Abstract
Purpose
Parental decisions about the treatment of nocturnal enuresis (NE) are generally based on silent agreement with a physician's recommendation. However, physicians may have an insufficient understanding about parents' concerns and expectations regarding treatment. The aim of this study was to clarify the discrepancies between the perceptions of parents and physicians and to better understand the attitudes related to NE treatment.
Materials and Methods
A survey was conducted in six centers and included 105 parents and 102 physicians. Two questionnaires, one for parents and another for physicians, were prepared. Each contained items on demographic characteristics, concerns, and NE treatment preferences. The parents completed the questionnaire during their child's first clinical visit, and the physicians completed the questionnaire via e-mail or individual interviews.
Results
Low self-esteem was the most common concern among both parents and physicians. Parents showed a more serious concern regarding disease progression and sequelae than did physicians. In the parent group, parents of younger children were mainly concerned about growth, whereas parents of children with daytime symptoms were mainly concerned about disease progression and relationships. Treatment outcome preferences differed significantly between the two groups. Physicians preferred treatments yielding immediate results, whereas parents preferred long-term treatments that would result in low recurrence.
Enuresis is a condition involving intermittent nocturnal incontinence during sleep and can be categorized as monosymptomatic or nonmonosymptomatic [1]. Nocturnal enuresis (NE) is common, with a prevalence of 20% in 5-year-old children and of up to 2% in adults [2]. NE is a bothersome and distressing disorder in enuretic children. Enuresis negatively affects the self-esteem, interpersonal relationships, and social performance of affected children and their families; moreover, enuretic children with daytime symptoms have particularly diminished self-esteem [3-5]. Meydan et al. [6] conducted a survey and reported that the quality of life of mothers of enuretic children is negatively affected; they have low general health concepts and high anxiety and depression scores. These effects may lead parents to seek medical advice and treatment for their enuretic children. However, mothers preferred management strategies such as lifting, water restriction, regular voiding, and rewards rather than treatment interventions such as medication, alarm use, hypnosis, and physician advice [3,7-9].
Although concerns about and treatment modalities for NE have been introduced and applied, few studies have examined the concerns and attitudes of parents and physicians regarding this condition and its treatment. The aim of this study was to identify and compare the perspectives of parents and physicians on enuresis and its treatment to provide physicians with information regarding the management of enuresis.
The parent participants were recruited during their enuretic child's first visit to an outpatient clinic, and the physicians were recruited via e-mail or by visiting researchers. This investigation was conducted in six centers between September 2009 and March 2010. The survey consisted of two questionnaires: one for the parents of children with NE and the other for clinically practicing physicians.
The parents were asked to complete the questionnaire, which requested demographic information including the parent's age, education level, work status, and the nature of symptoms such as enuresis severity and the presence of daytime symptoms. The physicians were additionally asked for basic information regarding their work environment, length of clinical career, and number of enuretic patients seen per week. Both groups answered three common questions. The first common question regarding therapeutic motives consisted of six sub-questions with "yes" or "no" as the possible answers, which focused on enuresis concerns including disease progression, urologic sequelae, interpersonal relationship difficulties, self-esteem, and growth retardation. The second common question asked participants to rate their treatment outcome preferences on a digital scale ranging from 1 to 5, where 1 indicates a treatment providing quick relief of enuresis even if it has a high relapse rate, and 5 indicates a treatment providing a low relapse rate even if the onset of enuresis relief is slow. The third common question asked participants to choose one of the following treatment modalities for enuretic children: wait and see, counseling on drinking and voiding habits, pharmacotherapy, alarm therapy, combination drug/alarm therapy, psychotherapy, or decisions made by physicians or parents of enuretic children (appendix).
The quantitative results are presented as mean±standard deviation. Student's t-test and the chi-square test were used to compare single variables between parents and physicians and the relationships between variables within each group, respectively. The level of statistical significance was set at p<0.05. When comparing the motives for NE treatment between parents and physicians and between variables in the parents' group, we performed Bonferroni corrections for multiple testing; therefore, the significance level in these cases was p<0.0083 after adjustment according to the Bonferroni formula Pbonf=n×Pobserved.
