic assistance [18]. It has been postulated that in larger prostates, the neurovascular bundles are displaced posteriorly, where they are possibly obscured by the prostate, making them prone to injury [19]. Also, a large prostate is less mobile in the pelvis, owing to the smaller available space [20]. These factors could offset the advantage of RALP for potency preservation.
In the present findings, there were no pronounced advantages to RALP for continence. Interestingly, patients with large-volume prostates seemed to recover continence more quickly after ORP than after RALP. Menon et al. [21] found that 84% of patients were continent at the 12 month follow-up after RALP. Hu et al. [8] reported that men undergoing RALP were more likely to be diagnosed as incontinent. Malcolm et al. [22] found no difference in health-related quality-of-life "bother scores" related to incontinence. Krambeck et al. [14] reported no difference in continence after RALP or RRP at the 1-year follow-up. Others, meanwhile, have reported 12 month urinary continence rates as high as 97% after RALP. Our findings are interesting in light of the fact that RALP is thought to increase the precision of anastomosis and decrease the incidence of traumatic maneuvers on the urethrosphincteric complex [23]. We suspect that these outcomes are related to a combination of extensive apical dissection and overzealous diathermy at the bladder neck with over-tight suturing [24], though we have no direct evidence for this. This difference might be attributable to the necessarily lengthy learning curve for making a running anastomosis compared with the interrupted anastomosis used for ORP [14]. Or, it might also be due to the differences between the retrograde and antegrade approaches [17]. In any case, there is no real explanation for such findings at the present time.
The main limitation of this study, a retrospective review of our database, was the lack of randomized allocation of patients into one of the two treatment arms. The choice of surgical approach was based mainly on patient preferences and requests after they were fully informed about both procedures. This is a potential source of bias in the present study. Still, given that these groups were relatively well matched regarding the comparability of the patients' baseline characteristics, the substantial differences in functional outcomes shown in the present results can be attributed mainly to the two different surgical approaches. Another concern is that because the patients underwent RP at a tertiary-care centre, the present study might not fully reflect epidemiological trends and, indeed, might have incorporated a certain degree of selection bias. The other limitations of this study were the relatively small number of patients and the short follow-up period.
In this single-surgeon consecutive series, patients after RALP demonstrated early recovery of erectile function, especially those with small-volume prostates. RALP was also associated with lower blood loss but slightly longer operation times when compared with ORP. The short-term oncological outcomes between the two groups seemed to be equivalent. A large-volume prostate was associated with lower rates of postoperative urinary continence recovery, particularly in RALP patients. Long-term follow-up and well-designed randomized controlled trials are required before definitive conclusions on oncological and functional outcomes between ORP and RALP can be drawn.
Figures and Tables
 | FIG. 1Kaplan-Meier biochemical recurrence-free probability by operation type. Black lines indicate robot-assisted laparoscopic prostatectomy, dotted lines indicate open radical retropubic prostatectomy. |
 | FIG. 2Cumulative incidence by operation type. (A) Continence, (B) potency. Black lines indicate robot-assisted laparoscopic prostatectomy, dotted lines indicate open radical retropubic prostatectomy. |
 | FIG. 3Cumulative incidence of continence by prostate volume. (A) <40 g, (B) ≥40 g. Black lines indicate robot-assisted laparoscopic prostatectomy (RALP), dotted lines indicate open radical retropubic prostatectomy (ORP). The incidences of continence at each time point were compared by use of the Pearson chi-square test. |
 | FIG. 4Cumulative incidence of potency by prostate volume. (A) <40 g, (B) ≥40 g. Black lines indicate robot-assisted laparoscopic prostatectomy (RALP), dotted lines indicate open radical retropubic prostatectomy (ORP). The incidences of potency at each time point were compared by use of the Pearson chi-square test. |
TABLE 1
Preoperative characteristics of the patients

Values are presented as mean±standard deviation or number (%).
PSA, prostate-specific antigen; TRUS, transrectal ultrasound; IIEF, International Index of Erectile Function.
a:Patients who had been potent before surgery, defined as an IIEF-5 score of ≥12, and who had undergone a bilateral or unilateral nerve-sparing procedure.
References
1. National Cancer Information Center [Internet]. c2011. cited 2012 May 2. Goyang (KR): National Cancer Information Center;Available from: http://www.cancer.go.kr/ncic/.
2. Fracalanza S, Ficarra V, Cavalleri S, Galfano A, Novara G, Mangano A, et al. Is robotically assisted laparoscopic radical prostatectomy less invasive than retropubic radical prostatectomy? Results from a prospective, unrandomized, comparative study. BJU Int. 2008. 101:1145–1149.
3. Finkelstein J, Eckersberger E, Sadri H, Taneja SS, Lepor H, Djavan B. Open versus laparoscopic versus robot-assisted laparoscopic prostatectomy: the European and US experience. Rev Urol. 2010. 12:35–43.
4. Duffey B, Varda B, Konety B. Quality of evidence to compare outcomes of open and robot-assisted laparoscopic prostatectomy. Curr Urol Rep. 2011. 12:229–236.
