Abstract
Infection stones are more likely to form after urinary diversion as the result of urinary stasis. To prevent urinary stasis due to encrusted pyelitis in a transplanted kidney, we describe an alternative a surgical treatment: ileo-pelvic anastomosis. In our patient with a transplanted kidney, the ileal conduit had previously been anastomosed end-to-side owing to renal tuberculosis with an atrophied bladder; the transplanted ureter was anastomosed to the ileum in the left lower abdomen with an ileal conduit on the opposite side. Routine check-up revealed hydronephrosis with infected pyelitis and ureteritis in the transplanted kidney. We performed ileo-pelvic end-to-end anastomosis to prevent urinary stasis by lengthening the ileal conduit and performed augmentation cystoplasty to support the atrophied bladder following tuberculosis. We suggest that this approach may be useful in similar cases.
Encrusted pyelitis is characterized by mucosal inflammation and encrustations of the upper urinary tract. Such encrustations consist of deposits of ammonium magnesium phosphate and struvite. Corynebacterium urealyticum, a gram-positive bacillus, has been identified as the most frequent causative pathogen.
Urinary stasis is highly likely to contribute to stone formation, because large-scale spontaneous precipitation of crystals occurs when a critical concentration (e.g., supersaturation) is exceeded. Ileal conduits encourage stone formation, because they are prone to urinary stasis [1].
Failed treatment of encrusted pyelitis in a transplanted kidney can cause graft failure or nephrectomy. To overcome urinary stasis with encrusted pyelitis in a transplanted kidney, we report surgical treatment by ileo-pelvic anastomosis without nephrectomy. In addition, in this case, augmentation cystoplasty was performed to strengthen the atrophied bladder following tuberculosis.
A 51-year-old female patient received a kidney from her sister after a double nephrectomy owing to renal tuberculosis 12 years previously. At that time, the transplanted ureter was anastomosed to the ileum in the left lower abdomen with an ileal conduit on the opposite side. Ureteroileal anastomosis was performed by using 2 sutures of 3-0 Vicryl. The patient experienced no problems for 12 years. At a routine checkup, she complained of abdominal pain, gross hematuria, and increased debris in the ileal conduit. Her serum creatinine was elevated to 1.7 mg/dL (normal, 0.6 to 1.1 mg/dL), and her transplanted kidney developed hydronephrosis with calcified debris observed by sonography (Fig. 1). Neither hydronephrosis nor calcified debris had been observed 6 months before in a routine outpatient checkup.
Proteus mirabilis and Pseudomonas aeruginosa were detected by urine culture. Abdominopelvic computed tomography revealed hydronephrosis with encrusted pyelitis and ureteritis in the transplanted kidney (Fig. 2).
The patient was treated by percutaneous nephrostomy and empirical antibiotics. Microorganisms in the urine showed no evidence of tuberculosis. A cystogram showed that the bladder was not refluxed but had a small capacity (50 mL).
After 3 weeks, we operated to anastomose the transplanted renal pelvis to one end of the ileal conduit, performing augmentation cystoplasty with new ileum and to anastomosis the other end of the remnant ileum with the augmented bladder. Augmentation cystoplasty is a reconstructive technique for creating a compliant, large-capacity urinary storage unit to protect the upper urinary tract.
The operation was performed via a midline incision. Because it was difficult to approach the major calices of the transplanted kidney in the left pelvic rim, we anastomosed one end of the ileal conduit to the pelvis of the transplanted kidney in an end-to-end fashion. The ileal conduit was lengthened by 30 cm to extend from the pelvis to the augmented bladder chimney. The encrusted upper ureter of the transplanted kidney was retained. We observed that the encrusted ureteritis involved the entire upper ureter. Bladder atrophy was remarkable, with only the trigon portion remaining. After exposure of the urinary bladder, a transverse wide V-shaped cystostomy incision was created, with the apex approaching the anterior bladder neck and the base extending posteriorly past the midcoronal plane of the bladder dome. A 20 cm segment of new ileum at least 15 cm proximal to the ileocecal junction was used for ileocystoplasty. For the small bowel, a V-shaped plate was created by a side-to-side anastomosis with 2-0 Vicryl. A circumferential, continuous, full-thickness, single layer anastomosis of the bowel to the bladder was started posteriorly by using 2-0 braided absorbable sutures. Bladder drainage was maintained with a 24 French urethral catheter. The other end of the ileal conduit was anastomosed through small separate ileotomies (1.5 cm length) in the limb of the augmentation cystoplasty.
After surgery, calcified debris was decreased and encrusted pyelitis was absent on sonography. The patient's creatinine level was also normalized on follow-up. A follow-up cystogram showed increased bladder capacity to approximately 300 mL with well-preserved end-to-end anastomosis of the ileo-pelvic portion with the other end of one chimney of augmentation cystoplasty with the elongated ileal conduit (Figs. 3, 4).