The demographic characteristics of the parents and physicians are shown in Table 1. A total of 105 parents were included. The mean ages of the enuretic children, mothers, and fathers were 8.2, 37.6, and 40.3 years, respectively. All parents had a minimum of a high school education, and 32.4% of them indicated that they were part of a working couple. A total of 102 physicians participated in the survey; 37% had clinical careers of 10 years or longer, and 81.4% worked in metropolitan areas. The proper time to start NE treatment was identified to be 5 years of age by 37% of the parents and 64% of the physicians.
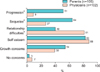
The main concerns of the parents seeking medical advice for their children's enuresis were low self-esteem (83%), urologic sequelae (64%), growth retardation (54%), disease progression (51%), and interpersonal relationship difficulties (40%). For the physicians, the main concerns motivating treatment decisions were low self-esteem (88%), interpersonal relationship difficulties (81%), growth retardation (39%), urologic sequelae (27%), and disease progression (9%). Whereas the physicians tended to be more concerned about interpersonal relationship difficulties, the parents were significantly more concerned about disease progression and urologic sequelae (p<0.001) (Fig. 1).
With regard to the concerns about seeking medical advice, parents of children younger than 10 years were more concerned about growth retardation than were the parents of the older children (62.9% vs. 34.3%, p=0.007). Although these parents were less concerned about sequelae than were the parents of older children, the difference was not significant (p=0.018). In addition, the parents whose children had daytime symptoms tended to be more concerned about disease progression and interpersonal relationship difficulties than did the parents of children without daytime symptoms, but the differences were statistically insignificant (46.5% vs. 25.8% for disease progression and 62.8% vs. 40.3% for relationship difficulties, p=0.03 and p=0.037, respectively). Parents of children with severe bedwetting problems were more concerned about sequelae (p=0.003). Parents with lower incomes tended to be more concerned about interpersonal relationship difficulties than did those with higher incomes, but the difference was statistically insignificant (p=0.045). The parents' ages (<35, 36.45, and >46 years), monthly incomes, work status (single vs. dual income), and education levels (high school vs. university) were not significantly different.
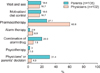
To determine the parents' treatment outcome preferences for enuresis, we asked them to rate their preferences on a digital scale from 1 to 5. The mean scores for the physicians and parents were <0.64 and 4.17, respectively (p<0.05). Whereas 49% of the physicians reported that they preferred treatments providing a quick reduction of nighttime bedwetting, even if the relapse rate was high (score of 1 or 2), over treatments with a low relapse rate (18%; score of 4 or 5), 74% of the parents preferred treatments with low relapse rates, even if the onset of enuresis relief was slow, over treatments providing quick results (4%) (Fig. 2). However, the preferences of parents did not differ with respect to the child's age, the severity of enuresis, and daytime symptoms or the parents' age, education level, work status, or monthly income.
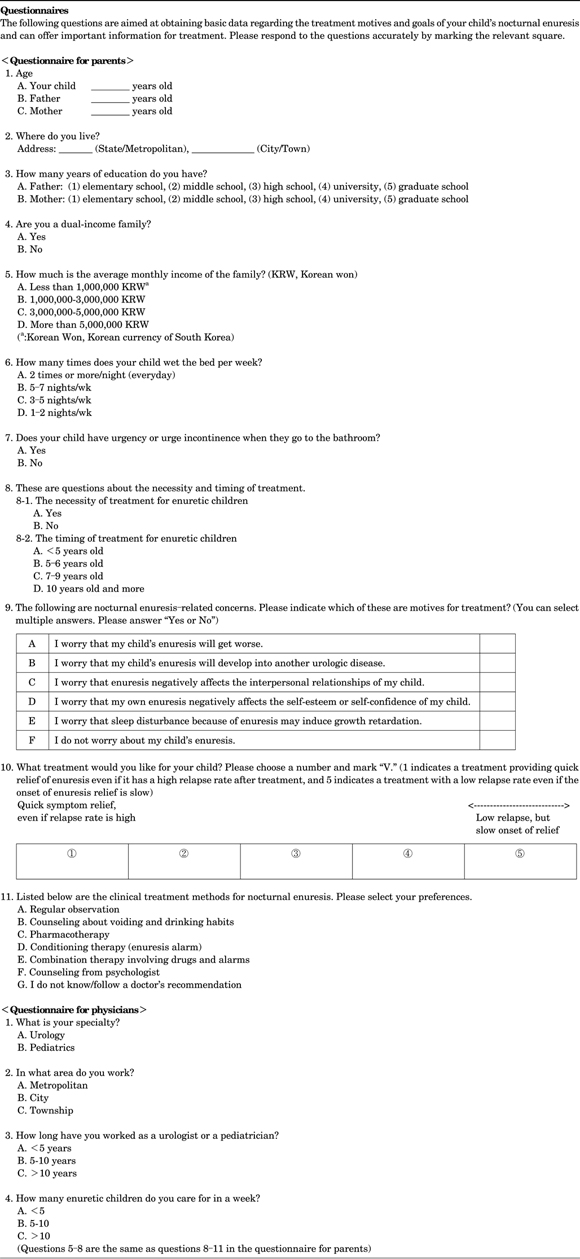
The parents' preferences for treatment modalities were physician's recommendations (31.4%), pharmacotherapy (27.1%), wait and see (18.6%), and behavioral therapy (18.6%). Meanwhile, physicians actually adopted pharmacotherapy in 61% of cases and alarm therapy in 6.9% of cases (Fig. 3), whereas their preferences regarding treatment modalities were pharmacotherapy in 33% of cases and a combination of drug and alarm therapy in 29% of cases.