5. Tewari A, Srivasatava A, Menon M. Members of the VIP Team. A prospective comparison of radical retropubic and robot-assisted prostatectomy: experience in one institution. BJU Int. 2003. 92:205–210.
6. Ficarra V, Cavalleri S, Novara G, Aragona M, Artibani W. Evidence from robot-assisted laparoscopic radical prostatectomy: a systematic review. Eur Urol. 2007. 51:45–55.
7. Ficarra V, Novara G, Fracalanza S, D'Elia C, Secco S, Iafrate M, et al. A prospective, non-randomized trial comparing robot-assisted laparoscopic and retropubic radical prostatectomy in one European institution. BJU Int. 2009. 104:534–539.
8. Hu JC, Gu X, Lipsitz SR, Barry MJ, D'Amico AV, Weinberg AC, et al. Comparative effectiveness of minimally invasive vs open radical prostatectomy. JAMA. 2009. 302:1557–1564.
9. Hsu EI, Hong EK, Lepor H. Influence of body weight and prostate volume on intraoperative, perioperative, and postoperative outcomes after radical retropubic prostatectomy. Urology. 2003. 61:601–606.
10. D'Amico AV, Whittington R, Malkowicz SB, Schultz D, Tomaszewski JE, Wein A. A prostate gland volume of more than 75 cm3 predicts for a favorable outcome after radical prostatectomy for localized prostate cancer. Urology. 1998. 52:631–636.
11. Ahlering TE, Kaplan AG, Yee DS, Skarecky DW. Prostate weight and early potency in robot-assisted radical prostatectomy. Urology. 2008. 72:1263–1268.
12. Ficarra V, Novara G, Artibani W, Cestari A, Galfano A, Graefen M, et al. Retropubic, laparoscopic, and robot-assisted radical prostatectomy: a systematic review and cumulative analysis of comparative studies. Eur Urol. 2009. 55:1037–1063.
13. Schroeck FR, Sun L, Freedland SJ, Albala DM, Mouraviev V, Polascik TJ, et al. Comparison of prostate-specific antigen recurrence-free survival in a contemporary cohort of patients undergoing either radical retropubic or robot-assisted laparoscopic radical prostatectomy. BJU Int. 2008. 102:28–32.
14. Krambeck AE, DiMarco DS, Rangel LJ, Bergstralh EJ, Myers RP, Blute ML, et al. Radical prostatectomy for prostatic adenocarcinoma: a matched comparison of open retropubic and robot-assisted techniques. BJU Int. 2009. 103:448–453.
15. Sooriakumaran P, Haendler L, Nyberg T, Gronberg H, Nilsson A, Carlsson S, et al. Biochemical recurrence after robot-assisted radical prostatectomy in a European single-centre cohort with a minimum follow-up time of 5 years. Eur Urol. 2012. 62:768–774.
16. Rozet F, Jaffe J, Braud G, Harmon J, Cathelineau X, Barret E, et al. A direct comparison of robotic assisted versus pure laparoscopic radical prostatectomy: a single institution experience. J Urol. 2007. 178:478–482.
17. Rocco B, Matei DV, Melegari S, Ospina JC, Mazzoleni F, Errico G, et al. Robotic vs open prostatectomy in a laparoscopically naive centre: a matched-pair analysis. BJU Int. 2009. 104:991–995.
18. Tewari A, Peabody JO, Fischer M, Sarle R, Vallancien G, Delmas V, et al. An operative and anatomic study to help in nerve sparing during laparoscopic and robotic radical prostatectomy. Eur Urol. 2003. 43:444–454.
19. Zorn KC, Orvieto MA, Mikhail AA, Gofrit ON, Lin S, Schaeffer AJ, et al. Effect of prostate weight on operative and postoperative outcomes of robotic-assisted laparoscopic prostatectomy. Urology. 2007. 69:300–305.
20. Link BA, Nelson R, Josephson DY, Yoshida JS, Crocitto LE, Kawachi MH, et al. The impact of prostate gland weight in robot assisted laparoscopic radical prostatectomy. J Urol. 2008. 180:928–932.
21. Menon M, Tewari A, Baize B, Guillonneau B, Vallancien G. Prospective comparison of radical retropubic prostatectomy and robot-assisted anatomic prostatectomy: the Vattikuti Urology Institute experience. Urology. 2002. 60:864–868.
22. Malcolm JB, Fabrizio MD, Barone BB, Given RW, Lance RS, Lynch DF, et al. Quality of life after open or robotic prostatectomy, cryoablation or brachytherapy for localized prostate cancer. J Urol. 2010. 183:1822–1828.
23. Abbou CC, Salomon L, Hoznek A, Antiphon P, Cicco A, Saint F, et al. Laparoscopic radical prostatectomy: preliminary results. Urology. 2000. 55:630–634.
24. Joseph JV, Vicente I, Madeb R, Erturk E, Patel HR. Robot-assisted vs pure laparoscopic radical prostatectomy: are there any differences? BJU Int. 2005. 96:39–42.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download