Infection stones composed of struvite apatite account for 15% of urinary stone disease. The most common causative agent in the formation of infection stones is a urease-positive urinary tract infection. Urease is necessary for splitting urea into ammonia to form alkaline urine. Such infections need to be treated to avoid kidney damage.
Less invasive methods are preferable to preserve the connection between the renal pelvis and the upper ureter. Ileo-pelvic anastomosis must be adjusted for patients with infection stones in the upper urinary tract after renal transplantation. An alternative way to prevent these infection stones is to ensure a wider pathway through a ureter that has been narrowed in places by these stones [2].
According to a report on the incidence of urolithiasis in cystectomy patients, 5 of 78 patients who had undergone diversion with an intestinal conduit developed urolithiasis, all in the upper tract. In contrast, 4 of 78 patients who had received a diversion had a renal stone at the time of presentation. Refluxing urine may contribute to an increased risk of stone formation after urinary diversion, whereas pouch stasis may contribute to stone formation in the diversion group.
A case of failed treatment of encrustation in a kidney transplant recipient was reported and graft removal was performed after 6 months of failed management owing to intractable febrile urinary tract infections that became life threatening. Encrusted pyelitis must be diagnosed rapidly and requires, if possible, conservative management. Nevertheless, kidney loss can occur in transplant recipients [3].
In a case similar to ours, Benoit et al. [4] reported on their efforts to salvage a transplanted kidney with encrusted pyelitis. They excised renal parenchyma from the caudal portion of the inferior calyx, which was then anastomosed to the ileostomy. In their case, bladder capacity was within the normal limit; thus, augmentation cystoplasty was not indicated.
In conclusion, if urinary tract infection is controlled, we suggest that ileo-pelvic anastomosis [5] combined with augmentation cystoplasty [6,7] is an alternative for the treatment of encrusted pyelitis with atrophied bladder. In our patient, we performed ileo-pelvic anastomosis to prevent urinary stasis by elongating the ileal conduit. In addition, the augmentation cystoplasty technique is useful for increasing bladder capacity that has been diminished by renal tuberculosis (Fig. 5).
Figures and Tables
FIG. 1
Preoperative ultrasonography revealed multiple infection stones with hydronephrosis in left transplanted kidney.
FIG. 2
Abdominopelvic computed tomography revealed hydronephrosis with encrusted pyelitis and ureteritis in transplanted kidney.

FIG. 3
Postoperative ultrasonography scan showing that calcified debris was decreased, encrusted pyelitis was absent, and hydronephrosis was improved.
FIG. 4
Postopearative cystogram shows no leakage and remnant ileum with the transplanted kidney anastomosed with augmented bladder. Bladder capacity is increased from 50 to 300 mL, a capacity near the normal limit.
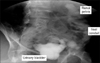
FIG. 5
(A) Fifty-one-year-old female patient had renal tuberculosis 12 years before. (B) The patient had double nephrectomy with transplanted ureter was anstomosed ileum end to side. (C) Routine check-up revealed hydronephrosis with infected pyelitis and ureteritis in transplanted kidney. (D) We performed ileo-pelvic end-to end anastomosis to prevent urinary stasis by lengthening ileal conduit, and performed augmentation cystoplasty to support the atrophied bladder following tuberculosis.

References
1. Parmar MS. Kidney stones. BMJ. 2004. 328:1420–1424.
2. Wong HY, Riedl CR, Griffith DP. Coe FL, Favus MJ, Pak CYC, Parks JH, Preminger GM, editors. Medical management and prevention of struvite stones. Kidney stones: medical and surgical management. 1996. Philadelphia: Lippincott-Raven;941–950.
3. Meria P, Margaryan M, Haddad E, Dore B, Lottmann HB. Encrusted cystitis and pyelitis in children: an unusual condition with potentially severe consequences. Urology. 2004. 64:569–573.
4. Benoit G, Eschwege P, Paradis V, Droupy S, Nordmann P, Charpentier B. Successful treatment of encrusted pyelitis in a renal transplant with local acidification and surgical ileocaliceal anastomosis. J Urol. 1999. 162:1369–1370.
5. Stein RJ, Turna B, Patel NS, Weight CJ, Nguyen MM, Shah G, et al. Laparoscopic assisted ileal ureter: technique, outcomes and comparison to the open procedure. J Urol. 2009. 182:1032–1039.
6. Gupta NP, Kumar A, Sharma S. Reconstructive bladder surgery in genitourinary tuberculosis. Indian J Urol. 2008. 24:382–387.
7. Lee SS, Kang WG, Huh K, Kim DW, Kim GH, Shin YH, et al. Dysfunctional contracted bladder in renal transplantation. J Korean Soc Transplant. 2007. 21:257–261.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download