NE is classified as primary or secondary and as monosymptomatic or nonmonosymptomatic according to daytime voiding symptoms. The major pathogenetic mechanisms contributing to NE include nocturnal polyuria, detrusor overactivity, and increased arousal threshold, although this is not clearly understood. Accordingly, pharmacotherapy, enuresis alarm therapy, and anticholinergics have been widely used to treat NE along with general lifestyle advice. However, the treatment strategies for enuretic children might be determined according to the opinions of physicians rather than those of the parents or children. Although NE usually disappears spontaneously with age, it continues in up to 2% of adults [2]. As mentioned earlier, NE has potentially negative emotional, social, and behavioral effects on affected children and their families [5,10-12]. These considerations may lead parents to seek medical advice and physicians to engage in the treatment of these children.
Studies in the general population have shown that more than half of parents of enuretic children do not seek professional medical advice. A very low proportion of parents are concerned about the future development of their children, whereas 50% to 97% are very concerned about enuresis itself [13-18]. A lack of knowledge regarding the nature of enuresis and its negative effect on their children can cause parents to delay seeking medical advice. However, previous studies and our study are not comparable because of differences between the study subjects. Nevertheless, the results of the current study indicate that more than 90% of parents and physicians approached NE treatment because of concerns, although the actual concerns differed between the two groups. The most common concern in both groups was low self-esteem. While physicians considered interpersonal relationship difficulties when making treatment decisions more often than did the parents, the parents were more concerned about urologic sequelae and disease progression. Growth retardation and urologic sequelae were more prevalent concerns in parents with younger children and children with severe enuresis, respectively. Thus, the results suggest that parents may actually be more concerned about long-term enuresis complications than physicians. Korean parents tend to act rashly to achieve favorable outcomes from disease treatment, whereas Korean physicians often do not spend enough time with patients because of medical infrastructure limitations and patients' needs. Therefore, regarding treatment outcome preferences, we expected the parents of enuretic children to prefer strategies that immediately address symptoms and the physicians to prefer treatments that decrease recurrence in the long term. However, the results indicate the opposite: the physicians tended to prefer "quick fix" or "middle-of-the-road" NE treatments, whereas the parents preferred long-term treatments with a low risk of NE relapse.
Several studies report that enuresis is negatively associated with risk factors related to children such as age, sex, enuresis severity, daytime symptoms, and encopresis as well as those related to parents, such as age, family income, education level, family size, professional status, and employment status [19-21]. However, this study did not focus on risk factors but aimed to compare the motives and goal preferences for NE treatment between physicians and parents. Except for enuresis severity and patient age, the baseline characteristics of parents or patients did not influence motives or treatment outcome preferences. This lack of influence may have resulted because the highly educated middle-class status of most parents facilitated access to information regarding enuresis and their child's nocturnal bedwetting caused them considerable distress, surpassing other characteristic factors. Similarly, physician characteristics such as career length, work environment, or the number of enuretic patients seen per week did not influence the therapeutic preferences.
In general, behavioral therapy, enuresis alarm therapy, and pharmacologic therapy are conventional NE treatments. However, evidence supporting NE treatment efficacy is weak, except for enuresis alarms, desmopressin, and imipramine [1,22]. According to the International Children's Continence Society, enuresis alarms and desmopressin are recommended as first-line NE therapies for monosymptomatic enuresis [1]. Desmopressin is safe and acts quickly, especially on nocturnal polyuric enuresis, but does not cure the disorder and results in a high relapse rate [23-25]. Enuresis alarms support dryness in approximately two-thirds of children with enuresis and result in low relapse rates after successful therapy; however, long-term therapy is required to achieve complete success [1,26]. A review of Korean studies on alarm treatment revealed that only 1.6% (4 of 225) of enuretic children used alarm therapy and just 0.4% of Korean physicians prescribed alarm therapy as a first-line therapy [27,28]. Jang et al. [4] state that low rates of alarm therapy may be explained by slow progress, a small initial effect, alarm device failure, a lack of understanding, and physicians' inexperience with alarms compared with pharmacotherapy. We asked the parents and physicians which treatments they would actually choose. The physicians chose pharmacotherapy as a first-line NE treatment option, which is consistent with their treatment outcome preferences (rating of 1 or 2 on the digital scale). The parents did not have strong therapeutic preferences; 31.4% of parents simply followed their physicians' recommendations, which went against their preference for low-relapse outcomes (rating of 4 or 5 on the digital scale). In addition, 61% of the physicians prescribed pharmacotherapy and 8% prescribed alarm/drug combination therapy in clinical practice. However, when describing ideal first-line treatments, only 33% selected pharmacotherapy and 29% selected alarm/drug combination therapy. These discrepancies between practices and beliefs may have resulted because of the clinical factors mentioned previously. The discrepancy between preferences for treatment outcomes and treatment modalities in parents suggests that the parents may not have fully understood the clinical processes and outcomes of each therapeutic modality or may have had information regarding the requirements for successful alarm therapy. Parents may be passively involved in decisions regarding their child's healthcare because of these limitations.
Taken together, the current finding suggest that physicians need to thoroughly consider the concerns and treatment outcome preferences of parents of enuretic children and provide detailed explanations regarding the clinical process of NE and the course of the planned treatment to actively involve both parents and children in treatment planning.
This study had some limitations, including an incomplete representation of Korean physicians and parents of enuretic children and potential interviewer bias. In addition, the questionnaire was not formally validated, and some descriptive data could not be statistically analyzed. Although the questions regarding treatment outcome preferences were limited because they imply concepts of onset time of therapeutic response and recurrence after treatment, we adopted a connotative concept in order to compare conflicting treatment strategies. Despite these limitations, the current investigation provides valuable insight into the concerns and attitudes of parents and physicians regarding NE and its treatment.
The concerns and antithetic polarization of treatment outcome preferences differ between parents and physicians. Compared with physicians, parents focus on the possible long-term complications of enuresis and prefer treatments with low relapse rates. Physicians should communicate effectively with parents and consider their NE treatment preferences during clinical decision making.
Figures and Tables
References
1. Neveus T, Eggert P, Evans J, Macedo A, Rittig S, Tekgul S, et al. Evaluation of and treatment for monosymptomatic enuresis: a standardization document from the International Children's Continence Society. J Urol. 2010. 183:441–447.
2. Butler RJ, Holland P, Gasson S, Norfolk S, Houghton L, Penney M. Exploring potential mechanisms in alarm treatment for primary nocturnal enuresis. Scand J Urol Nephrol. 2007. 41:407–413.
3. Butler RJ, Golding J, Heron J. ALSPAC Study Team. Nocturnal enuresis: a survey of parental coping strategies at 7 1/2 years. Child Care Health Dev. 2005. 31:659–667.
4. Jang WS, Cho JS, Kim JM, Hong CH. Application and treatment result of an enuresis alarm based on a questionnaire in children with enuresis? Korean J Urol. 2008. 49:745–752.
5. Hagglof B, Andren O, Bergstrom E, Marklund L, Wendelius M. Self-esteem before and after treatment in children with nocturnal enuresis and urinary incontinence. Scand J Urol Nephrol Suppl. 1997. 183:79–82.
6. Meydan EA, Civilibal M, Elevli M, Duru NS, Civilibal N. The quality of life of mothers of children with monosymptomatic enuresis nocturna. Int Urol Nephrol. 2012. 44:655–659.
7. Bower WF, Moore KH, Shepherd RB, Adams RD. The epidemiology of childhood enuresis in Australia. Br J Urol. 1996. 78:602–606.
8. Lee SD, Sohn DW, Lee JZ, Park NC, Chung MK. An epidemiological study of enuresis in Korean children. BJU Int. 2000. 85:869–873.
9. Shelov SP, Gundy J, Weiss JC, McIntire MS, Olness K, Staub HP, et al. Enuresis: a contrast of attitudes of parents and physicians. Pediatrics. 1981. 67:707–710.
10. Liu X, Sun Z, Uchiyama M, Li Y, Okawa M. Attaining nocturnal urinary control, nocturnal enuresis, and behavioral problems in Chinese children aged 6 through 16 years. J Am Acad Child Adolesc Psychiatry. 2000. 39:1557–1564.
11. Yeung CK, Sreedhar B, Sihoe JD, Sit FK, Lau J. Differences in characteristics of nocturnal enuresis between children and adolescents: a critical appraisal from a large epidemiological study. BJU Int. 2006. 97:1069–1073.
12. Redsell SA, Collier J. Bedwetting, behaviour and self-esteem: a review of the literature. Child Care Health Dev. 2001. 27:149–162.
13. Inan M, Tokuc B, Aydiner CY, Aksu B, Oner N, Basaran UN. Personal characteristics of enuretic children: an epidemiological study from South-East Europe. Urol Int. 2008. 81:47–53.
14. Khan AG, Shahid A, Memon AA. Prevalence of nocturnal enuresis in children: a community study. Pak J Med Res. 2009. 48:75–78.
15. Miskulin M, Miskulin I, Mujkic A, Dumic A, Puntaric D, Buljan V, et al. Enuresis in school children from eastern Croatia. Turk J Pediatr. 2010. 52:393–399.
16. Gunes A, Gunes G, Acik Y, Akilli A. The epidemiology and factors associated with nocturnal enuresis among boarding and daytime school children in southeast of Turkey: a cross sectional study. BMC Public Health. 2009. 9:357.
17. Foxman B, Valdez RB, Brook RH. Childhood enuresis: prevalence, perceived impact, and prescribed treatments. Pediatrics. 1986. 77:482–487.
18. Kanaheswari Y. Epidemiology of childhood nocturnal enuresis in Malaysia. J Paediatr Child Health. 2003. 39:118–123.
19. Ozkan S, Durukan E, Iseri E, Gurocak S, Maral I, Ali Bumin M. Prevalence and risk factors of monosymptomatic nocturnal enuresis in Turkish children. Indian J Urol. 2010. 26:200–205.
20. Hanafin S. Sociodemographic factors associated with nocturnal enuresis. Br J Nurs. 1998. 7:403–408.
21. Ozkan KU, Garipardic M, Toktamis A, Karabiber H, Sahinkanat T. Enuresis prevalence and accompanying factors in schoolchildren: a questionnaire study from southeast Anatolia. Urol Int. 2004. 73:149–155.
22. Robson WL. Clinical practice. Evaluation and management of enuresis. N Engl J Med. 2009. 360:1429–1436.
23. Moffatt ME, Harlos S, Kirshen AJ, Burd L. Desmopressin acetate and nocturnal enuresis: how much do we know? Pediatrics. 1993. 92:420–425.
24. Evans JH, Meadow SR. Desmopressin for bed wetting: length of treatment, vasopressin secretion, and response. Arch Dis Child. 1992. 67:184–188.
25. Ye JW, Lee SD. The comparison of therapeutic effect between imipramine and desmopressin on enuretic patients. Korean J Urol. 2001. 42:75–79.
26. Wille S. Comparison of desmopressin and enuresis alarm for nocturnal enuresis. Arch Dis Child. 1986. 61:30–33.
27. Kim WB, Kim KD. The epidemiology of childhood enuresis in Seoul and Kyunggi province. Korean J Urol. 1998. 39:1166–1170.
28. Cho SC, Kim JW, Shin MS, Hwang JW, Han SW, Park KH, et al. Behavioral and emotional problems in children with nocturnal enuresis: results of a multicenter study. J Korean Neuropsychiatr Assoc. 2005. 44:730–735.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download